Urinary tract
Methods of imaging the urinary tract
1. Plain film radiography
2. Excretion urography (IVU)
3. Ultrasound (US)
4. Computed tomography (CT):
(a) CT for urological diagnosis and urological cancer staging
(b) CT for characterization of renal lesion
(c) CT adrenals
(d) CT KUB (kidneys, ureters, bladder)
(e) CT urography (CTU)
(f) CT angiography.
5. Magnetic resonance imaging (MRI):
(a) MR for characterization of renal lesion
(b) MR prostate
(c) MR bladder
(d) MR urography
(e) MR adrenals
(f) MR angiography.
6. Micturating cystography and cystourethrography
7. Ascending urethrography
8. Retrograde pyeloureterography
9. Percutaneous renal procedures:
(a) Biopsy
(b) Cyst puncture
(c) Antegrade pyelography
(d) Nephrostomy
(e) Percutaneous nephrolithotomy.
10. Arteriography
11. Venography
12. Conduitogram
13. Radionuclide imaging:
Plain film radiography
Intravenous excretion urography (IVU)
The technique is less frequently used than in the past and is now largely replaced by CT, MRI or US.
Contraindications
See Chapter 2 – general contraindications to intravenous (i.v.) water-soluble contrast media and ionizing radiation. In patients with contrast medium allergies alternative modalities such as ultrasound or MR can be considered. Patients with impaired renal function, particularly those with diabetes should be prepared with oral or intravenous hydration, or an alternative imaging modality considered. See Chapter 2.
Preliminary images
Supine, full-length anterior posterior (AP) of the abdomen, in inspiration. The lower border of the cassette is at the level of the symphysis pubis and the X-ray beam is centred in the mid-line at the level of the iliac crests.
If necessary, the location of overlying opacities may be further determined by:
• supine AP film of the renal areas, in expiration. The X-ray beam is centred in the mid-line at the level of the lower costal margin or
• 35° posterior oblique views (side of interest towards the film) or
• tomography of the kidneys.
The examination should not proceed further until these images have been reviewed by the radiologist or radiographer and deemed satisfactory.
Technique
Venous access is established. The gauge of the cannula/needle should allow the injection to be given rapidly as a bolus to maximize the density of the nephrogram.
Images
1. Immediate film. AP of the renal areas. This film is exposed 10–14 s after the injection (approximate ‘arm-to-kidney’ time). It aims to show the nephrogram at its most dense, i.e. the renal parenchyma opacified by contrast medium in the renal tubules. Tomography may assist in evaluation of the renal outline or possible masses (or ultrasound if subsequently available).
2. 5-min film. AP of the renal areas. This film gives an initial assessment of pathology – specifically the presence or absence of obstruction before administering compression.
A compression band is then applied positioned midway between the anterior superior iliac spines, i.e. precisely over the ureters as they cross the pelvic brim. The aim is to produce pelvicalyceal distension. Compression is contraindicated:
(a) after recent abdominal surgery
(b) after renal trauma
(c) if there is a large abdominal mass or aortic aneurysm
(d) when the 5-min film shows already distended calyces indicative of obstruction.
3. 10-min film. AP of the renal areas. There is usually adequate distension of the pelvicalyceal systems with opaque urine by this time. Compression is released when satisfactory demonstration of the pelvicalyceal system has been achieved. If the compression film is inadequate the compression should be checked and repositioned if necessary and a further 50 ml of contrast medium administered and the film after 5 minutes.
4. Release film. Supine AP abdomen taken immediately after release of compression. This film is taken to show the ureters. If this film is satisfactory, the patient is asked to empty their bladder.
5. After micturition film. Full-length supine AP abdomen. The aims of this film are to assess bladder emptying, to demonstrate drainage of the upper tracts, to aid the diagnosis of bladder tumours, to confirm ureterovesical junction calculi and, uncommonly, to demonstrate a urethral diverticulum in females.
Additional images
1. 35° posterior obliques of the kidneys, ureters or bladder – for equivocal collecting system lesions or localization of calculi.
2. Tomography – if renal outlines are not well seen.
3. Prone abdomen following the release film – may improve visualization of distal ureters by making them more dependent.
4. Delayed films at increasing (doubling of time intervals) up to 24 h after injection in renal obstruction.
Ultrasound of the urinary tract
Indications
1. Renal mass lesion
2. Renal parenchymal disease
3. Renal obstruction/loin pain
4. Haematuria
5. Hypertension
6. Renal cystic disease
7. Renal size measurement
8. Bladder outflow obstruction
9. Urinary tract infection
10. Bladder tumour
11. Following renal transplant:
12. To guide needle placement in interventional procedures
13. Renal vascular studies.
Patient preparation
Kidneys and bladder – prehydrate with oral fluids, e.g. 500–1000 ml 1 h before scan, patient attends with a full bladder. This may have the disadvantage of making the collecting systems appear mildly hydronephrotic pre-micturition.
