TERMINOLOGY
Abbreviations
- •
Vaginal artery (VA), uterine artery (UA)
GROSS ANATOMY
Overview
- •
Muscular tube formed by smooth muscle and elastic connective fibers
- •
Serves as excretory duct for uterus, female organ for copulation, and part of birth canal
- •
Extends up and back from vestibule of external genitalia to surround cervix of uterus
- •
Has anterior and posterior walls, normally in apposition, with longer posterior wall
- •
Superiorly, cervix projects downward and backward into vagina and divides vagina into shallow anterior, deep posterior, and lateral fornices
- •
Upper 1/2 of vagina lies above pelvic floor, lower 1/2 lies within perineum
- •
Lined with stratified squamous epithelium
- •
Inner mucosal surface of wall form rugae when collapsed
- •
Thin mucosal fold called hymen surrounds entrance to vaginal orifice
- •
Outer surface (adventitial coat) is thin fibrous layer continuous with surrounding endopelvic fascia
- •
Vasculature
- ○
Arterial supply
- –
VA: Can branch directly from internal iliac artery (anterior trunk) or sometimes from inferior vesical artery or UA
- –
Vaginal branches of UA
- –
Branches of VA and UA anastomose to form 2 median longitudinal vessels: Azygos arteries, 1 in front and 1 behind vagina
- –
- ○
Venous drainage
- –
Form venous plexus around vagina
- –
Eventually drains to internal iliac veins
- –
- ○
- •
Variations with age
- ○
Menarche: 7-10 cm long
- ○
Postmenopausal: Shrinks in length and diameter; fornices virtually disappear
- ○
Anatomic Relationships
- •
Anterior
- ○
Superior: Bladder base
- ○
Inferior: Urethra
- ○
- •
Posterior
- ○
Upper 1/3: Rectouterine pouch of Douglas
- ○
Middle 1/3: Ampulla of rectum
- ○
Lower 1/3: Perineal body
- ○
- •
Lateral
- ○
Upper 1/3: Ureters
- ○
Middle 1/3: Levator ani and pelvic fascia
- ○
Lower 1/3: Bulb of vestibule, urogenital diaphragm, and bulbospongiosus muscles
- ○
- •
Ligamentous supports
- ○
Upper 1/3: Levator ani muscles, transverse cervical (cardinal), pubocervical, and sacrocervical ligaments
- ○
Middle 1/3: Urogenital diaphragm
- ○
Lower 1/3: Perineal body
- ○
IMAGING ANATOMY
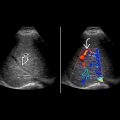
Ultrasound
- •
Transabdominal US with distended bladder is standard imaging technique
- ○
Caudal angulation on both longitudinal and transverse scans
- ○
Commonly found at/near sagittal midline of pelvis
- ○
Length and wall thickness vary in response to bladder and rectal filling
- ○
Combined thickness of anterior and posterior vaginal walls should not exceed 1 cm for transabdominal scan with distended bladder
- ○
Characteristic appearance of 3 parallel lines
- –
Highly echogenic mucosa centrally, may be difficult to visualize if stretched by distended bladder
- –
Moderately hypoechoic muscular walls
- –
- ○
- •
Transperineal US with nondistended bladder for assessment of uterine prolapse or for difficult cases
- ○
Vagina, especially vaginal canal, is less well defined
- ○
- •
Transvaginal US may require withdrawal of transducer so as not to compress pathology
EMBRYOLOGY
Embryologic Events
- •
Uterus and upper vagina are formed from paired müllerian (paramesonephric) ducts
- •
Paired ducts meet in midline and fuse, forming uterovaginal canal
- •
Lower vagina is formed from urogenital sinus
CLINICAL IMPLICATIONS
Uterine Prolapse
- •
Ligamentous support of pelvic organs may be damaged or become lax, leading to uterine prolapse or prolapse of vaginal walls
- •
Cystocele: Sagging of bladder with bulging of anterior vaginal wall
- •
Rectocele: Sagging of ampulla of rectum with bulging of posterior vaginal wall
- •
Best to be investigated by transperineal US supplemented with 3D
Müllerian Duct Anomalies
- •
Failure of müllerian duct development ± fusion
- •
Vagina most commonly affected in uterus didelphys (class III anomaly); vaginal septum seen in ~ 75% of cases
- •
Hematocolpos from imperforate hymen or vaginal septum may be evaluated by transperineal US
Pelvic Abscess
- •
Common site: Rectouterine pouch of Douglas
- •
Transvaginal approach allows US-guided drainage of pelvic abscess without surgery
Infertility
- •
Transvaginal US is used for egg retrieval in assisted reproduction
Persistent Sexual Arousal Syndrome
- •
Persistent sexual arousal during sleep in postmenopausal women
- •
VA blood flow as 1 diagnostic aid
- •
VA normally shows high-resistance flow
- •
During sexual arousal, increased blood flow to VA with low-resistance spectral waveform
VAGINA IN SITU AND ARTERIAL SUPPLY