GROSS ANATOMY
Ureters
- •
Muscular tubes (25-30 cm long) that carry urine from kidneys to bladder
- •
Course
- ○
In abdomen, retroperitoneal location
- –
Proximal ureters lie in perirenal space
- –
Mid ureters lie over psoas muscles slightly medial to tips of L2-L5 transverse process
- –
- ○
In pelvis, lie anterior to sacroiliac joints crossing common iliac artery bifurcation near pelvic brim
- –
Lie anterior to internal iliac vessels and course along pelvic sidewall
- –
At level of ischial spines, ureters curve anteromedially to enter bladder at level of seminal vesicles (men) or cervix (women)
- –
- ○
Ureterovesical junction (UVJ) : Ureters pass obliquely through muscular wall of bladder for ~ 2 cm
- –
Creates valve effect with bladder distension, preventing vesicoureteral reflux (VUR)
- –
- ○
- •
3 points of physiological narrowing
- ○
Ureteropelvic junction
- ○
Pelvic brim (crossing over common iliac artery)
- ○
UVJ
- ○
- •
Vessels, nerves, and lymphatics
- ○
Arterial branches are numerous and variable, arising from aorta and renal, gonadal, internal iliac, vesicle, and rectal arteries
- ○
Venous branches and lymphatics follow arteries with similar names
- ○
Innervation
- –
Autonomic from adjacent sympathetic and parasympathetic plexuses
- □
Responsible for ureteral peristalsis
- □
- –
Also carry pain (stretch) receptors
- □
Stone in abdominal ureter perceived as back and flank pain
- □
Stone in pelvic ureter may project to scrotum or labia
- □
- –
- ○
Lymphatics to external and internal iliac nodes (pelvic ureter), aortocaval nodes (abdomen)
- ○
Bladder
- •
Hollow, distensible viscus with strong, muscular wall and normal adult capacity of 300-600 mL of urine
- •
Lies in extraperitoneal (retroperitoneal) pelvis
- •
Peritoneum covers dome of bladder
- ○
Reflections of peritoneum form deep recesses in pelvic peritoneal cavity
- ○
Rectovesical pouch (between rectum and bladder) is most dependent recess in men (and in women following hysterectomy)
- ○
Vesicouterine pouch (between bladder and uterus) and rectouterine pouch of Douglas (between rectum and uterus)
- –
Rectouterine pouch most dependent in women
- –
- ○
- •
Bladder is surrounded by extraperitoneal fat and loose connective tissue
- ○
Perivesical space (contains bladder and urachus)
- ○
Prevesical or retropubic space (of Retzius) between bladder and symphysis pubis
- –
Communicates superiorly with infrarenal retroperitoneal compartment
- –
Communicates posteriorly with presacral space
- –
- ○
Spaces can expand to contain large amounts of fluid (as in extraperitoneal rupture of bladder and hemorrhage from pelvic fractures)
- ○
- •
Bladder wall composed mostly of detrusor muscle
- ○
Trigone of bladder: Triangular structure at base of bladder with apices marked by 2 ureteral orifices and internal urethral orifice
- ○
- •
Vessels, nerves, and lymphatics
- ○
Arteries from internal iliac
- –
Superior vesicle arteries and other branches of internal iliac arteries in both sexes
- –
- ○
Venous drainage
- –
Men: Vesicle and prostatic venous plexuses → internal iliac and internal vertebral veins
- –
Women: Vesicle and uterovaginal plexuses → internal iliac vein
- –
- ○
Autonomic innervation
- –
Parasympathetic from pelvic splanchnic and inferior hypogastric nerves (causes contraction of detrusor muscle and relaxation of internal urethral sphincter to permit emptying of bladder)
- –
Sensory fibers follow parasympathetic nerves
- –
- ○
IMAGING ANATOMY
Overview
- •
Normal ureters are small in caliber (2-8 mm) and are difficult to appreciate on ultrasound
- •
Fluid-distended urinary bladder is anechoic with posterior acoustic enhancement
- •
Urinary bladder changes in shape and position depending on intraluminal volume of urine
- ○
In its nondistended state, urinary bladder is retropubic in location, lying anterior to uterus in females and rectum in males
- ○
In markedly distended state, urinary bladder may occupy abdominopelvic area
- ○
Urinary bladder wall changes in thickness depending on state of distension of urinary bladder and is normally 3-5 mm in thickness
- ○
ANATOMY IMAGING ISSUES
Imaging Recommendations
- •
Transducer: Curvilinear 2-5 MHz
- •
Ureters
- ○
Ureters are normally not seen on ultrasound unless they are dilated; when dilated, overlying bowel gas may still limit ureteral evaluation in transabdominal approach
- –
Proximal dilated ureters may be well seen using kidney as window in coronal oblique plane
- –
Middle portion of dilated ureter may be identified in pediatric patients or thin adults using transabdominal approach
- –
Dilated terminal ureter/UVJ are seen best along posterolateral aspect of urinary bladder on transverse view
- □
Can also be evaluated by endovaginal sonography in women
- □
- –
- ○
Ureteral caliber may slightly increase as result of overfilled urinary bladder
- –
Distended bladder may cause ureteral and pelvicalyceal dilation, and rescanning post void is beneficial to exclude obstruction
- –
- ○
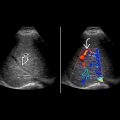
Color Doppler
- –
Assess ureteral jets; presence of jets helps exclude complete ureteral obstruction
- –
Look for twinkling artifact from obstructing stone
- –
- ○
- •
Bladder
- ○
Recommend fluid intake prior to examination to ensure optimal distension of urinary bladder
- –
In fully distended state, urinary bladder is easily visualized using transabdominal approach
- –
- ○
Examine patient in supine position with transabdominal suprapubic approach
- –
Perform scanning in sagittal and transverse planes
- –
Patient may be placed in decubitus position to determine mobility and differentiated intravesical masses from debris or stones
- –
With poor distention, caudal transducer angulation is needed to visualize urinary bladder in its retropubic location
- –
- ○
Nature of cystic structure in pelvis may be ascertained by asking patient to void or by inserting Foley catheter
- ○
Transvaginal ultrasound may be used in women for evaluation of suspect bladder neck lesions, UVJ stone, or ureterocele
- ○
Advantages of ultrasound
- –
Radiation-free, real-time assessment with high spatial resolution of bladder and bladder wall
- –
Real-time assessment of intraluminal masses in bladder for mobility and vascularity
- –
Real-time imaging guidance for bladder intervention, e.g., placement of percutaneous suprapubic catheters
- –
Real-time assessment of ureteral jets using color Doppler imaging; particularly useful in pregnant patients with dilated collecting system
- –
- ○
Imaging Pitfalls
- •
Reverberation artifacts are commonly encountered behind anterior wall of urinary bladder
- ○
Appear as regularly spaced lines at increasing depth as result of repeated reflection of ultrasound signals between highly reflective interfaces close to transducer
- ○
May be reduced or avoided by changing scanning angle or by moving transducer or using spacer
- ○
- •
Underdistended bladder may give false impression of wall thickening and limits intraluminal assessment
- ○
Have patient drink water and rescan with better distention
- ○
- •
Large midline ovarian or pelvic cystic mass may simulate bladder on transabdominal ultrasound
- ○
Attention to normal bladder shape, rescanning after voiding to confirm empty bladder, or transvaginal imaging is helpful to differentiate
- ○
CLINICAL IMPLICATIONS
Clinical Importance
- •
Ureters are at high risk of inadvertent injury during abdominal or gynecological surgery due to close proximity to uterine (in uterosacral ligament) and gonadal arteries (at pelvic brim)
- •
Ectopic ureter
- ○
Usually (80%) associated with complete ureteral duplication; more common in females
- ○
In complete duplication, upper moiety inserts ectopically inferiorly and distally to lower moiety ( Weigert-Meyer rule ) and can be associated with ureterocele
- –
Ureterocele may cause obstruction of upper pole moiety; also distorts UVJ of normally inserting lower pole moiety causing predisposition to VUR
- –
- ○
Ectopic ureteral insertion in females can occur in urethra or vagina, leading to urinary incontinence
- ○
- •
Ureterocele
- ○
Cystic dilation of intramural portion of ureter bulging into bladder
- –
Orthotopic: Normal insertion of single ureter
- –
Ectopic: Inserts below trigone, mostly in duplicated system
- –
- ○
- •
Ureteral duplication
- ○
Bifid ureter drains duplex kidney, but ureters unite before entering bladder
- ○
- •
Urachal anomalies
- ○
Patent fetal urachus forms conduit between umbilicus and bladder
- ○
Urachus is normally obliterated to form median umbilical ligament
- ○
May persist as cyst, diverticulum, or, rarely, fistula
- ○
Risk of infection or carcinoma (adenocarcinoma)
- ○
- •
Bladder diverticula are common
- ○
Congenital: Hutch diverticulum (near UVJ)
- ○
Acquired (usually due to chronic bladder outlet obstruction), associated with trabeculated bladder wall
- ○
Can lead to infection, stones, tumor
- ○
- •
Trauma
- ○
Extraperitoneal bladder rupture
- –
Urine and blood distend prevesical space (Retzius)
- –
Urine often tracks posteriorly into presacral space, superiorly into retroperitoneal abdomen
- –
High association with pelvic fractures
- –
- ○
Intraperitoneal bladder rupture
- –
Urine flows up paracolic gutters into peritoneal recesses and surrounds bowel
- –
Bladder ruptures along dome, which is in contact with intraperitoneal space
- –
Usually caused by blunt trauma to overdistended bladder
- –
- ○
URETERS AND URINARY BLADDER IN SITU