Technique
1. Patient supine, right (RAO) and left anterior oblique (LAO) positions or lateral for kidneys. The kidneys are scanned longitudinally in an oblique coronal plane supplemented by transverse sections perpendicular to the axis. The right kidney may be scanned through the liver and posteriorly in the right loin. The left kidney is harder to visualize anteriorly, but can be visualized from a lateral approach. In difficult cases the patient should lie on their side with a pillow under the left loin to widen the space between the rib cage and pelvis.
2. The length of the kidney measured by US is 1–2 cm smaller than that measured at excretion urography because there is no geometric magnification. With US measurement, care must be taken to ensure that the true longitudinal lengthwise measurement is obtained. The range of lengths of the normal kidneys is 9–12 cm, and the difference between each kidney should be less than 1–2 cm.
3. The bladder is scanned suprapubically in transverse and longitudinal planes. Measurements taken of the three orthogonal diameters before and after micturition enable an approximate volume to be calculated by multiplying the three diameters and applying a conversion factor. (A conversion factor is usually pre-programmed into modern ultrasound machines.)
4. Renal transplants are usually located in the right or left iliac fossa. These usually lie fairly superficially and are easy to evaluate using oblique planes and gentle pressure to displace overlying bowel loops.
5. The native or transplant kidneys can be evaluated for vascular pathology using Doppler techniques.
• Renal artery stenosis is diagnosed by direct Doppler interrogation of the main renal arteries from a transabdominal approach. Elevated peak systolic velocities greater than 200 cm s–1 are suggestive of a >50% stenosis. Alternatively, as the main renal arteries in the native kidneys are often hard to visualize, the intrarenal arteries can be evaluated from a flank approach for downstream changes in waveform – the tardusparvus pattern;1 a slow rise (tardus) to a reduced peak (parvus) producing a prolonged acceleration time (a value >70 ms is indicative of a severe stenosis).
• Renal vein thrombosis is diagnosed by absent colour Doppler venous flow, direct visualization of thrombus within the distended vein, and a raised resistive index with reversal of arterial diastolic flow within the intrarenal arteries.
Reference
1. Kotval, PS. Doppler waveform parvus and tardus: a sign of proximal flow obstruction. J Ultrasound Med. 1989; 8:435–440.
Computed tomography of the urinary tract
Indications
1. Renal colic/renal stone disease
2. Renal tumour
3. Renal/perirenal collection
4. Loin mass
5. Staging and follow-up of renal, collecting system or prostatic cancer (local staging of prostatic cancer is performed using thin-section MRI)
6. Investigation of renal tract obstruction
7. CT angiography may be used to assess renal vessels for suspected renal artery stenosis or arterio-venous fistula or malformation.
Techniques
Standard diagnostic CT
This technique is used to stage and follow-up known renal-tract malignancy or to investigate non-specific signs attributed to the renal tract. Examination of the thorax in addition to the abdomen and pelvis is usually performed where pulmonary metastatic disease or mediastinal nodal spread is a possibility:
1. Venous access is obtained
2. Patient lies supine
3. Scanogram of chest, abdomen and pelvis as appropriate
4. 100 ml i.v. LOCM given
5. Scans obtained approximately 70 s (portal venous phase) after i.v. contrast (arterial phase scans of the liver (20–25 s after i.v. contrast) may be appropriate in those patients with suspected metastatic renal cancer who may have hypervascular liver metastases.)
Renal lesion characterization CT
This is used to assess renal cysts or masses identified on another imaging modality such as ultrasound.
Pre- and post-i.v. contrast scans are obtained through the kidneys in order to assess precontrast attenuation and subsequent enhancement patterns. Many practitioners advise the post-contrast scan be performed at 100 seconds (nephrographic phase) to prevent small intraparenchymal lesions being obscured by corticomedullary differentiation.
Adrenal lesion characterization CT
Indication: adrenal mass is suspected or needs characterization.
Technique: Unenhanced CT of the abdomen to enable measurement of attenuation of any adrenal mass.
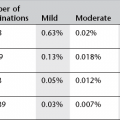
A value <10 HU is highly specific for a benign (lipid-rich) adenoma, and is often the only test required. This may, however, be supplemented when necessary by washout CT; re-measurement of the adrenal density in Hounsfield units at 15 min following i.v. contrast. Benign adenomas (whether or not lipid-rich) typically show rapid washout of contrast; an absolute percentage washout (APW) >60% or relative percentage washout (RPW) >40%, on delayed images, is highly specific for a benign lesion.
(Alternatively chemical shift MRI may be used for characterization.)
CT KUB
Plain CT (commonly referred to as CT KUB – kidneys, ureters, bladder) is useful to assess possible stone disease. It is used in many centres as the primary investigation of renal colic (replacing plain KUB radiograph):
1. No intravenous or oral contrast is given.
2. Patient supine. (Some authorities advise prone scanning to differentiate if stones are impacted at the vesicoureteric junction or have passed into the bladder.)
3. A low-radiation-dose technique is used to scan from the top of the kidneys to include the bladder base with a slice thickness of 5 mm or less, as determined by CT scanner. (Due to the low-dose nature of the scan and the absence of i.v. and oral contrast, the scan has a very limited role in identifying pathology other than renal tract calculus disease and should not be used indiscriminately for investigation of non-specific abdominal pain.)
CT urogram (CTU)
This technique uses a combination of unenhanced, nephrographic and delayed scans following i.v. contrast to sequentially allow examination of renal parenchyma and collecting systems.
1. An oral water load of 500–1000 ml 30–60 minutes before injection is recommended to ensure a diuresis and collecting system dilatation. No positive oral contrast
2. Patient supine
3. Initial low-dose unenhanced scans of urinary tract (CT KUB) to determine if renal tract calculus disease is present
4. Low osmolar contrast material (LOCM) 300 mg I ml–1 100 ml is given as bolus intravenously
5. Thin-section (usually 1 mm) scans are obtained from diaphragm to lower poles of kidneys during nephrographic/parenchymal enhancement phase (100 s following start of bolus injection). Alternatively, scan may instead be acquired during the portal venous phase (70 s) but normal corticomedullary differentiation may make small tumours difficult to appreciate
6. Delayed thin-section (1 mm) scans are acquired from upper pole of kidneys to bladder base 20 min after contrast injection, to examine collecting systems and ureters
7. Source images are reviewed along with multiplanar reconstructions. Post-processing with maximum-intensity projections and surface-shaded displays may be helpful, especially for demonstration.
Variations
The nephrographic phase may be omitted if the scan is specifically for urothelial tumour or collecting system assessment.
Some protocols use diuretics or use abdominal compression bands to achieve collecting system distension.
Radiation dose is a significant consideration for a triple-phase CTU (compared to an IVU) but newer iterative reconstruction techniques increasingly available are reducing the differential. Some authorities advocate the use of a split bolus technique, i.e. 50 ml of i.v. contrast 10–15 min before scanning, with a further 50 ml at the time of the scan, to achieve demonstration of the nephrographic and pyelographic phases with the same acquisition with consequent radiation dose saving.
CT angiography
Technique
1. No oral iodinated contrast used
2. Scan from the upper pole of the kidneys to the aortic bifurcation. Modern scanners are fast enough to produce high-quality studies of the whole abdomen
3. Narrow collimation (1 mm)
4. 100–150 ml i.v. contrast medium (LOCM 300) injected at 3–4 ml s–1
5. Use of bolus tracking/triggering devices or timing test injections is recommended to ensure appropriate timing. Otherwise scans are initiated after a preset empiric delay of 20–25 s from start of contrast material injection
6. Source axial scans are supplemented by multiplanar reconstructions and maximum intensity projection and volume-rendered surface-shaded display postprocessing.
Adrenal Lesion Characterization CT
Johnson, PT, Horton, KM, Fishman, EK. Adrenal imaging with multidetector CT: evidence-based protocol optimization and interpretive practice. RadioGraphics. 2009; 29:1319–1331.
Low, G, Dhliwayo, H, Lomas, DJ. Adrenal neoplasms. Clin Radiol. 2012; 67(10):988–1000.
O’Regan, KN, O’Connor, OJ, McLoughlin, P, et al. The role of imaging in the investigation of painless hematuria in adults. Semin Ultrasound, CT and MRI. 2009; 30(4):258–270.
Van Der Molen, AJ, Cowan, NC, Mueller-Lisse, UG, et al. CT urography working group of the European Society of Urogenital Radiology (ESUR). CT urography: definition, indications and techniques. A guideline for clinical practice. Eur Radiol. 2008; 18(1):4–17.
Magnetic resonance imaging of the urinary tract
Indications
1. Local staging of prostatic cancer
2. Local staging of bladder cancer
3. Staging of pelvic lymph nodes
4. Renal mass
5. Screening of patients with von Hippel–Lindau disease or their relatives, or other genetic conditions
6. MR urography where intravenous or CT urography contraindicated
7. MR angiography: potential living related donors, suspected renal artery stenosis.
Technique
Technique will be tailored to the clinical indication. MR of the kidneys and upper abdomen will generally include T1 and T2 weighted sequences in axial and coronal planes with or without fat saturation; with pre and post contrast T1 weighted imaging at 30 and 70 seconds. MRI of the abdomen and pelvis can be obtained to assess retroperitoneal lymphadenopathy as part of the staging investigations for patients with bladder and prostate cancer but CT is often used for this purpose with MRI reserved for local staging.
Magnetic resonance imaging of the prostate
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree