KEY POINTS
Ventriculomegaly is not a diagnosis. It is a sign. The search for all underlying causes should be immediately undertaken.
Ventriculomegaly is frequently associated with a large number of intra- and extracranial chromosomal as well as nonchromosomal anomalies.
For measuring the lateral ventricle it is recommended to use an axial view of the brain and to place the clipers at the level of the parieto-occipital fissure that is usually well demonstrated from 20 weeks’ gestation.
Congenital ventriculomegaly has a increased recurrence rate and after the birth of an affected infant a targeted neurscan is recommended in a subsequent pregnancy.
Ventriculomegaly, a term commonly employed to indicate the enlargement of the lateral cerebral ventricles, is found in ~1% of fetuses at midgestation and is the most common abnormal fetal cerebral diagnosis.
Although the enlargement of the lateral ventricles encompasses a wide spectrum of severity, at present a width of the atrium <10 mm is considered normal, 10 to 15 mm indicates mild ventriculomegaly, and >15 mm represents severe ventriculomegaly. This categorization has prognostic implications. Fetuses with normal ventricles have an exceedingly low risk of cerebral anomalies. Fetuses with mild ventriculomegaly in the majority of cases are normal at birth but have an increased risk of an abnormal outcome. Fetuses with severe ventriculomegaly have a very high probability of an abnormal outcome.
Enlargement of the cerebral lateral ventricles is not an anomaly per se. The clinical significance of this finding is that it signals to the possibility of associated anomalies of the brain or other organs. The final prognosis depends more on such anomalies than on the degree of ventricular dilation.
Fetuses with mild ventriculomegaly in particular have an increased risk of chromosomal aberrations.
Mild hydrocephaly, borderline ventriculomegaly
The widely accepted definition of mild cerebral lateral ventriculomegaly is an atrial width of 10 to 15 mm on the transverse plane (Figure 4–1)1,2,3
Seen in 1% of fetuses4
In many cases, it probably represents a normal variant. In other cases, mild enlargement of the lateral ventricles may be the only obvious epiphenomenon of heterogeneous cerebral anomalies.
Isolated mild ventriculomegaly should be differentiated from more complex abnormalities of the fetal brain that frequently have a different prognosis (eg, agenesis of the corpus callosum and cortical malformations). Several reports suggest that magnetic resonance imaging (MRI) may be a useful adjunct to sonography, particularly in late gestation.5,6
The main problem in cases that are referred with mild dilatation of the lateral ventricles is to exclude other neural and extraneural malformations. We recommend careful multiplanar examination of the fetal brain, performed if possible with a high-resolution vaginal probe, and a detailed evaluation of the spine. Both lateral ventricles should be visualized and assessed, as this condition can be unilateral (Figure 4–2). A stepwise ultrasound (US) evaluation of the fetal brain should be performed in order to exclude associated anomalies (Figure 4–3). Although the use of MRI has also been advocated,5,6 we believe that when following the protocol suggested in Figure 4–3, the role of fetal MRI remains limited to those cases in which technical issues impairs US visualization. A detailed evaluation of the entire fetal anatomy, including fetal echocardiography, should also be performed. These examinations may be incomplete or limited during the third trimester.
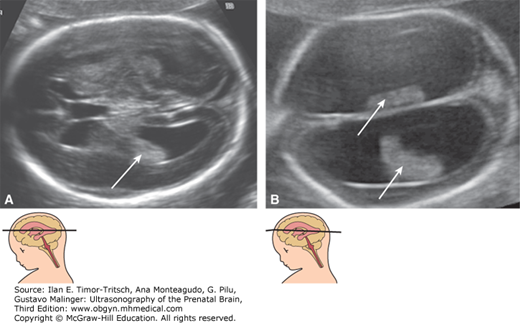
Figure 4–2.
(A) Unilateral ventriculomegaly. The calcarine fissure (arrows) is significantly less pronounced in the ventriculomegalic hemisphere than in the controlateral one. (B) Bilateral ventriculomegaly. The calcarine fissure is not seen in this image, even though it was obtained at 21 weeks. A delayed cortical maturation is frequently encountered with ventriculomegaly. The clinical significance of such finding is uncertain. Both of these fetuses had a completely normal outcome and normal neurologic development at long-term follow-up.

Figure 4–3.
Flowchart for the investigation of fetuses with mild bilateral ventriculomegaly. Ventriculomegaly may be present with any congenital or acquired brain anomaly. Isolated mild ventriculomegaly may be diagnosed only after exclusion of these central nervous system anomalies. ONTD, open neural tube defects (Chapter 5); DWC, Dandy-Walker complex (Chapter 8); HPE, holoprosencephaly (Chapter 6); ACC, agenesis of the corpus callosum (Chapter 6); MCD, malformations of cortical development (Chapter 7); IVH, intraventricular hemorrhage (Chapter 12); HC, head circumference.

In all standard sonographic examinations, a view of the lateral ventricles should be obtained, and at least one of the atria should be visualized and assessed. A qualitative -evaluation is acceptable, and the presence of the choroid plexus filling the cavity of the atrium, being closely apposed to both the medial and lateral walls of the ventricle, is indicative of normalcy. A quantitative approach, however, is favored, and a measurement <10 mm is considered normal between 15 and 40 weeks.7 Congenital ventriculomegaly may develop late in gestation, and a normal midtrimester exam does not exclude this condition. The correct measurement of the lateral ventricles is important to avoid false-positive diagnoses of ventriculomegaly. Common errors in measurement include placing the calipers in the brain parenchyma instead of at the inner border of the ventricular wall, measuring the ventricle not perpendicular to their walls, measuring the occipital horn, or measuring the lateral ventricle not in a truly axial plane. A specific approach has been described that proposes placing the calipers at the level of the parietooccipital fissure, an easily recognizable landmark beginning around 20 weeks’ gestation8 (Figure 4–4).
Figure 4–4.
Pitfalls in the measurement of the lateral ventricle. (A) Axial plane. The correct measurement of the lateral ventricular width (LVW) is numbered 1. The measurements depicted as 2 and 3 are wrong; 2 is positioned in the occipital horn, and 3 measures not only the ventricles but also part of the brain parenchyma. (B) This image shows a common error in measuring the proximal lateral ventricle. The proximal ventricle is difficult to visualize in a true axial plane, and the operator tilted the transducer to reach access to show the proximal ventricle. This plane shows a poorly visualized ventricle in an oblique plane, and measurement 4 overestimates the LVW.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree