and Hossein Jadvar1
(1)
Department of Radiology, Keck School of Medicine, University of Southern California, Los Angeles, CA, USA
Prostate Cancer
Case 8.1
History
A 60-year-old Caucasian male with castrate-resistant metastatic adenocarcinoma of prostate, status post radical prostatectomy (Gleason score 4 + 5) and androgen ablation therapy.
Findings
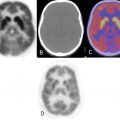
FDG PET-CT scan performed 4 months after the baseline showed an interval increase in extent and degree of hypermetabolism diffusely throughout both hepatic lobes with maximum SUV of 9.1 (Fig. 8.1). There is also an interval increase in number and size of diffuse pulmonary nodules. Patient died from disseminated disease 2 months later.


Fig. 8.1
Impression
Interval progression of metastatic disease.
Case 8.2
History
A 55-year-old male with history of end-stage renal disease and metastatic prostate cancer, initially diagnosed in June 2005, status post radiation treatment and currently on Casodex and monthly Lupron.
Findings
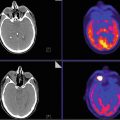
There has been an interval increase in the size and metabolic activity of previously seen mesenteric, retroperitoneal, and right common iliac lymph nodes (Fig. 8.2). For example, the hypermetabolic left para-aortic lymph nodes, at L2 level, now have a maximum SUV of 2.7 (from 2.1). A newly apparent, hypermetabolic left supraclavicular lymph node has a SUVmax of 3.0 and measures 1.5 cm × 2.9 cm. There has also been an interval increase in the intensity and extent of previously seen hypermetabolic osseous lesions.


Fig. 8.2
Impression
Progressive retroperitoneal, left supraclavicular lymphadenopathy, and osseous metastatic disease.
Case 8.3
History
A 63-year-old male with castrate-resistant metastatic prostate cancer (primary Gleason score 4 + 5).
Findings
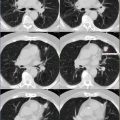
Serial FDG PET-CT scans showed that the lesions’ metabolic activity, as depicted by SUVmax, kept on decreasing showing a good response to therapy and was also correlated with decline in PSA values, but the CT density, as depicted by HU (Hounsfield unit), continued to increase (Fig. 8.3).


Fig. 8.3
Impression
Metabolic activity of metastatic osseous lesions tends to decrease, while CT density tends to increase with successful therapy.
Case 8.4
History
An 86-year-old male, recently diagnosed with small cell carcinoma of the prostate gland. PET-CT is done as part of the initial treatment strategy evaluation.
Findings
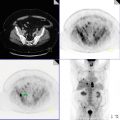
The prostate gland is extensively bulky with areas of calcification (Fig. 8.4). Intense metabolic activity is seen at the right posterior and central aspect of prostate (SUVmax 11.2), compatible with known primary neoplasm. The prostate tumor appears to encroach the urethra with no fat plane identified between the prostate tumor and anterior wall of the rectum posteriorly or the urinary bladder anteriorly. There are several hypermetabolic bilateral external and internal iliac and presacral/perirectal lymph nodes, compatible with metastatic disease. The highest level of FDG-avid lymph node is seen at the level of left proximal external iliac bifurcation, involving the left external iliac lymph node, measuring approximately 2.7 cm in long axis with SUVmax 13.3. The largest hypermetabolic right external iliac lymph node measures approximately 2.6 cm long axis with SUVmax 14.6. Two hypermetabolic presacral lymph nodes are seen: one in the midline shows SUVmax 7.0, and the left paramedian presacral lymph node shows SUVmax 9.4. A right perirectal lymph node at the level of S4 shows SUVmax 13.1.


Fig. 8.4
Impression
Hypermetabolic, large, bulky tumor involving right and central posterior aspect of prostate with hypermetabolic, metastatic bilateral internal and external iliac and perirectal/presacral lymphadenopathy.
Pearls and Pitfalls
FDG PET may be useful for detecting, staging, and restaging poorly differentiated, hypoxic, high Gleason score tumors, monitoring treatment response in metastatic disease, assessment of extent of metabolically active castrate-resistant disease, and prognostication.
FDG PET-CT has limited utility to differentiate between primary prostate cancer vs. BPH and post-op scarring and in patients with local recurrence after primary therapy.
Higher FDG uptake with higher Gleason grade, advanced clinical stage, and higher serum PSA levels.
Conventional morphologic (CT) and functional (99m Tc-MDP bone scintigraphy) imaging methods for qualitative treatment response assessment of bone metastases have been inaccurate and pose a challenge in routine oncological practice and in clinical trials, as skeletal lesions have been considered as nonmeasurable disease [2].
Discussion
Prostate cancer is the most common CA (30 % of all male CA) and second leading cause of CA death in men (exceeded by lung cancer) [1]. Incidence of adenocarcinoma is much higher than sarcoma and transitional cell carcinoma of the prostate. Routine diagnostic tests include digital rectal examination (DRE), PAP and PSA (nonspecific), and Gleason score (min 2, max 10). PSA and DRE have a limited positive predictive value. Imaging modalities currently in use are ultrasonography (standard gray scale, enhanced transrectal with contrast agents, color and power Doppler, elastrography), computed tomography (CT), MRI (endorectal probe, contrast, spectroscopic imaging, lymphotropic nanoparticles, DWI), scintigraphy (bone scan, radioimmunoscintigraphy—Prostascint ™), and positron emission tomography (PET), PET-CT, and PET-MRI.
Prostate cancer is biologically and clinically a heterogeneous disease, and its imaging evaluation needs to be tailored to the specific phases of the disease in a patient-specific, risk-adapted manner. Within 10 years after successful treatment for localized disease, 15–40 % experience PSA rise which is termed as biochemical recurrence. About 25–35 % of men with an increasing serum PSA level will develop locally recurrent disease only, 20–25 % will develop metastatic disease only, and 45–55 % will develop both local recurrence and metastatic disease. Median survival time for patients detected with metastatic disease is around 5 years, while the medial survival is only 8–18 months for those who have become refractory to hormonal therapy. As shown in Case 1, the patient had developed castrate-resistant metastatic prostate cancer and died 2 months after his 4-month scan due to disease progression.
Bone is the most common site to which prostate cancer metastasizes. Response to treatment is typically estimated by using a combination of methods, including diagnostic imaging, measurement of biochemical markers, and evaluation of patients’ symptoms. Three patterns of bone metastasis commonly noted depending on the stage of treatment are (a) FDG uptake without corresponding morphological changes on CT; (b) FDG uptake with concomitant morphological changes on CT as sclerotic, lytic, and/or mixed lesions; and (c) negative FDG PET but dense sclerosis on CT. Metabolic and anatomic details provided by the combined PET-CT may provide a good imaging tool for quantitatively assessing response of metastatic skeletal lesions to various forms of systemic therapy.
Several novel PET tracers which are being tested for use in prostate cancer are radiolabeled acetate (11C, 18F), choline (11C, 18F), 11C-methionine, dihydrotestosterone (18F-FDHT), anti-1-amino-3-18F-fluorocyclobutane-1-carboxylic acid (anti-18F-FACBC), 1-(2′-deoxy-2′-fluoro-b-d-arabinofuranosyl)thymidine (18F-FMAU), and [18F]DCFBC (PSMA inhibitor) [12, 14, 15].
Bladder Cancer
Case 8.5
History
A 68-year-old male with high-grade urothelial carcinoma primary involving his kidney and bladder with metastasis in the retroperitoneum and liver, status post open nephroureterectomy with excision of the bladder cuff and left pelvic lymph node dissection and chemotherapy. Scan is being done for restaging.
Findings
Interval progression of hepatic disease now pan lobar with interval increase in extent of right hepatic confluent metastatic disease with new active left hepatic lobe lesions (Fig. 8.5). The confluent disease in the right correlates to low attenuation and now measures 9.8 × 9.2 × 10.4 cm, with SUVmax 25.1 (9 × 6.6 × 4.1 cm with SUVmax 23.1 in prior). There is an interval increase in size and activity of portacaval nodes now with SUVmax 14.1 (right 13.5 in prior). Also noted is a new hypermetabolic gastroduodenal (SUVmax 16) celiac axis node which is normal sized. There are also new multiple retroperitoneal hypermetabolic nodes, for example, aortocaval nodes with SUVmax up to 8.9. Interval increase is seen in the extent of left anterior pillar of acetabulum medullary sclerosis with stable metabolic activity, now involving superior pubic ramus, with SUVmax 10.6 (SUVmax 9.8 in prior).