Ankle Joint and Forefoot
Anatomy and Techniques
Introduction
Position 1: Medial Ankle Proximal
Technique
The examination begins with the probe in an axial position just above the medial malleolus (Fig. 23.1). The posteromedial margin of the tibia is easily identified and the largest and most medial of the tendons is the TPT. Deep to the TPT, a low-reflective band overlies the tibial cortex representing the hyaline cartilage of a pulley enthesis. This assists with the smooth passage of the tendon around the malleolus. The presence of cartilage at this location explains why enthesopathy can occur and why bony spur formation is a component of patients with chronic TPT disease. The tendon should have a normal internal structure comprising areas of low reflectivity, representing the tendon fibres interspaced with areas of increased reflectivity from the intervening connective tissue support structures. The most medial aspect of the tendon is in line with the medial border of the tibia.
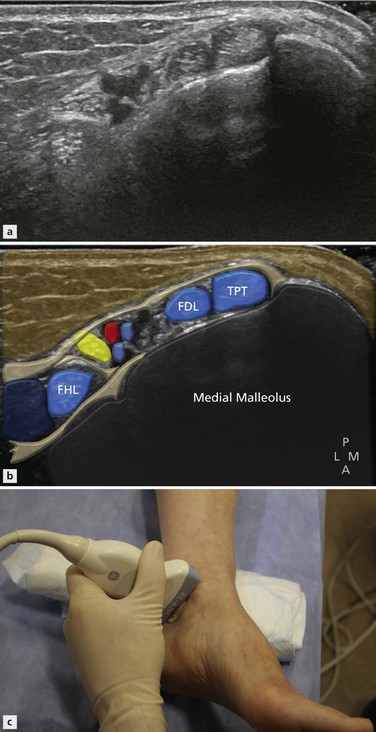
Figure 23.1 The ultrasound transducer is positioned in the axial plane posterior to the medial malleolus, demonstrating the three medial tendons and the tibial neurovascular bundle.
Lying along the lateral margin of tibialis posterior in close proximity with it is the tendon of flexor digitorum longus (FDL). This is a much smaller tendon than TPT with a lower musculotendinous junction. The other structures in the proximal part of the tarsal tunnel include the posterior tibial artery and veins. The medial border of the posterior subtalar joint is identified deep to the flexor digitorum tendon as it passes below the sustentaculum. Immediately lateral to this is the tibial neurovascular bundle. The posterior tibial artery and its multiple surrounding veins separate flexor digitorum from the tibial nerve. The tibial nerve is a brighter, more reflective structure than the nearby tendons. Once again low-signal elements can be identified within it, representing the neural bundles, and these are separated by intensely bright components representing epineural tissue. The tibial nerve divides to form the medial and lateral plantar nerves. This branching can occur at any point and may already have occurred at the level of the medial malleolus. A smaller branch, the medial calcaneal nerve, arises directly from the tibial nerve and can be seen deep and slightly posterior as it heads towards the posterior medial corner of the os calcis. Another important branch, the inferior calcaneal nerve, arises from the lateral plantar nerve. It is sometimes referred to as the first branch lateral plantar nerve. This nerve also passes deep and somewhat posteriorly to pass around the underside of the hind foot close to the origin of the plantar fascia. It traverses the hind foot to supply abductor digiti minimi. This nerve may be impinged by plantar fasciitis, leading to atrophy of the aforementioned muscle. Compression of the nerve more proximally may also lead to a syndrome that mimics plantar fasciitis, called Baxter’s neuropathy.
Position 2: Medial Ankle Distal
Technique
As the probe is advanced distally following tibialis posterior, the medial malleolus disappears from view. The structure which now is found deep to TPT is the tibiotalar ligament, a major component of the deltoid ligament complex (Fig. 23.2). This ligament is said to have two components, although the posterior component is more dominant and blends with the anterior component in most cases. In the relaxed position the normal internal structure of the ligament is difficult to discern due to anisotropy as the fibres are oriented at various angles to the probe. Tensing the ligament, by dorsiflexing the foot, brings the fibres into alignment and reveals the true internal structure.

Figure 23.2 There are three groups in the medial ligament complex. The deep group comprises the anterior and posterior tibiotalar ligaments (dark blue). The superficial group comprises the tibiocalcaneal, tibiospring and tibionavicular ligaments (mid blue). The principal transverse ligament is the calcaneonavicular or spring ligament (light blue).
The normal ligament is triangular or sail shaped with its narrow end superiorly attached to the medial malleolus and its wide portion distally attaching to the talus. The tibiotalar joint is deep to the ligament. If the tibialis posterior is followed a little more distally, the spring ligament appears deep to it (Fig. 23.3). The posterior part of this ligament, the component that is attached to the sustentaculum tali, is identified first as this is its widest portion. If the upper end of the probe is rotated anteriorly, the middle and anterior parts of the ligament come into view, passing around the reverse S shape of the talus towards the navicular. A small bursa, little more than a potential space, is located between the TPT and the spring ligament. This is called the gliding layer. A small quantity of fluid may be present around the tibialis posterior in this location. The other significant component of the medial ligament complex is the tibiospring ligament (Fig. 23.4), which is orientated in the coronal plane, linking the tibia to the spring ligament. The tibiocalcaneal and tibionavicular can be usually found in most individuals but with a more variable appearance.

Figure 23.3 A more distal section just below the medial malleolus shows the flexor hallucis longus within its own fibroosseous tunnel. The tibial nerve (yellow) lies immediately superficial to the tendon. The spring ligament is located beneath the TPT.

Figure 23.4 Coronal T1-weighted MR image showing the relationship of the tibiospring ligament (arrow) to the spring ligament (blue). The spring ligament lies deep to the TPT.
Position 3: Posterior Ankle
Technique
The Achilles tendon is easily located by placing the probe in long axis in the midsagittal plane above the os calcis (Fig. 23.5). It is one of the largest tendons in the body. It can be tracked proximally to where it is joined by the soleus muscle (soleal incorporation) and further proximally where it is formed within the gastrocnemius muscle. Note should be made of the distance between the level of soleal incorporation, usually referred to as the musculotendinous junction, and the insertion to the os calcis. A low incorporation is said to predispose to Achilles tendinopathy. Just before its insertion, the anterior relation of the Achilles tendon is Kager’s fat triangle and the pre Achilles bursa. Normally a very small amount of fluid can be identified within the bursa. Gentle flexion and extension of the foot reveal the movement of the posteroinferior tip of the fat pad within the bursa, helping to define it. This manoeuvre also helps to exclude some forms of pre Achilles bursitis that are more complex and may have ultrasound characteristics similar to the fat pad. The retro Achilles bursa lies posterior to the tendon at the same level. This rarely contains fluid in normal individuals and in many cases can be difficult to identify. It is important not to press too hard with the ultrasound probe as the soft-walled bursa can be easily obscured.

Figure 23.5 The Achilles tendon is best examined with the patient prone. The foot overhangs the end of the examination couch to make tendon movement easier.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree