Fig. 4.1
Normal water enema multidetector CT (WE-MDCT) examination in a 55-year-old woman with unspecific abdominal complaints, requested to investigate clinical suspicion of diverticulitis. Image review along coronal and axial planes allows assessing all well-distended segments of the large bowel, with optimal contrast between the perivisceral fat, thin enhanced colonic wall and hypodense lumen. No non-distended segments, mural thickening or intraluminal vegetations are observed. Faecal residues are absent following standard bowel preparation. Note rectal tube in (a)
Potential pitfalls of the technique are mostly represented by non-distended bowel segments, and by the presence of fecal residues, which is the rule when bowel preparation is limited or avoided. Whereas other authors have reported a 95 % sensitivity and specificity for the detection of CRC in unclean bowel, in our experience endoluminal stools usually do not hamper a correct assessment of the colonic wall thickness and enhancement pattern, but sub-centimeter polyps and fine mural details characteristic of UC may be obscured [4, 11, 14].
4.3 Water Enema Multidetector CT in Ulcerative Colitis
4.3.1 Mural WE-MDCT Findings
Pathologically, UC is characterized by extensive mucosal ulceration and diffuse non-granulomatous inflammation that usually commences in the rectum and extends proximally in a continuous, confluent and concentric manner to affect a variable entity of the large bowel.
Historically, CT had a limited role in imaging patients with UC, because of its low sensitivity for endoscopically detected early disease changes [7, 19].
However, despite being primarily a mucosal disease, UC is commonly characterized by mural colon thickening. Therefore, with its intrinsic optimal spatial resolution, tissue contrast, luminal and mural distension, WE-MDCT may usefully complement OC to assess the colonic wall in its full-thickness, as well as mesenteric and extraintestinal changes. Early superficial and flat mucosal changes observed at OC, such as granulation due to oedema, hyperemia and increased mucin secretion, remain below the high resolution power of MDCT [7, 18].
In patients with UC, WE-MDCT allows an easy identification of the transition between the involved large bowel which is not completely distended despite pharmacological hypotonisation, and the upstream spared segments that usually appear well distended with recognizable haustral folds. Most usually, UC changes show a continuous distribution from the rectum (which is spared in 4 % of cases only) to the left-sided or the entire colon (Figs. 4.2, 4.3 and 4.4). In UC, colon wall thickening is usually of moderate entity (6−9 mm), circumferential and symmetric in the majority of cases. In the only series that investigated the role of MDCT in UC, wall thickening was positively associated with endoscopic, clinical and histopathological severity [4, 18].
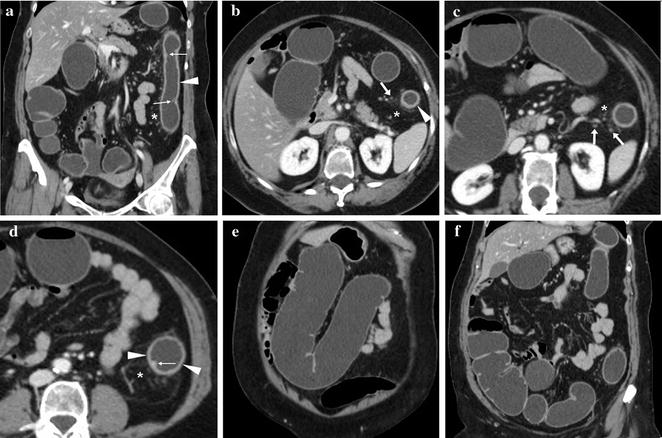
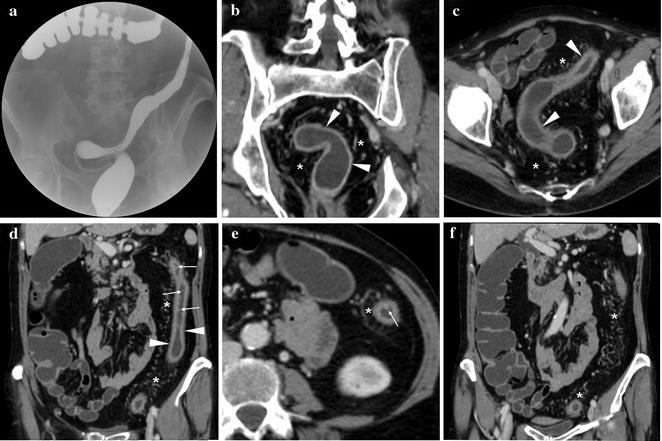
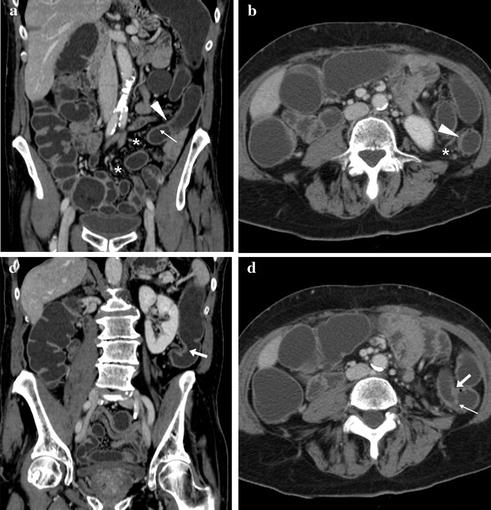
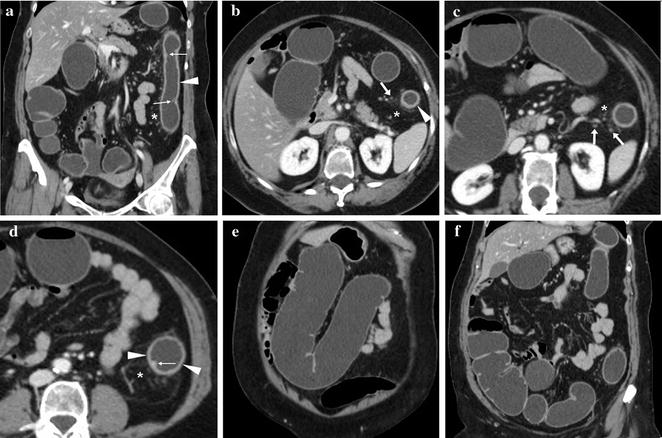
Fig. 4.2
63-year-old female with ulcerative colitis. Elective WE-MDCT shows moderate, uniform mural thickening throughout the descending colon (arrowheads) with tiny endoluminal projections corresponding to endoscopic finding of pseudopolyps (thin arrows). The proliferating pericolonic fat shows increased density and vascularity (*) with some tiny lymph nodes (arrows). The upstream transverse and right colon is well distended with preserved haustra (Reprinted from Open Access Ref. [4])
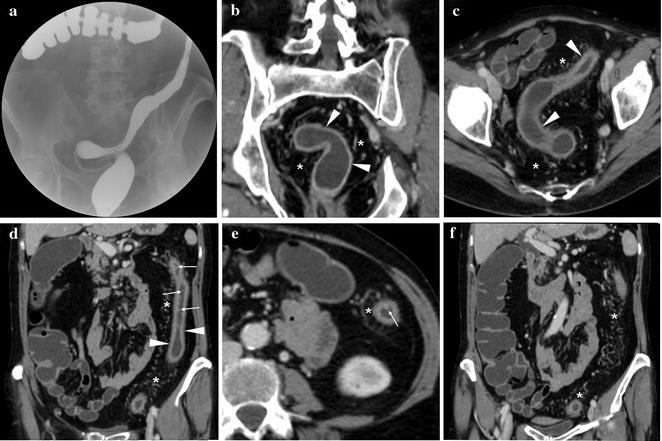
Fig. 4.3
65-year-old female with ulcerative colitis, initially investigated with water-soluble contrast enema shows “water-pipe” appearance of shortened, narrow left colon with advanced haustral loss (a). After medical treatment, elective WE-MDCT was performed because of incomplete colonoscopy. Discrete, circumferential mural thickening is observed from the rectum to the splenic flexure (arrowheads), corresponding to endoscopic severe disease, with confirmation of several millimetric pseudopolyps (thin arrows) throughout the descending tract. Markedly increased vascularity is seen in the proliferating perirectal and pericolonic fat planes (*). Most of the transverse and right colon appear to be spared (Reprinted from Open Access Ref. [4])
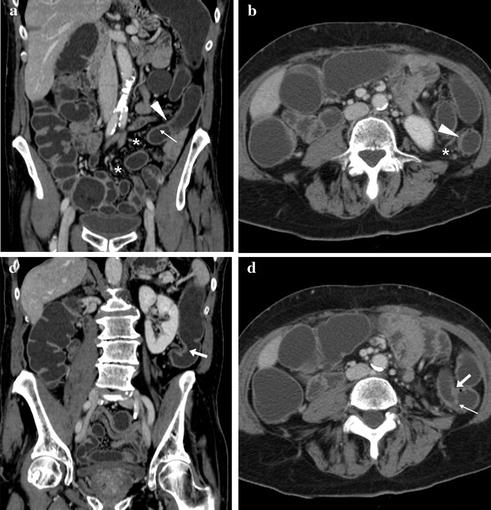
Fig. 4.4
63-year-old male with ulcerative colonoscopy and endoscopy limited to 45 cm from the anal verge because of non-distensible colon with diffuse mucosal changes and pseudopolyps. Elective WE-MDCT shows moderate mural thickening throughout the rectosigmoid and descending tract consistent with left-sided colitis (arrowheads) and associated pericolonic fat changes (*). In the proximal descending colon, a focal substenosis with asymmetric mural thickening (arrows) and pseudopolyps (thin arrow) is detected, prompting endoscopic and bioptic re-evaluation, that allowed to exclude carcinoma and dysplasia. Fair distension of the transverse and right colon with preserved mural thickness and haustra (Reprinted from Open Access Ref. [4])
Whereas WE-MDCT findings observed in active UC phases are discussed in Chap. 6 dealing with acute UC manifestations of this book, with disease progression mucosal ulceration and denudation leading to the formation of inflammatory pseudopolyps, which can be visualized at WE-MDCT as tiny solid endoluminal projections (Figs. 4.2, 4.3 and 4.4). In subacute and chronic phases of UC, the characteristic marked hypertrophy of the muscularis mucosa and transmural fibrosis produces diffuse, uniform mural thickening, reduced distension and shortening of the involved colon, segmental or diffuse luminal narrowing (Figs. 4.2, 4.3 and 4.4) [4, 7, 18, 19].
4.3.2 Proposed Indications for WE-MDCT in Ulcerative Colitis
According to the above-cited current clinical guidelines, indications for CT in UC should be limited to cases of impossible or incomplete OC (Figs. 4.3, 4.4), and impassable stenosis. Due to the substantial CRC risk, the endoscopic detection of a colonic stricture in UC warrants further imaging investigation with WE-MDCT, to assess both its features and the upstream colon (Fig. 4.4) [4, 8].
Furthermore, in our experience selected patients with UC and incomplete endoscopy may benefit from WE-MDCT to determine the longitudinal disease extent. In fact, the distribution of UC according to the Montreal criteria as proctitis, left-sided (distal to the splenic flexure) or extensive colitis (including pancolitis) influences patient management (particularly the choice of drug delivery system), dictates CRC risk and therefore the start and frequency of periodic surveillance [4, 9, 10, 20].
4.3.3 Perivisceral WE-MDCT Findings
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree