In the rapidly changing, accelerated world of radiology, technology has revolutionized how patient data is recorded, shared, and stored. While boosting unparalleled efficiency and accuracy in diagnosis and therapy, it raises severe issues concerning data security and privacy. At the forefront of these concerns is HIPAA:the Health Insurance Portability and Accountability Act, a regulatory tool that protects patient information of a sensitive nature.
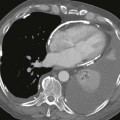
HIPAA compliance offers radiologists more than just a legal framework—it provides a clear structure for safeguarding patient information, which ultimately strengthens the quality of care. By adhering to HIPAA standards, radiology professionals can ensure that patient data is handled securely and consistently, reducing the risk of breaches or unauthorized access. This not only protects individuals’ privacy but also enhances the reputation and reliability of the healthcare institution. When patients know their sensitive imaging data—whether from MRI scans, CT images, or ultrasound reports—is protected under strict guidelines, it builds confidence and encourages more open, accurate communication during diagnosis and treatment.
Understanding the Stakes in Radiology
Radiology departments handle some of the most data-intensive workflows in medicine. From transmitting DICOM images to archiving large volumes of patient records, the digital ecosystem is vast and interconnected. This complexity makes radiology especially vulnerable to data breaches. A single unsecured file transfer or an improperly configured cloud storage system can put thousands of patient records at risk.
HIPAA’s Security Rule mandates administrative, physical, and technical safeguards to ensure the confidentiality, integrity, and availability of electronic PHI (ePHI). For radiology practices, this means implementing robust encryption, secure PACS systems, and role-based access controls. It also involves regular staff training, so that everyone from radiologists to IT personnel understands how to handle data responsibly.
Common Compliance Pitfalls to Avoid
Despite the best intentions, lapses still happen. One common issue is the use of unsecured mobile devices or personal email to share patient images. Even seemingly minor actions like discussing patient cases in public areas can lead to violations.
Another risk area is third-party vendors. Many radiology practices outsource billing, cloud storage, or AI tools. Under HIPAA, any business associate with access to PHI must also be compliant. This makes it essential to vet partners carefully and sign proper Business Associate Agreements (BAAs).
The Role of AI and Presentations
As artificial intelligence becomes more integrated into radiology from aiding diagnoses to automating report generation questions about compliance grow more nuanced. Even tools leveraging AI for presentation purposes, such as enhancing educational materials or creating case summaries, must be carefully evaluated to ensure they handle anonymized data responsibly. While these technologies can significantly improve communication and learning, they must still operate within the bounds of HIPAA to protect patient privacy. For example, generating a slide deck for a tumor board meeting using AI-enhanced imaging must still meet HIPAA standards if it includes patient information.
Conclusion: Building a Culture of Compliance
Ultimately, HIPAA compliance is not a checklist, it’s a mindset. In radiology, where innovation moves fast and data is abundant, fostering a culture of security and respect for patient privacy is key. By embedding compliance into every workflow and staying informed about emerging technologies, radiology professionals can ensure that their work remains both cutting-edge and ethically grounded.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree