1. If there is a one-view-only asymmetry, what could be the next step?
2. If a patient was in the office at the time of the exam, what could be the next step?
3. What is a technical repeat in general?
4. What is the most likely malignancy explaining a one-view-only asymmetry?
5. What are the factors that make the judgment difficult, if this is a real finding?
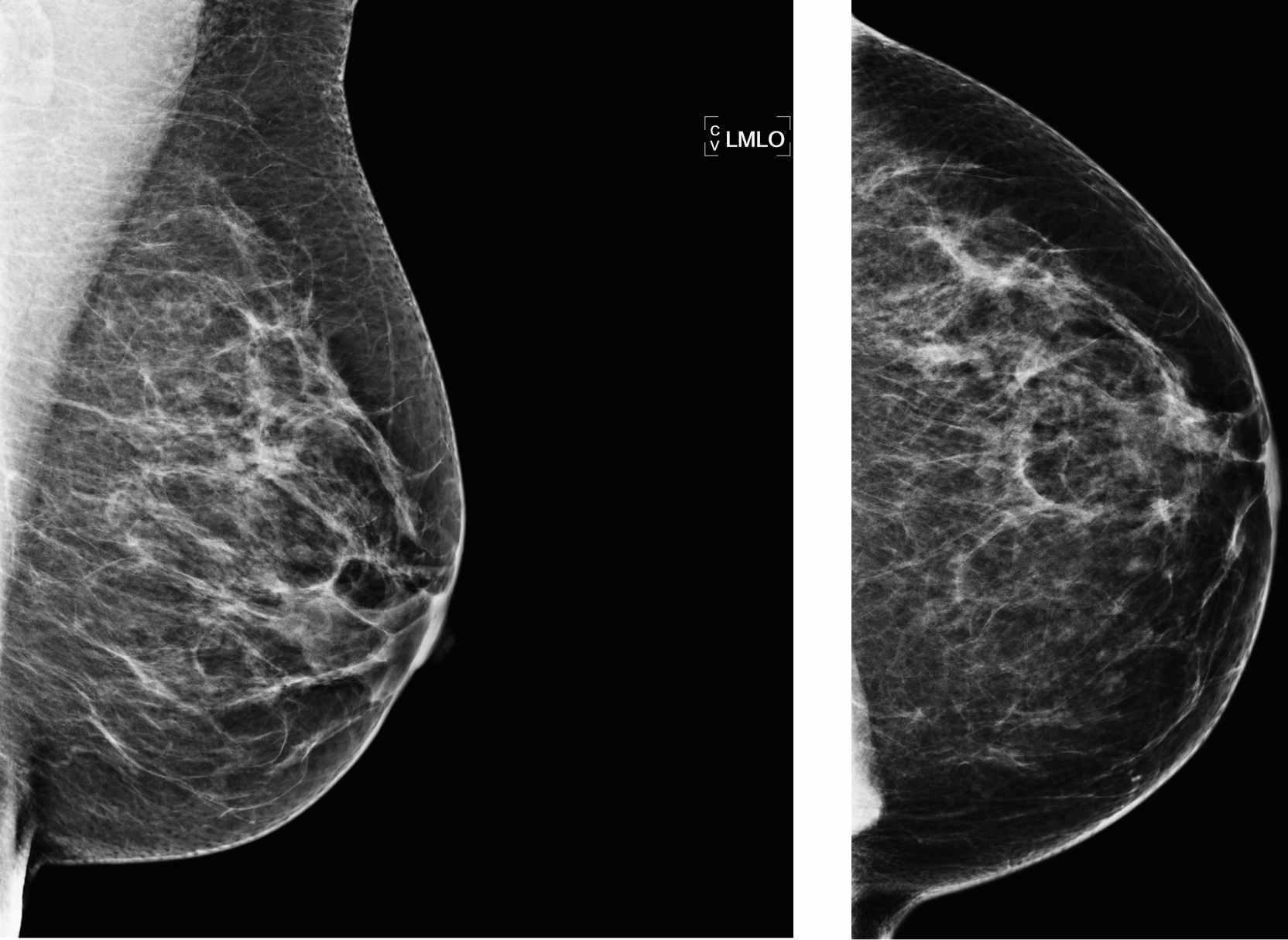
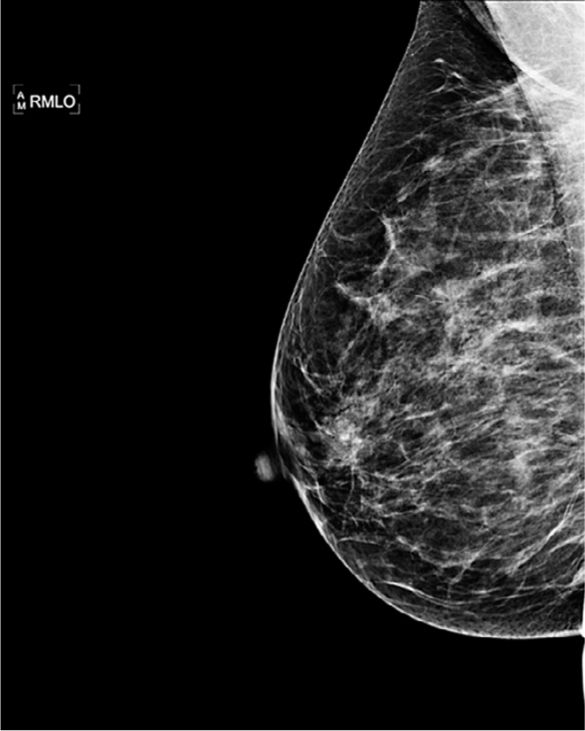
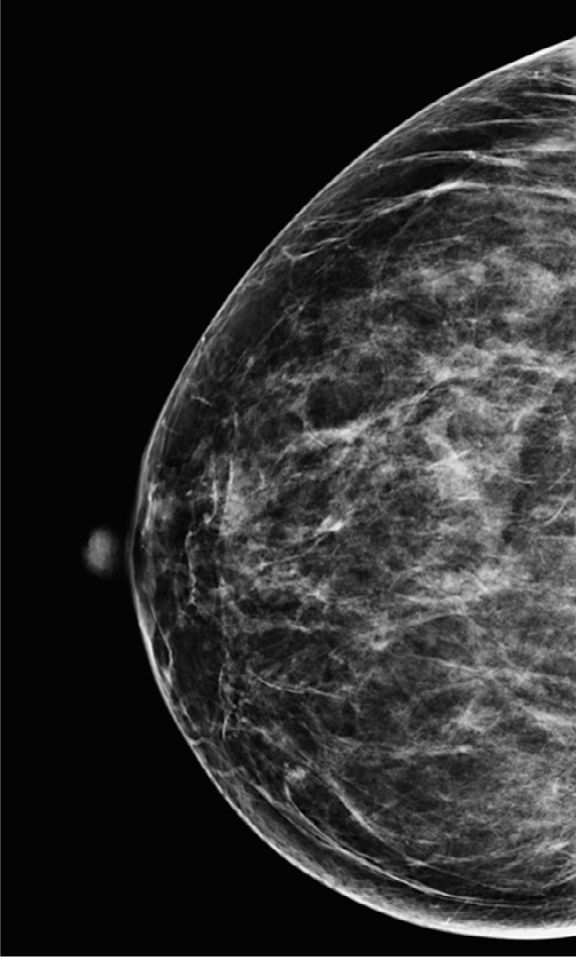
Normal screening mammogram 1626
Case ranking/difficulty: ![]() Category: Screening
Category: Screening
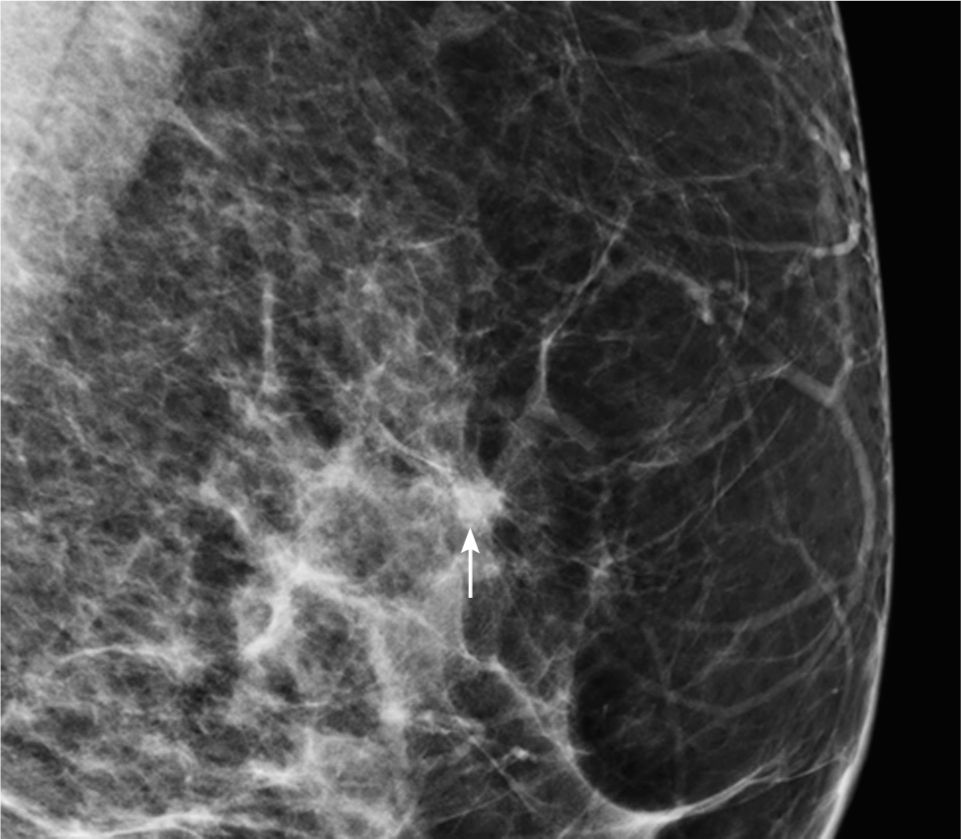
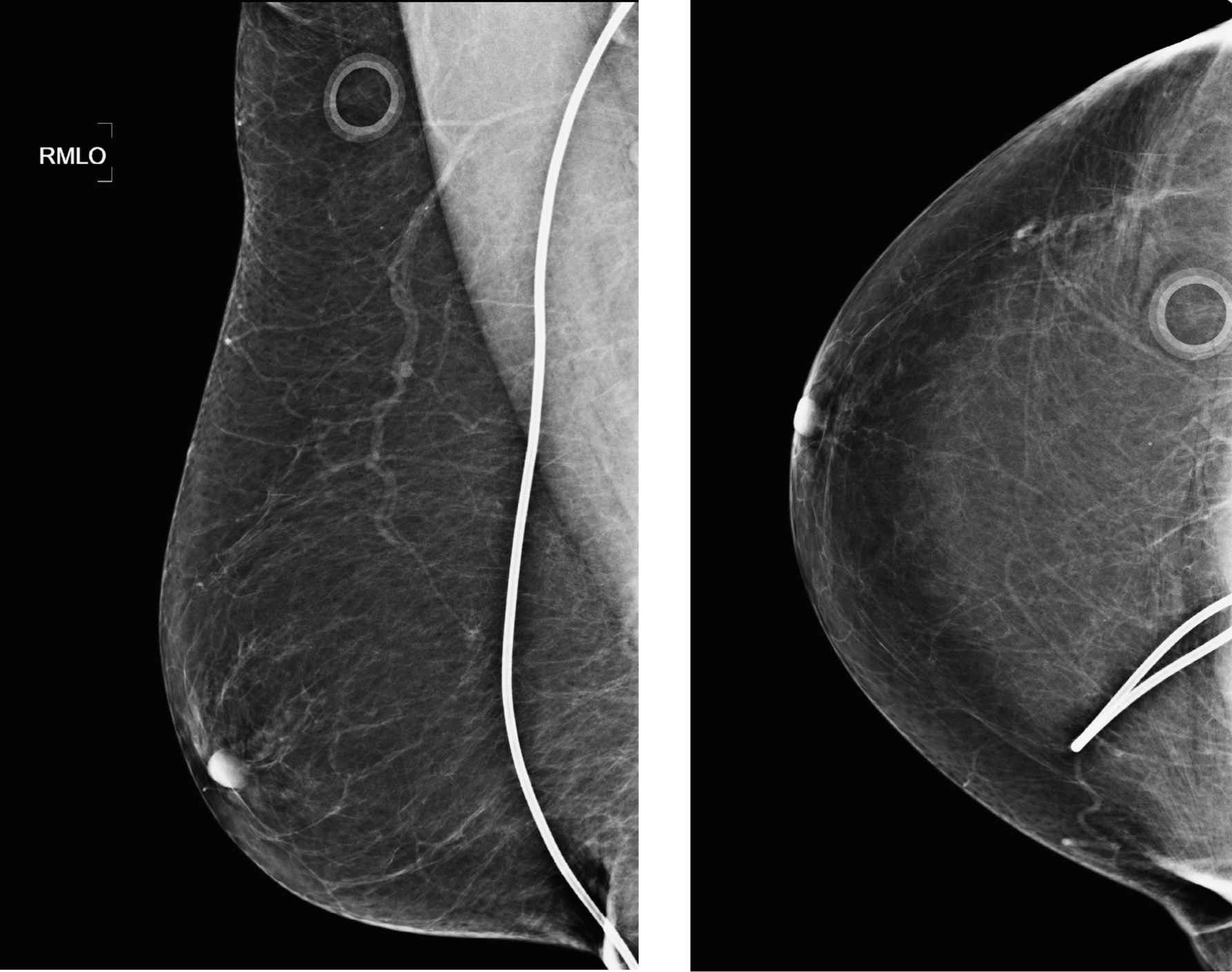
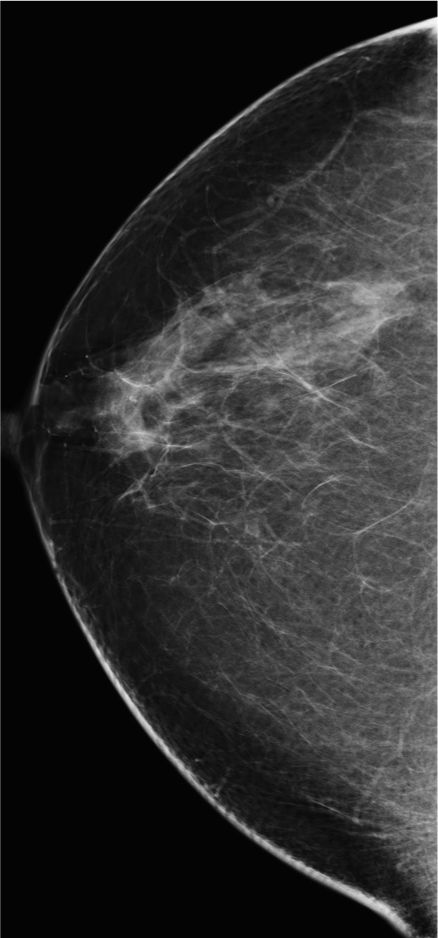
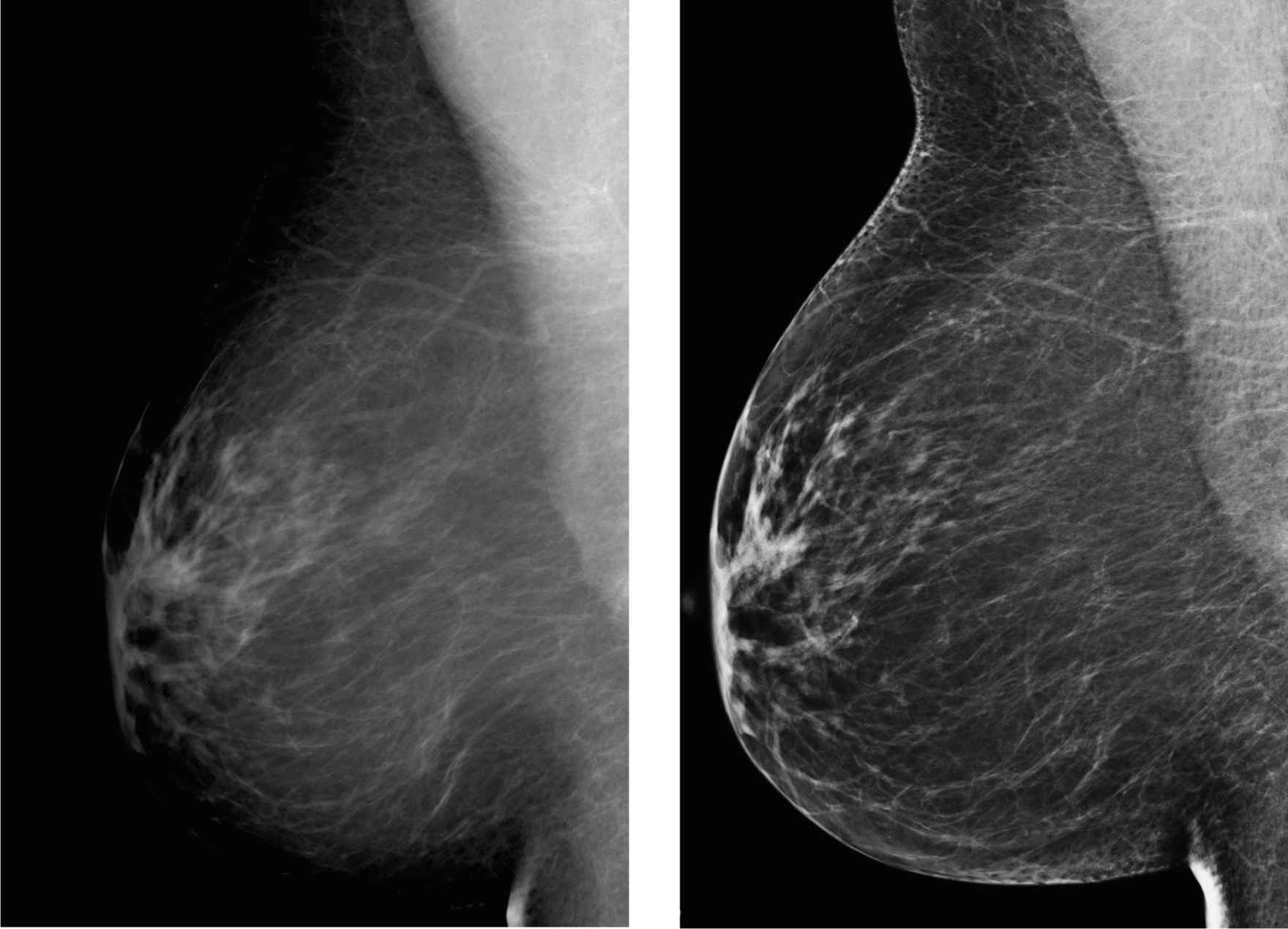
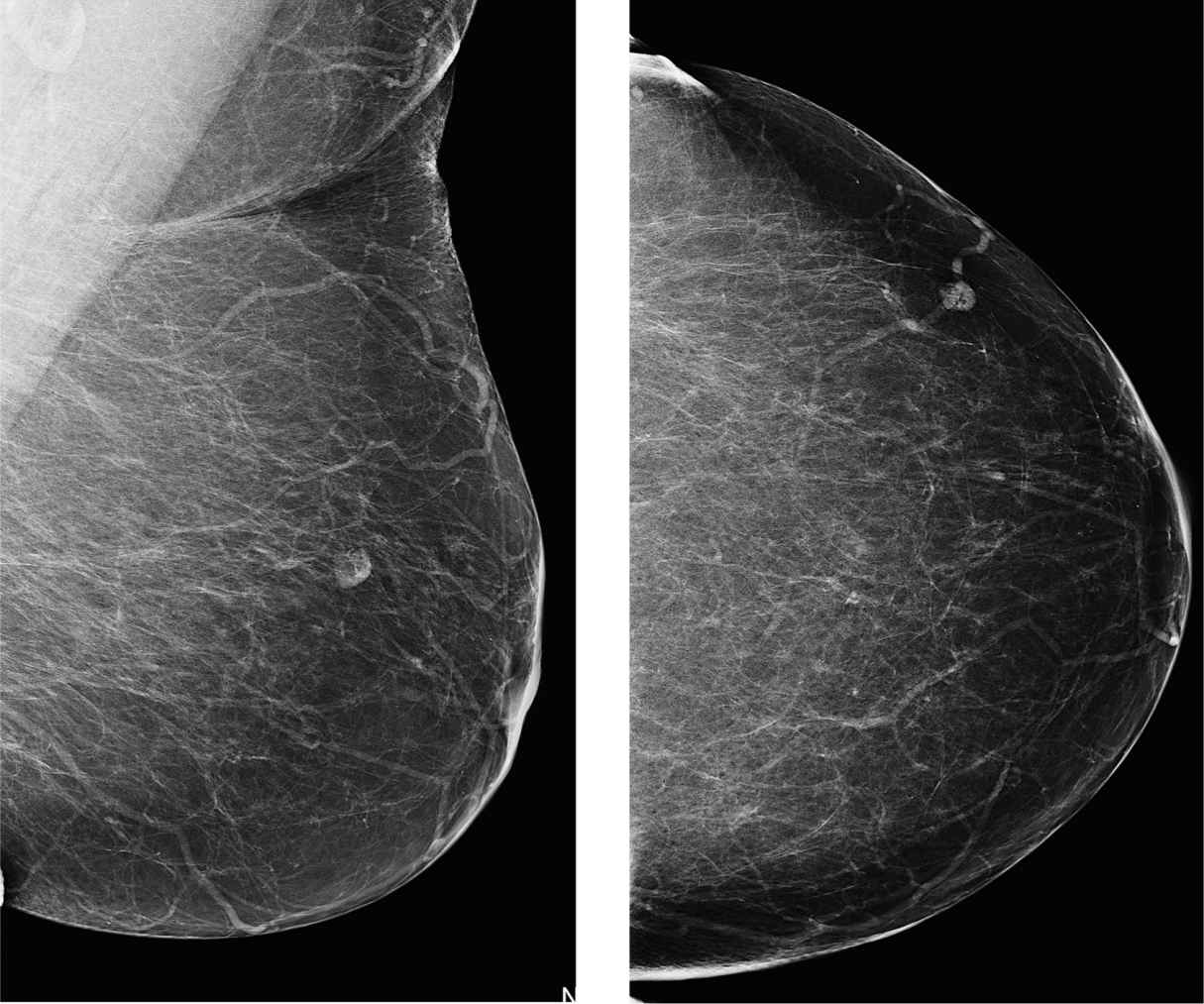
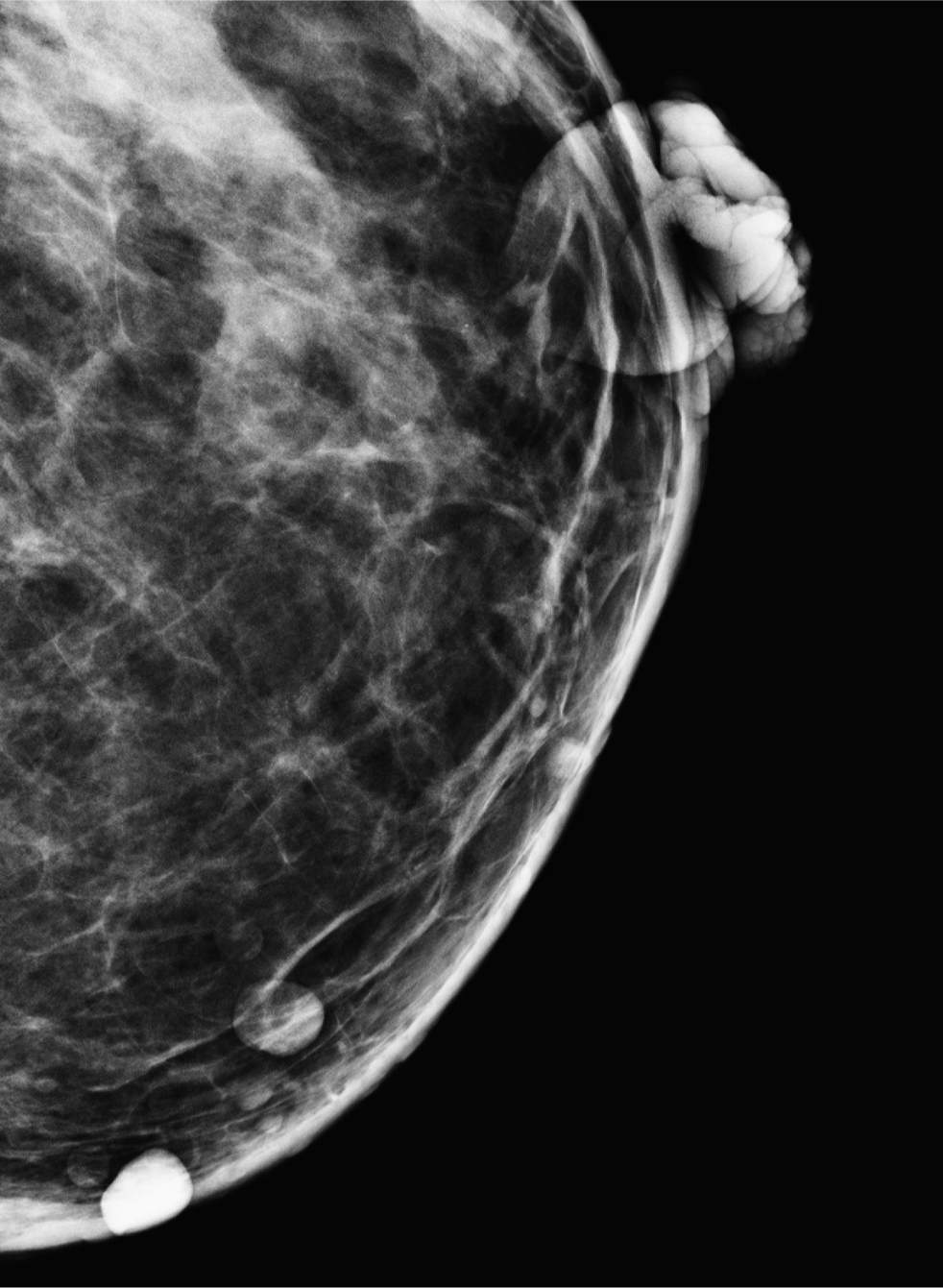
Electronically magnified image of the left MLO screening view.

Repeat left MLO view with different angle demonstrating resolution of the questionable asymmetry.
Answers
1. If there is an asymmetric density seen in one view only, decision has to be made first whether this is real or it is a result of projection and overlying tissue. If the finding is believed to be real, the patient has to be recalled, and if the finding is believed to be the result of projection, then the patient can be classified as BI-RADS 1 negative.
2. If the patient is still in office, a repeat MLO view with different angle could be done and the patient could still be handled as a screening patient. This is not a common environment, since batch reading is performed in the vast majority of places in the United States. If a spot compression view is performed, the patient had to be handled as “recall” and the exam should be labeled as diagnostic mammogram.
3. If there is an indeterminate finding that needs workup, it is called a diagnostic mammogram. If there is limited exam because of motion, incomplete inclusion of tissue, or bad compression, repeat standard views or XCCL view can be added as a “technical repeat.”
If this mammogram is obtained with the patient still available in the office, an additional image can be added with a different angle and the exam could still be classified as a screening exam. However, this scenario is not common, since most screening exams are read without the patient being present (batch reading).
4. Lobular invasive carcinoma is most likely the type of malignancy that can manifest in the form of an asymmetry seen on one view only.
5. One way to eliminate the call back of “one-view-only findings” is to correlate the images with prior studies. Also helpful is if the breast is not very dense which makes correlation with the other plane easier. In case of nipple discharge or palpable abnormality, the patient should be diagnosed in the first place.
Suggested Readings
Pearson KL, Sickles EA, Frankel SD, Leung JW. Efficacy of step-oblique mammography for confirmation and localization of densities seen on only one standard mammographic view. AJR Am J Roentgenol. 2000;174(3):745-752.
Sickles EA. Findings at mammographic screening on only one standard projection: outcomes analysis. Radiology. 1998;208(2):471-475.
Screening mammogram
1. If you see this density on the CC view on screening mammogram, what is the next step?
2. What other options might help if there is clinical concern?
3. How frequent is that finding?
4. What else could be helpful to determine if density in the medial posterior breast is benign?
5. If this was a new suspicious finding, where could it likely hide on the MLO view?
Sternalis muscle 730
Case ranking/difficulty: ![]() Category: Screening
Category: Screening

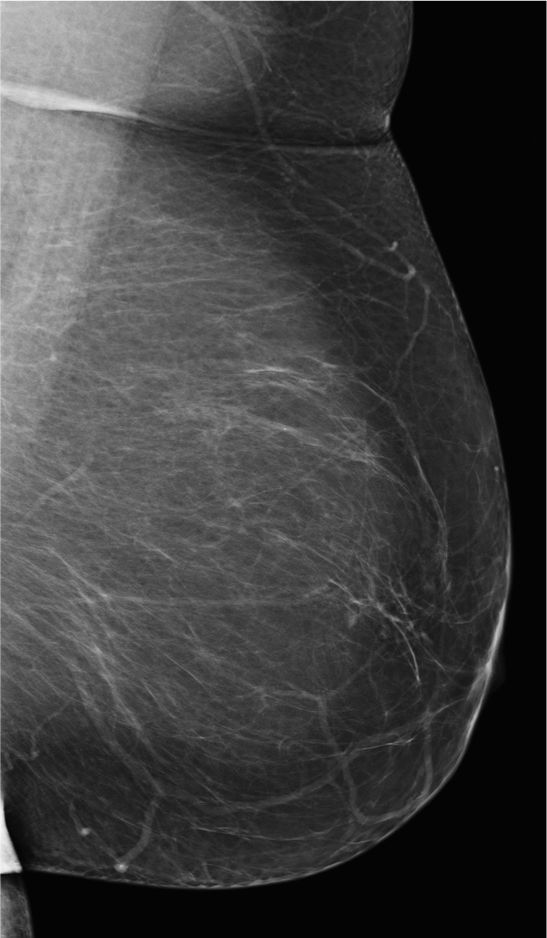
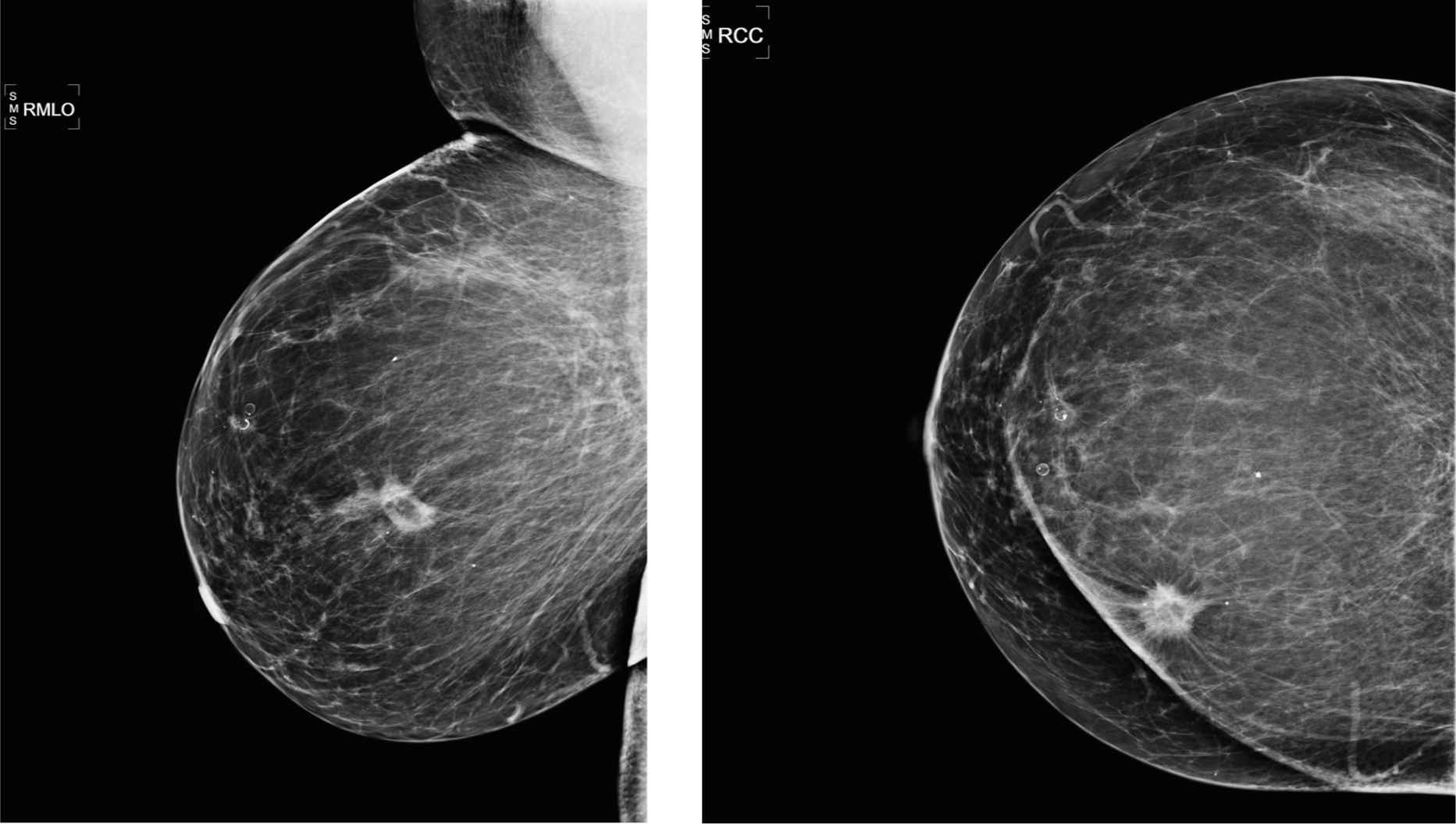
Screening mammogram, right MLO view.
Screening mammogram, right CC view.
Answers
1. This is a typical appearance of a sternalis muscle; in this particular case, bilaterally—it is considered a congenital variant—patient can return after 1 year for screening.
2. If clinical concern, further workup with modified CC views and possible ultrasound might be considered. If this is a sternalis muscle, ultrasound will be normal. As an alternative, correlation with old chest CT could be helpful.
3. It is present in about 8% of the population based on cadaver studies—in about 30% of these, it would show up on the mammogram.
4. If seen bilaterally and if it is stable since prior studies, there is no doubt this is a presentation of sternalis muscle and benign. If it is seen on one view only, and does not show the typical form and location for the presence of sternalis muscle, it is more of a concern—it might not be covered on the MLO view and workup might be necessary.
5. Finding such as seen above in the right CC view of the screening mammogram could hide in the inframammary fold. However, in this case, it is benign finding, consistent with sternalis muscle, given the typical shape, form, and location.
Suggested Reading
Bradley FM, Hoover HC, Hulka CA, et al. The sternalis muscle: an unusual normal finding seen on mammography. AJR Am J Roentgenol. 1996;166(1):33-36.
Prior lumpectomy
1. What BI-RADS classification is used for this entity?
2. What is the one most likely cause for these findings?
3. What is the next best imaging test?
4. What type of biopsy should be performed as one of these is palpable?
5. What type of surgical suture is more prone to calcify on mammograms?
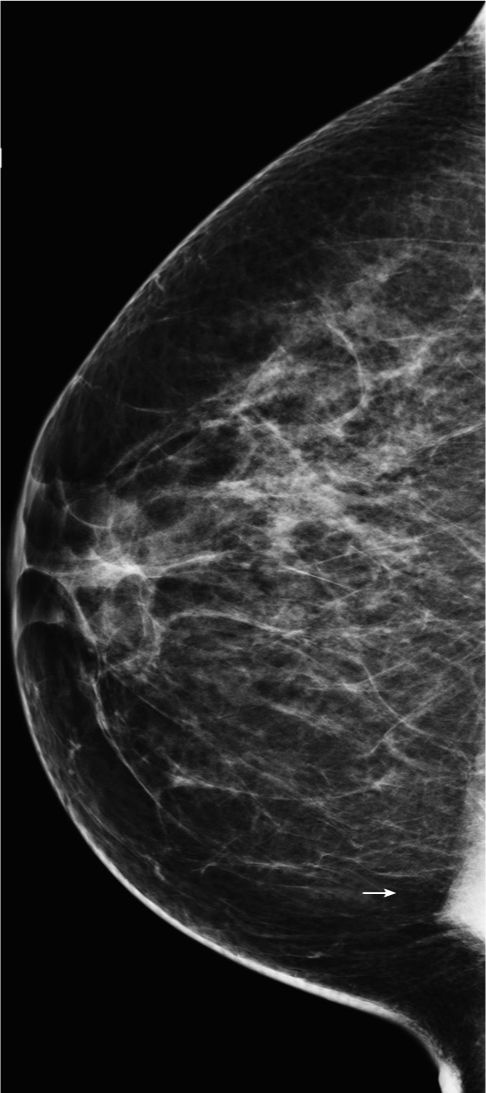
Calcified foreign bodies 1572
Case ranking/difficulty: ![]() Category: Diagnostic
Category: Diagnostic
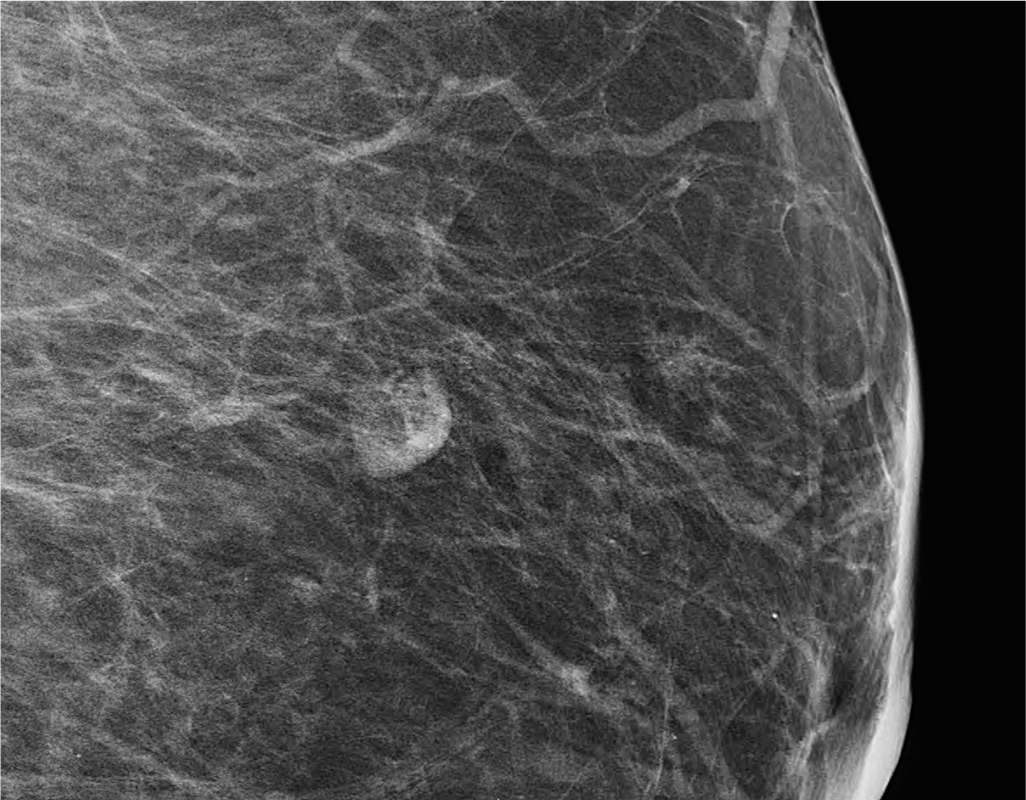
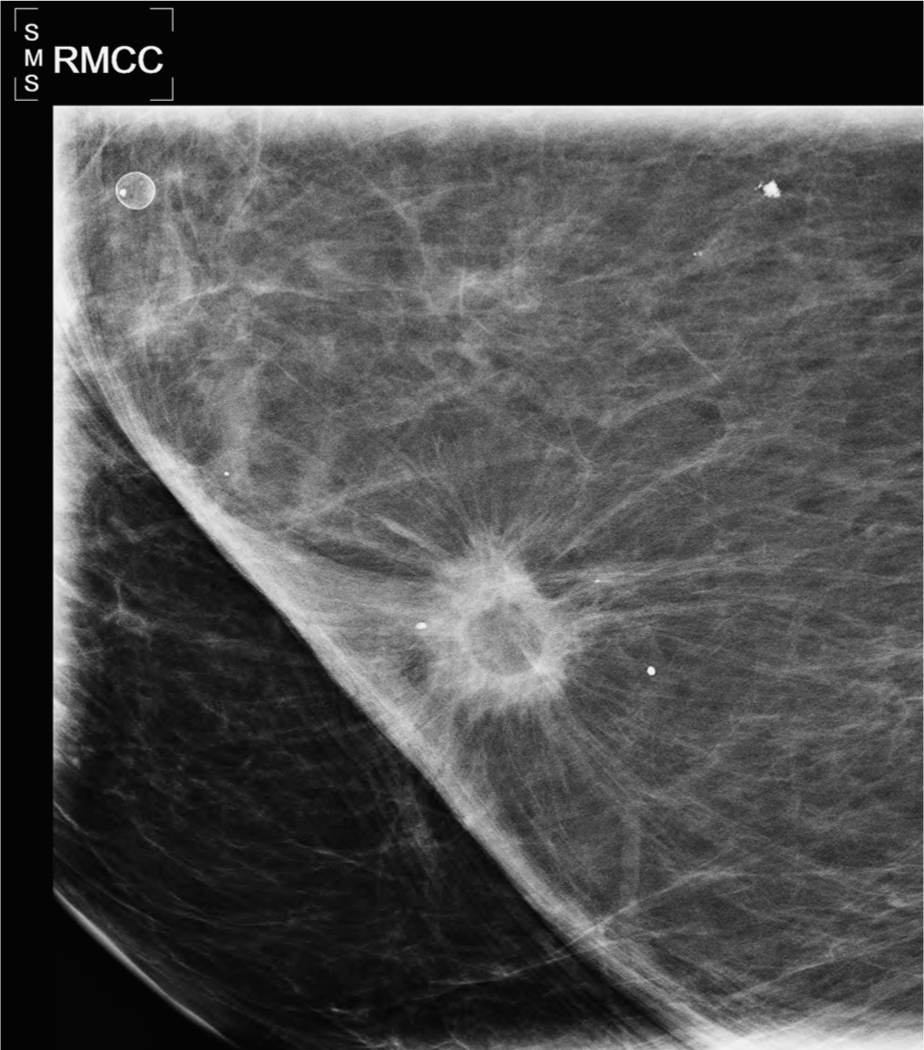
Close-up image shows one of the sutures has a tie.
Answers
1. If you do not describe the abnormality, and as there is nothing else in the breast, you could use BI-RADS 1. However, it is difficult to get away without describing the findings here, and so a more appropriate impression would be BI-RADS 2: benign.
2. Postradiation changes may cause calcifications in vessels and coarse ductal calcification as part of induced apoptosis. Calcifications postimplant removal are more typically at the posterior aspect of the breast disc, and there may be associated silicone granulomas. Calcified guinea worm is sometimes found in women from an area where the worm is prevalent. Ruptured oil cysts show discontinuous calcifications.
3. No further imaging tests are required for this calcified foreign body. The imaging features are diagnostic of calcified sutures.
4. The most prudent thing would be to leave them alone. Catgut sutures are supposed to be reabsorbed over time, but they now have fat necrosis around them. Sometimes, the patient would prefer to see a surgeon to discuss removal. Removal of foreign bodies (eg, biopsy clips) can be done using vacuum-assisted biopsy, so in theory, it could be used here.
5. Catgut usually gets reabsorbed over a period of months or years. However, the sutures can potentially give rise to a severe form of fat necrosis due to the foreign proteins in the catgut. For this reason, many man-made sutures have been used over the years, some of which are still broken down by the human body, and others that have more permanent properties.
Suggested Readings
Libshitz HI, Montague ED, Paulus DD. Calcifications and the therapeutically irradiated breast. AJR Am J Roentgenol. 1977;128(6):1021-1025.
Stacey-Clear A, McCarthy KA, Hall DA, et al. Calcified suture material in the breast after radiation therapy. Radiology. 1992;183(1):207-208.
Prior benign surgical biopsy of the left breast
1. What BI-RADS classification should be used here?
2. What is the one most likely cause for these findings?
3. What produce calcified lesions that can be identified on mammography
4. What is the best view to identify the track of a VP shunt?
5. What is the risk of malignant transformation around a VP shunt?
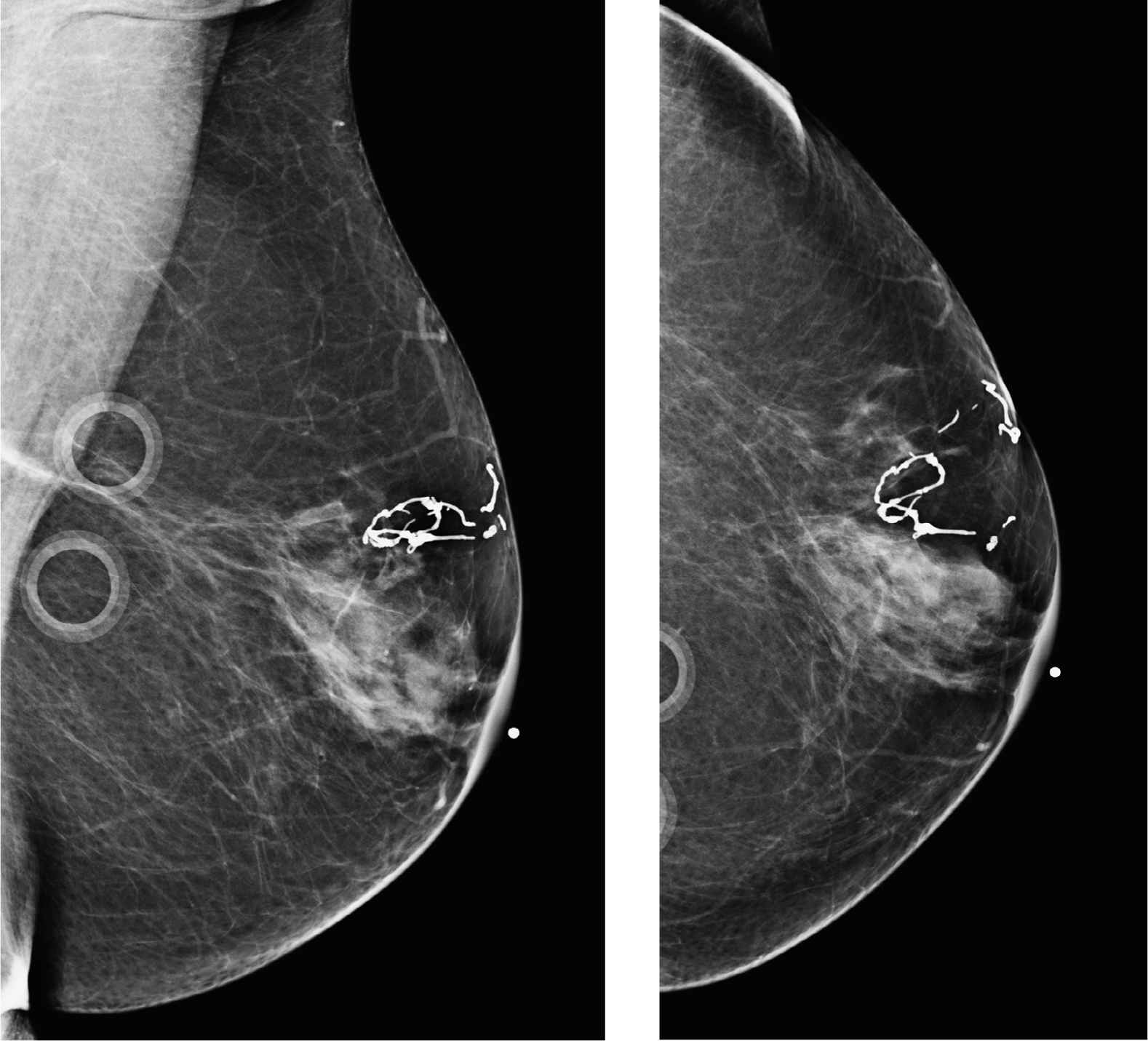
Ventriculoperitoneal shunt 1642
Case ranking/difficulty: ![]() Category: Diagnostic
Category: Diagnostic
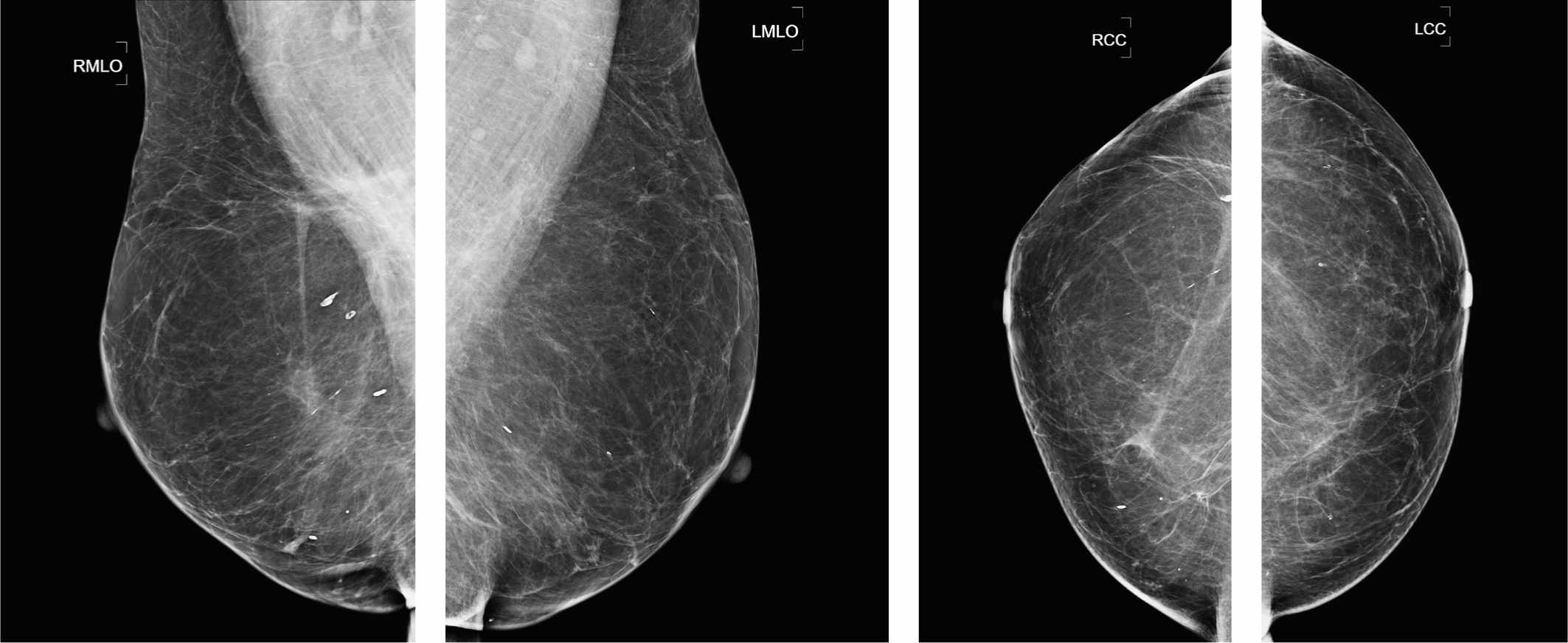
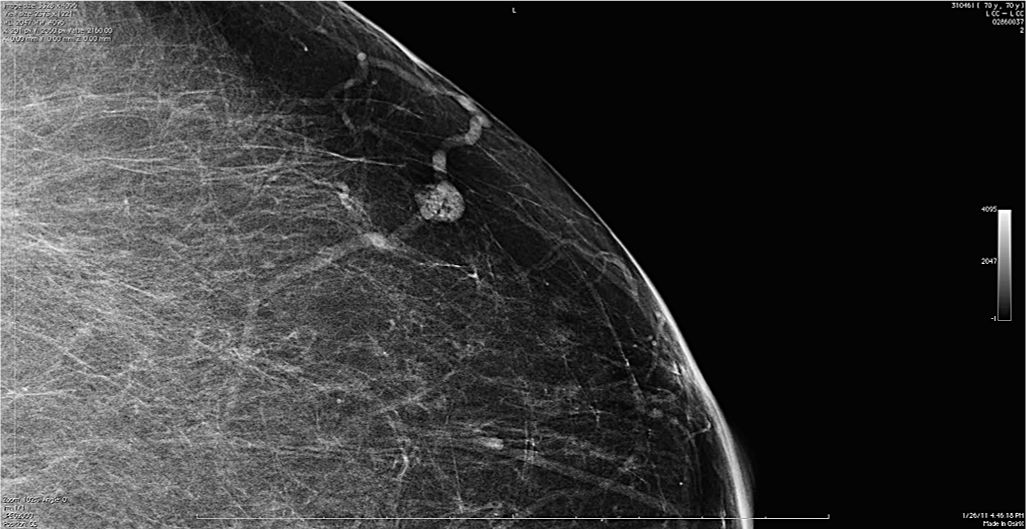
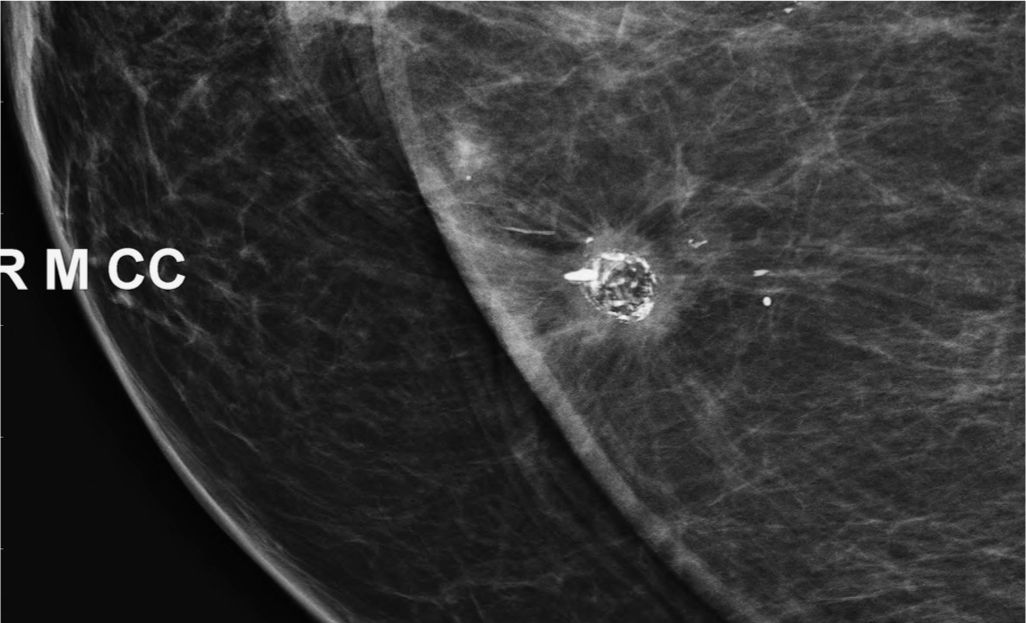
Bilateral MLO exam showing another case of a calcified ventricle-peritoneal shunt that had been in situ for the life of the patient.
Answers
1. In general, if you describe a finding, then BI-RADS 2 should be used. However, a BI-RADS 1 could equally be used as the finding is not within the breast itself.
2. This is typical of a ventriculoperitoneal shunt, as treatment for hydrocephalus.
3. Dracunculiasis is a guinea worm. When the parasite dies, it calcifies and appears as a loosely coiled tubular structure. Sutures may calcify, particularly if the patient has had radiation treatment. Surgical clips are inert and do not typically calcify. Pacemaker wires have occasionally been reported as calcified in the subdermal portion of its track. VP shunts calcify in the two examples shown here, as they are in the body for a very long time.
4. In general, the MLO view shows the tube entering from the superior breast and exiting through the inferior part. There are variable appearances on the CC, depending on its track. XCCL, cleavage views, and laterals sometimes help if you cannot see the tube adequately, but they are not usually required for diagnosis.
5. There is a published case report of a multifocal tumor around a VP shunt, but this is likely to be a very rare finding.
Suggested Readings
Ioannis K, Ioannis K, Angelos L. Routine mammographic imaging: it was only a needle. Breast J. 2006;12(5):493.
Lee D, Cutler B, Roberts S, Manghisi S, Ma AM. Multi-centric breast cancer involving a ventriculoperitoneal shunt. Breast J. 2010;16(6):653-655.
Vimalachandran D, Martin L, Lafi M, Ap-Thomas A. Cerebrospinal fluid pseudocyst of the breast. Breast. 2003;12(3):215-216.
Screening—asymptomatic
1. What BI-RADS classification should be used here?
2. What should be the next diagnostic imaging exam?
3. What type of surgery may this patient have had?
4. What type of biopsy should be performed?
5. What type of follow-up surveillance would you recommend?
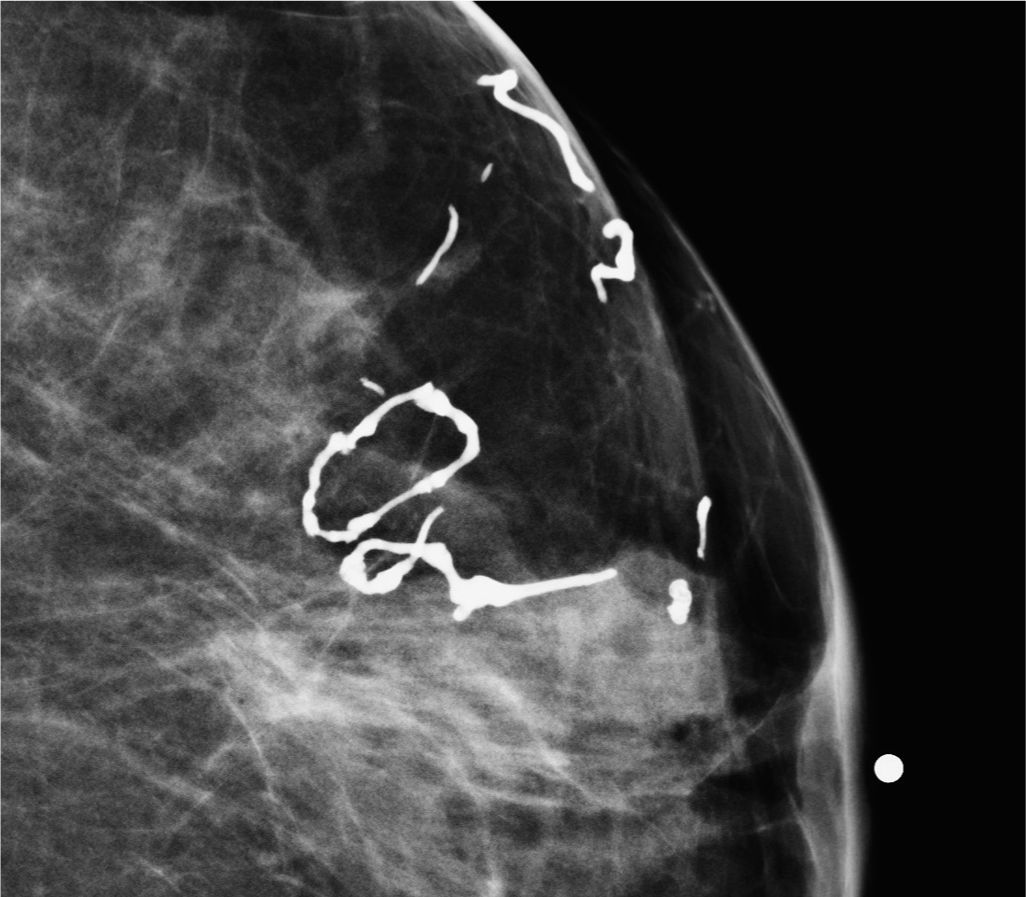
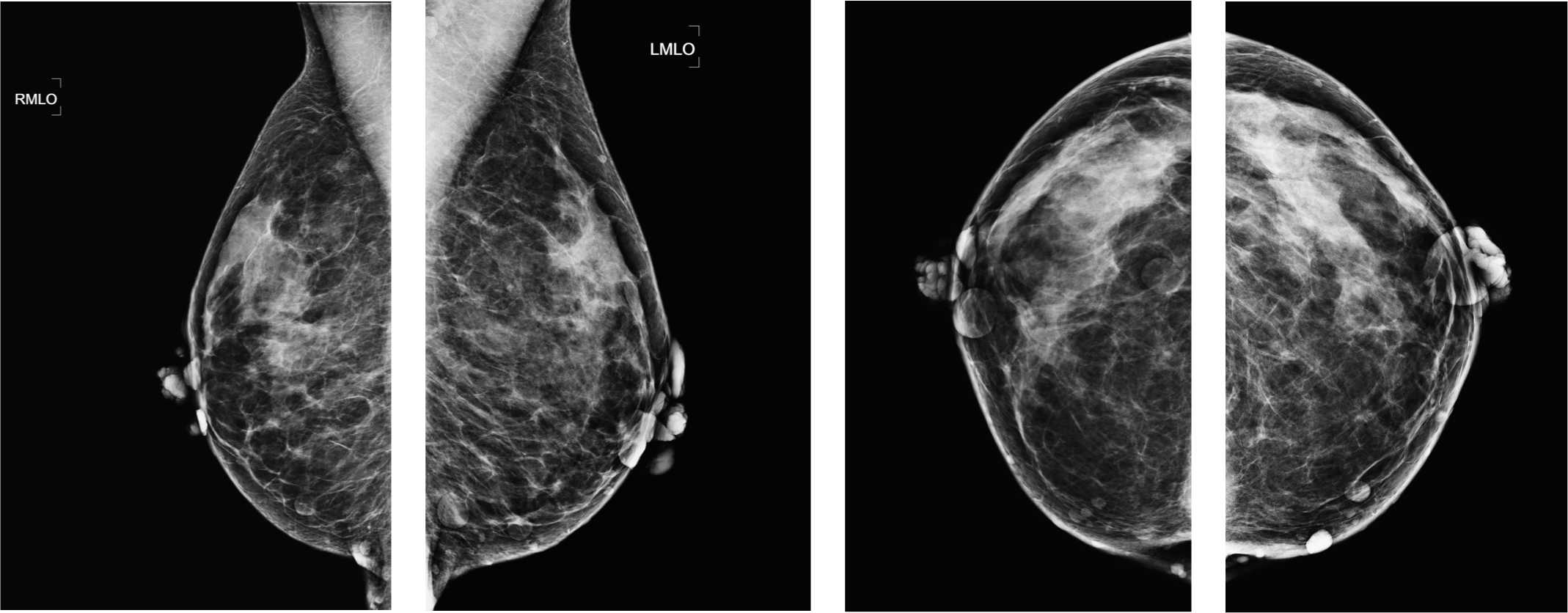
Breast reduction scars 1753
Case ranking/difficulty: ![]() Category: Screening
Category: Screening

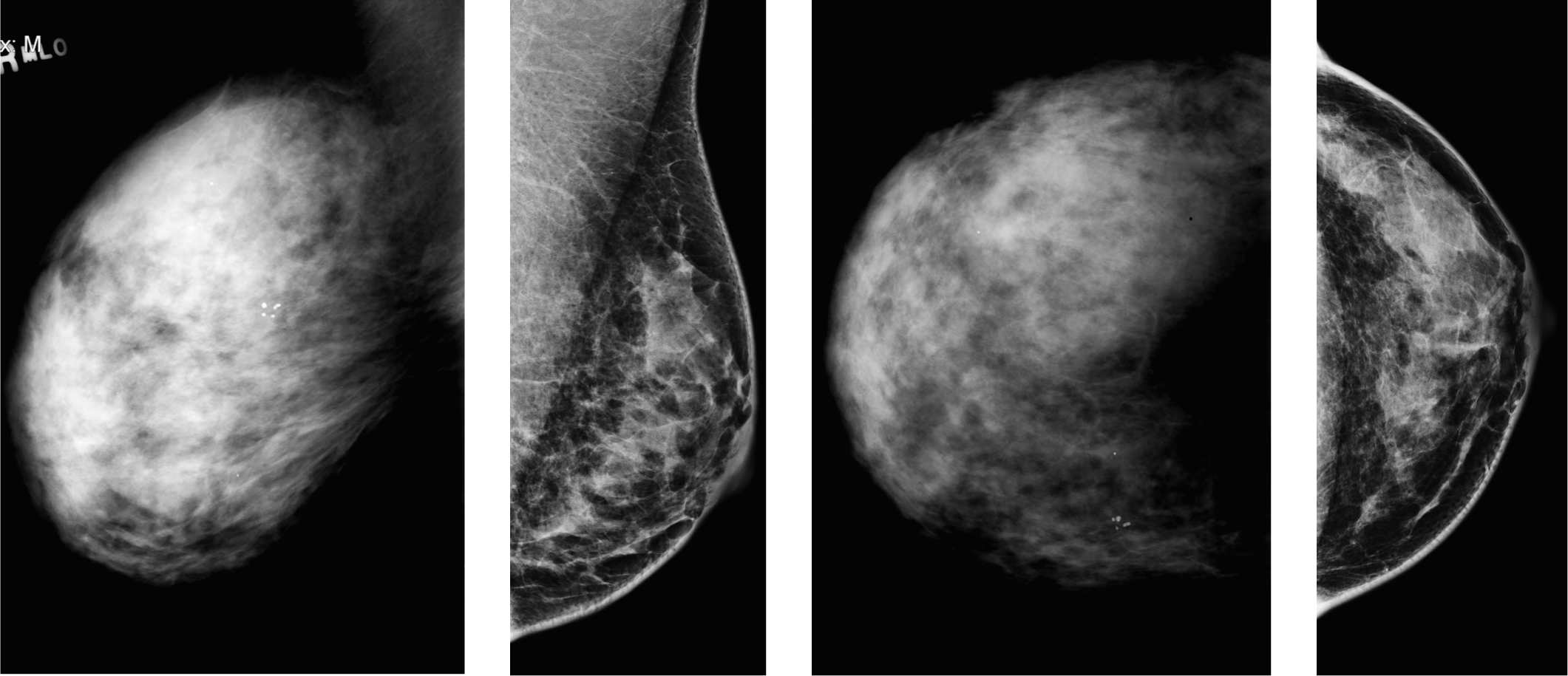
Another case of breast reduction showing a transverse line across the posterior part of the breast disc. Lines occurring that are not expected.
Answers
1. The findings of the scars are characteristic. You can ignore the scars and give a negative for malignancy BI-RADS 1 assessment, or describe the finding and give it a BI-RADS 2, benign.
2. No further workup is required, as the finding is normal postsurgical appearances.
3. These are the scars from a mastopexy (otherwise known as a breast reduction). TRAM reconstruction has its own characteristic imaging findings. Bilateral lumpectomy scars or multiple benign surgical biopsies could in theory give these appearances.
4. No biopsy is required as this is an “Aunt Minnie” appearance of postreduction scars. Biopsy may be required of palpable areas of fat necrosis occurring following this type of surgery.
5. The patient can be followed with routine screening, unless the operation was relatively recent, in which case annual diagnostic mammography is recommended.
Suggested Readings
Beer GM, Kompatscher P, Hergan K. Diagnosis of breast tumors after breast reduction. Aesthetic Plast Surg. 1997;20(5):391-397.
Muir TM, Tresham J, Fritschi L, Wylie E. Screening for breast cancer post reduction mammoplasty. Clin Radiol. 2010;65(3):198-205.
Rubin JP, Coon D, Zuley M, et al. Mammographic changes after fat transfer to the breast compared with changes after breast reduction: a blinded study. Plast Reconstr Surg. 2012;129(5):1029-1038.
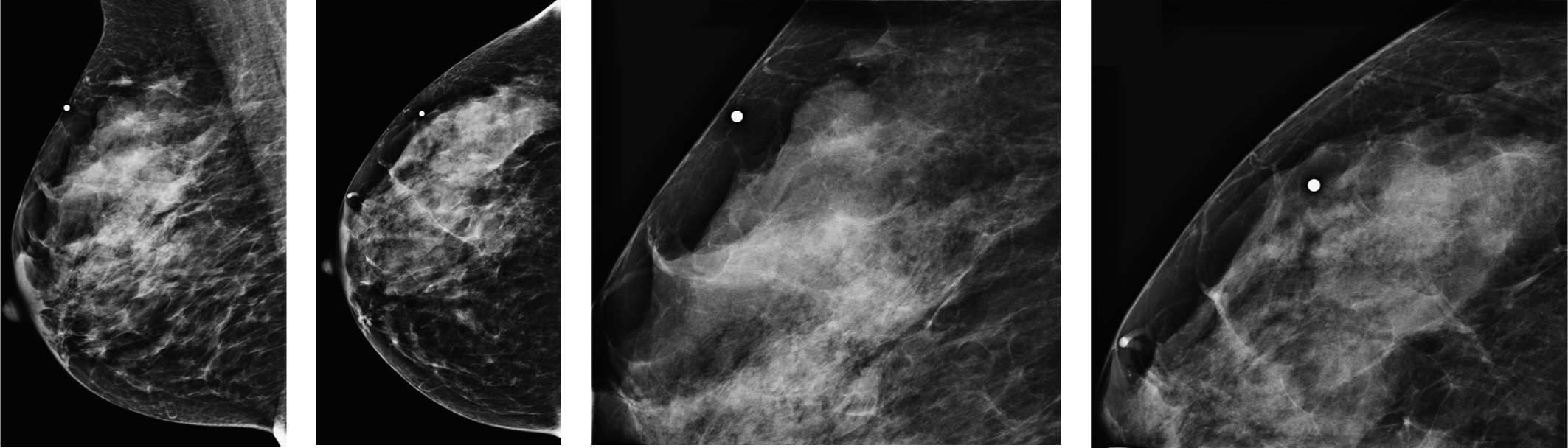
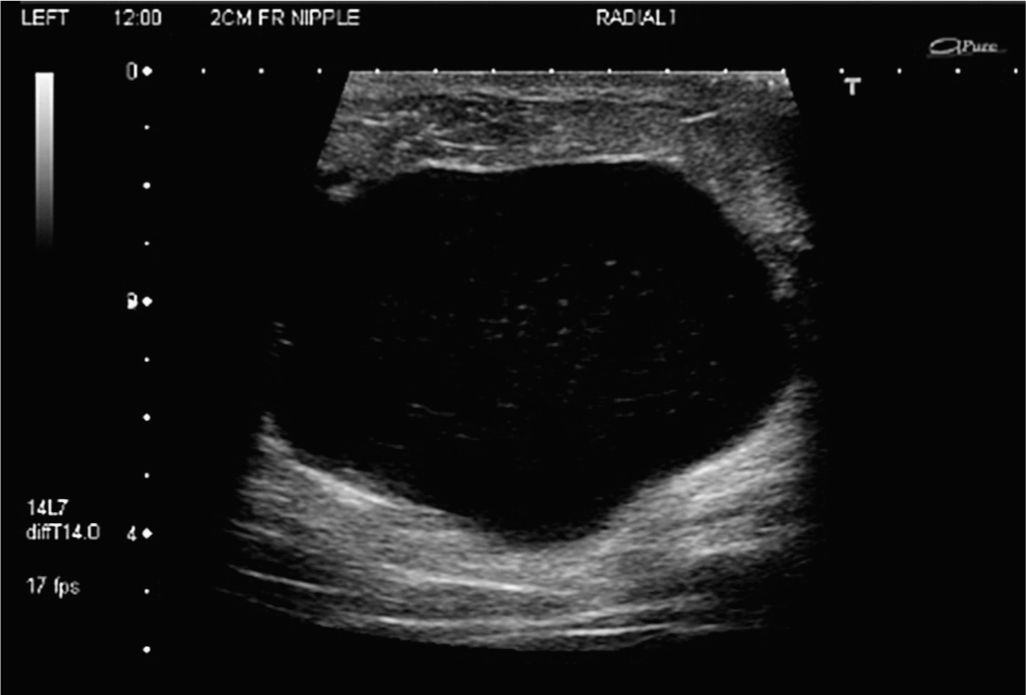
Different breast compositions—what does that mean?
1. What are the different choices in BI-RADS lexicon for relatively dense breasts?
2. What are the two choices in BI-RADS lexicon for relatively less dense breasts?
3. What is the consequence of very dense fibroglandular tissue?
4. Why is mammography not worthless in very dense patients?
5. What other breast screening exams exist in the United States?
Importance of breast composition 1298
Case ranking/difficulty: ![]() Category: Screening
Category: Screening

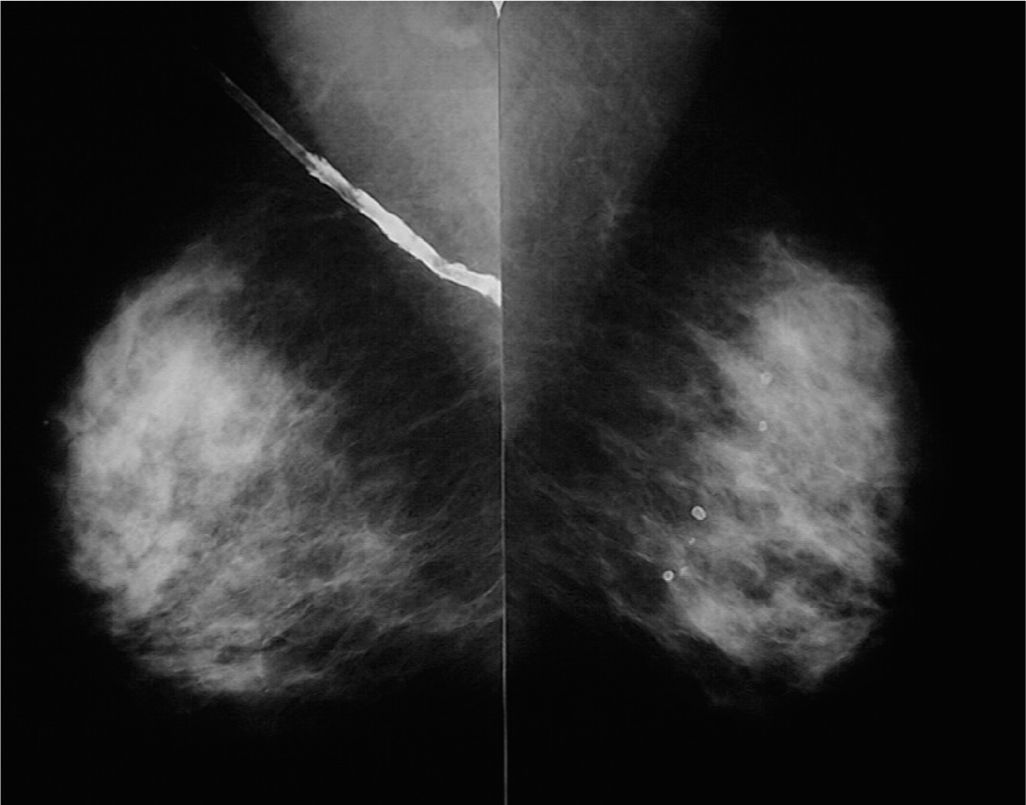
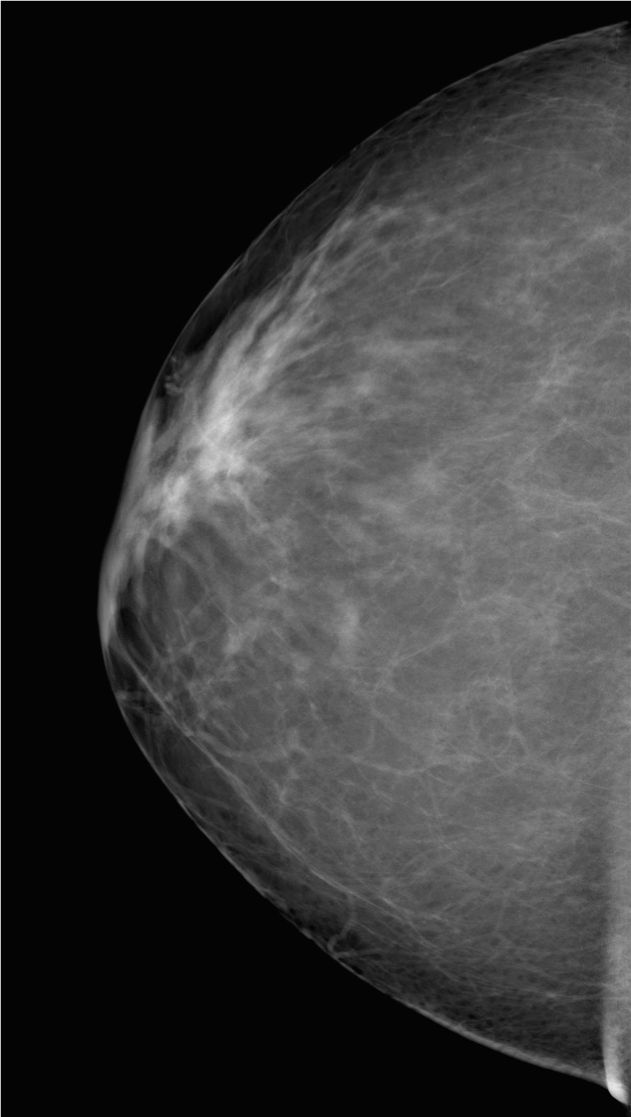
Screening mammogram, right MLO view demonstrating “scattered fibroglandular tissue.”
Screening mammogram, right CC view demonstrating “scattered fibroglandular tissue.”
Screening mammogram, left MLO view demonstrating “almost entirely fatty replaced” tissue.
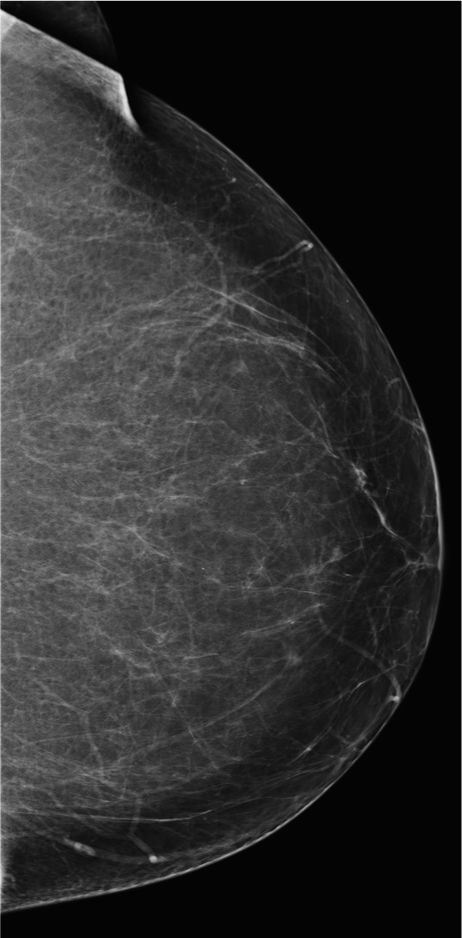
Screening mammogram, left CC view demonstrating “almost entirely fatty replaced” tissue.
Answers
1. There are four categories to describe the composition of the breast: The two categories describing denser breasts are (1) “extremely dense” (>75% glandular tissue) and (2) “heterogeneously dense” (51–75% glandular tissue).
2. There are two categories describing less dense breast compositions: (1) “scattered fibroglandular tissue” (25–50% glandular tissue) and (2) “almost entirely fatty replaced” (<25% glandular tissue).
3. The sensitivity of mammography is significantly reduced and this results in less value of the mammogram. However, it is still valuable and does not eliminate the need for screening. To obtain old images is even more important. Additional exams, such as MRI and ultrasound, might be helpful. In the United States, only screening MRI is officially accepted as additional screening exam. Ultrasound is more controversial.
4. Mammography is still very helpful. It can still show calcifications, and might be able to show distortion or masses. Mammography will be limited in value because of its reduced ability to detect developing densities.
5. Only MRI is accepted by insurance companies for screening, but only in high-risk patients (lifetime risk of more than 20–25%). Ultrasound is not accepted as a screening exam but sometimes ordered by referring physicians (gray zone) with the indication such as “fibrocystic changes.”
Suggested Readings
Boyd NF, Martin LJ, Bronskill M, Yaffe MJ, Duric N, Minkin S.
Breast tissue composition and susceptibility to breast cancer. J Natl Cancer Inst. 2010;102(16):1224-1237.
Boyd NF, Martin LJ, Yaffe MJ, Minkin S. Mammographic density and breast cancer risk: current understanding and future prospects. Breast Cancer Res. 2011;13(6):223.
Screening—asymptomatic
1. What BI-RADS classification should be used here?
2. What should be the next diagnostic imaging exam?
3. What type of surgery may this patient have had?
4. What type of biopsy should be performed?
5. What type of follow-up surveillance would you recommend?
Lipoma in dense breasts 583
Case ranking/difficulty: ![]() Category: Diagnostic
Category: Diagnostic
Answers
1. This lesion is characteristically benign, BI-RADS 2.
2. This lesion is composed of fat (adipose). The lesion would have glandular density and therefore invisible if it were composed of normal fibroglandular elements. Cooper’s ligaments are the small curvilinear lines attaching the glandular disc to the skin.
3. This finding is characteristic enough to recommend return to routine screening. It should be visible on prior examinations. Lipomas can be surprisingly hard to demonstrate on ultrasound. Non-fat sat T1 MRI can confirm that the lesion contains fat. Tomosynthesis should be able to demonstrate the findings clearly, compared with conventional 2D mammograms.
4. Clearly, if this lesion is diagnostic of a lipoma, then biopsy is not indicated.
5. The palpation findings of a lipoma are usually either nothing or a soft lump. Sometimes, the margins may not be easily felt, and then described as a vague soft lump. In rare instance that a lipoma gets infected, the findings may be of a hard lump, but there are clearly other signs of infection.
Suggested Readings
Kapila K, Pathan SK, Al-Mosawy FA, George SS, Haji BE, Al-Ayadhy B. Fine needle aspiration cytology of breast masses in children and adolescents: experience with 1404 aspirates. Acta Cytol. 2009;52(6):681-686.
Kirova YM, Feuilhade F, Le Bourgeois JP. Breast lipoma. Breast J. 2002;8(2):117-118.
Lanng C, Eriksen BØ, Hoffmann J. Lipoma of the breast: a diagnostic dilemma. Breast. 2004;13(5):408-411.
Screening mammography 2009 (left) and 2011 (right)

1. Can you see any abnormality on the new screening mammogram?
2. Which of the mammogram is digital?
3. What is the advantage of digital mammogram over film mammography?
4. What is the disadvantage of digital mammography in comparison with film mammography?
5. What are the practical consequences reading digital mammograms?
Digital versus film mammography 306
Case ranking/difficulty: ![]() Category: Screening
Category: Screening
Screening film mammogram, right CC view 2006.
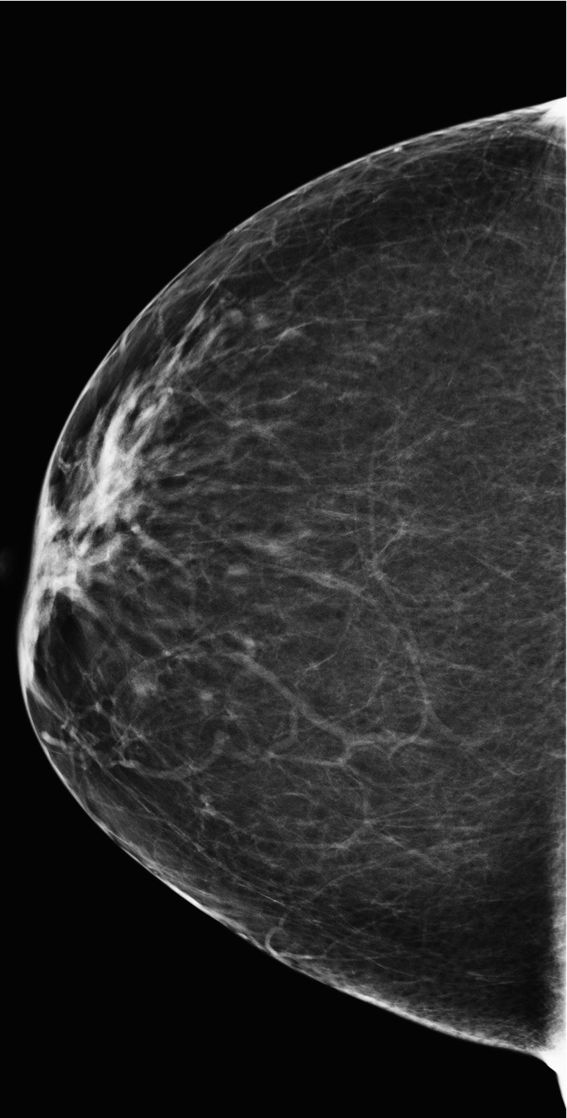
Screening digital mammography, right CC view 2011.
Answers
1. The exam from 2011 does not demonstrate any abnormality in comparison with the exam from 2009.
2. The 2011 exam is digital, whereas the 2009 exam is screen film mammography. The digital study demonstrates better contrast resolution.
3. Digital mammography has the advantage of better contrast resolution, which is helpful to detect developing malignancy in dense breast tissue.
4. Digital mammography has less spatial resolution then film mammography—this was for a long time the limiting factor in establishing digital mammography. The advantage of better contrast resolution, however, has been shown to outweigh the disadvantage of less spatial resolution.
5. Switching from reading screening film mammograms to reading screening digital mammograms requires to adjust the threshold to recall patient for densities as a result of the increased contrast resolution and to adjust the threshold to recall patient for calcifications as well.
Suggested Readings
Karssemeijer N, Bluekens AM, Beijerinck D, et al. Breast cancer screening results 5 years after introduction of digital mammography in a population-based screening program. Radiology. 2009;253(2):353-358.
Lewin JM, Hendrick RE, D’Orsi CJ, et al. Comparison of full-field digital mammography with screen-film mammography for cancer detection: results of 4,945 paired examinations. Radiology. 2001;218(3):873-880.
Well woman screening exam
1. What BI-RADS classification should be used here?
2. In which groups of women did the DMIST study show benefit?
3. What is the dose of a digital mammogram relative to analog?
4. Which of the following are some of the benefits of digital versus analog?
5. What of the following findings or structures are better seen with digital mammography?
Analog versus digital comparisons 1728
Case ranking/difficulty: ![]() Category: Screening
Category: Screening
Answers
1. Normal dense breast tissue, better seen on digital. The appropriate BI-RADS classification is therefore 1: negative for malignancy. The first time a digital mammogram is performed on the woman, there is a higher probability of finding calcifications that you are not sure could be seen on the analog mammogram. In that instance, you need to give a BI-RADS 0 and recall for workup.
2. The DMIST study was performed to answer the question as to whether digital mammography was better than analog mammography, but only really had to show equivalence to gain acceptance. There were three groups of women where some benefit was shown: those with dense breasts, women younger than 50 years, and perimenopausal women. There is some evidence that digital mammography is less effective than screen-film mammography in women with fatty breasts. However, this is being addressed by some manufacturers, changing their anodes to tungsten from molybdenum.
3. It can vary by tissue type, but there has generally been a drop in mean glandular radiation dose during the switch to digital. Further reductions have also occurred using photon counting techniques, where radiation doses are approximately 50% lower than regular mammograms. Tomosynthesis as a new technology started at approximately three times the regular dose of mammography as the FDA required a regular mammogram in addition to the 3D exam. Measures have been taken, which has reduced to approximately 1.6 times, and still within the 2 mGy FDA requirement.
4. The effects on the environment and concerns over the disposal of silver used to be a big concern. There is little difference in radiation dose compared with analog mammography, except for a few systems, for example, Philips MicroDose, which has approximately 50% normal radiation dose. Digital allows you to perceive calcifications much easier. A small digital reimbursement supplement that is likely to disappear now as analog is virtually extinct. CAD has been available for analog systems, but it is more efficient on digital systems.
5. Most of the above are correct, and some may argue that all are correct, as the dynamic range of digital and the contrast resolution of digital mammography makes everything easier to see.
Suggested Readings
Kopans DB, Pisano ED, Acharyya S, et al. DMIST results: technologic or observer variability? Radiology. 2008;248(2):703; author reply 703.
Pisano ED, Hendrick RE, Yaffe MJ, et al. Diagnostic accuracy of digital versus film mammography: exploratory analysis of selected population subgroups in DMIST. Radiology. 2008;246(2):376-383.
Zuley M. How to transition to digital mammography. J Am Coll Radiol. 2007;4(3):178-183.
Patient with screening exam
1. What is the workup for “round” mass seen on first mammogram?
2. What is the next step if fat cannot be visualized?
3. What is the characteristic finding of an intramammary lymph node?
4. Where is the location of the mass?
5. What would you do if the mammogram does not show fat but ultrasound demonstrates a large fatty hilum?
Lymph node on first screening 394
Case ranking/difficulty: ![]() Category: Screening
Category: Screening
Diagnostic mammogram, left MLO view demonstrates benign-appearing mass with fat.
Diagnostic mammogram, left CC view demonstrates benignappearing mass with fat
Answers
1. Next step in general is workup with spot compression views.
2. Ultrasound can be used for further characterization. If that does not show any abnormality, the finding is probably benign and 6-month follow-up mammography is recommended. If ultrasound demonstrates the mass, it can be further characterized on ultrasound. If ultrasound demonstrates cysts in internal echoes or thin membranes (“complicated cyst”), cyst aspiration or as an alternative 6-month follow-up and ultrasound surveillance over 2 years is recommended.
3. It is generally located in the upper outer quadrant. If fat is seen on the mammogram, it is diagnostic for lymph node. Lymph nodes are also sometimes located in other parts of the breast. They are in general well circumscribed.
4. It is located slightly superior on MLO and very lateral on CC view.
5. In this case, the ultrasound finding likely does not correlate to the mammogram. Mammogram should show fat as well. The ultrasound finding is benign and does not need follow-up. The mammogram finding does need follow-up if it is not new but seen on first mammogram and does not contain definitely fat. Bottom line: if ultrasound finding does not correlate, 6-month follow-up mammogram is recommended for a well-circumscribed mass seen on first mammogram.
Suggested Reading
Meyer JE, Ferraro FA, Frenna TH, et al. Mammographic appearance of normal intramammary lymph nodes in an atypical location. AJR Am J Roentgenol.1993;161:779-780.
Prior chemotherapy—finding of palpable right axilla
1. What BI-RADS classification should be used here?
2. What is the next best imaging test?
3. Which of the following are known causes of bilateral axillary adenopathy?
4. From which cell line does Non-Hodgkin lymphoma (NHL) arise?
5. How does primary breast lymphoma present?
Lymphoma patient 1646
Case ranking/difficulty: ![]() Category: Diagnostic
Category: Diagnostic

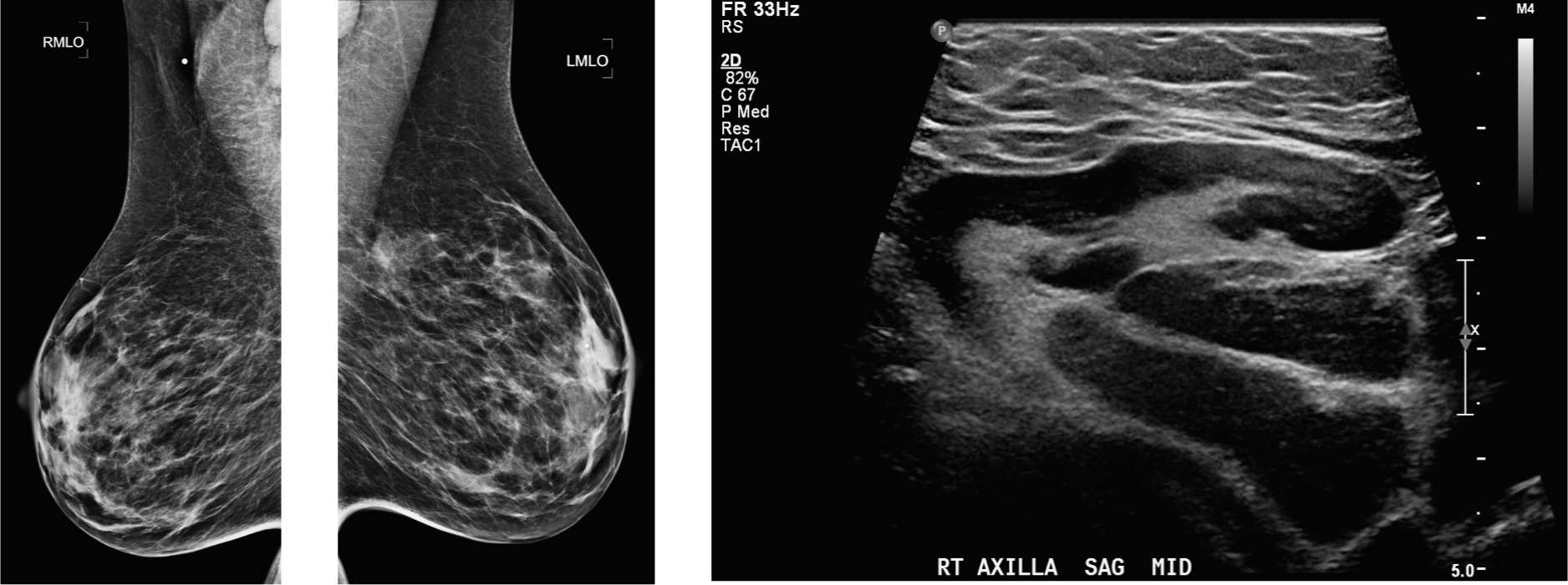
Axilla ultrasound shows one oval solid node with loss of the normal hilum, and a second with diffuse thickening of the cortex and effacement of the hilum.
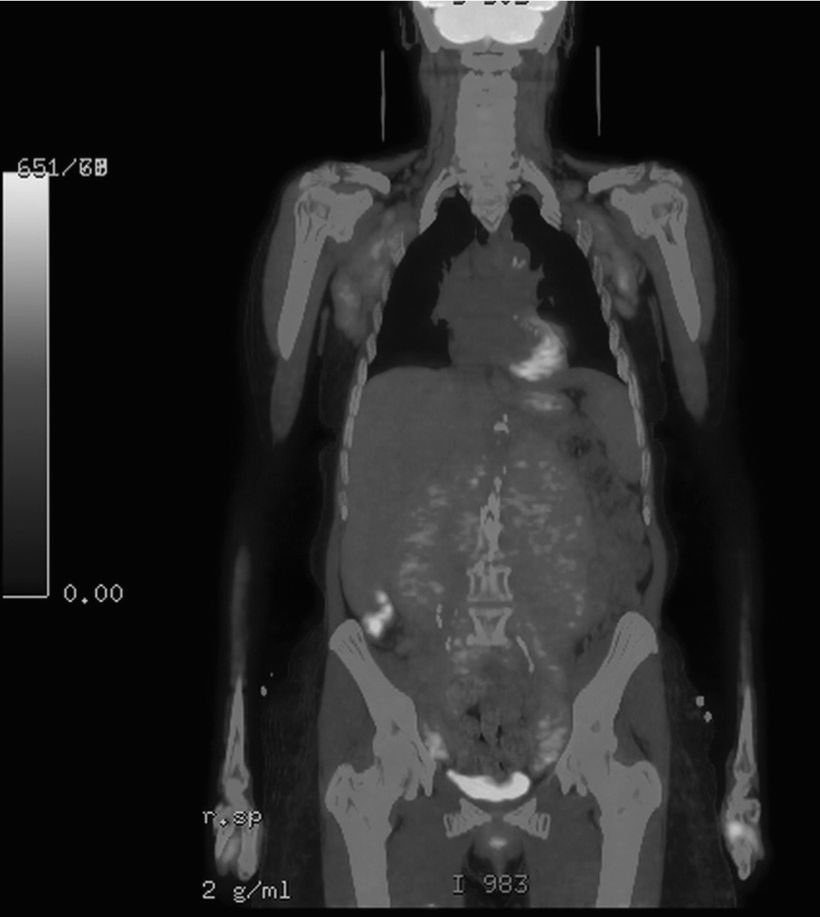
Note multiple enlarged lymph nodes in both axillae.
Answers
1. These lymph nodes are abnormal and do not look like lymphatic spread from a breast cancer. If the patient is with a known lymphoma and under treatment, you could use BI-RADS 2: benign for the breasts, but make a note of the axillary findings. If not known about, then a BI-RADS 0 could be used to get the patient seen, and ultrasound of the axilla performed and possibly biopsied so that they can be passed on to the hematologists.
2. In the setting of likely lymphoma, following a needle biopsy, a PET/CT may give the most staging information before a decision is made.
3. HIV-related lymphadenopathy, systemic inflammatory condition, and lymphoma/chronic lymphocytic leukemias can present with nodes. Inflammatory breast cancer usually presents with unilateral lymphadenopathy. Breast abscesses can also present as unilateral lymphadenopathy. Pelvic abscess does not usually present with axillary nodes.
4. NHL can arise from any of the T or B line white cells, progenitors, or more mature cells; 10% to 35% of patients have extranodal primary lymphoma at the time of presentation.
5. Very uncommon as breast primary, but breast commonly involved when known systemic lymphoma. Painless breast mass usually affecting the right breast; 30% to 40% have ipsilateral axillary adenopathy; average age 55 to 60 years, and right breast more common than left.
Suggested Readings
Gorkem SB, O’Connell AM. Abnormal axillary lymph nodes on negative mammograms: causes other than breast cancer. Diagn Interv Radiol. 2012;18(5):473-479.
Valente SA, Levine MD, Silverstein MD, et al. Accuracy of predicting axillary lymph node positivity by physical examination, mammography, ultrasonography, and magnetic resonance imaging. Ann Surg Oncol. 2012;19(6):1825-1830.
Walsh R, Kornguth PJ, Soo MS, Bentley R, DeLong DM. Axillary lymph nodes: mammographic, pathologic, and clinical correlation. AJR Am J Roentgenol. 1997;168(1):33-38.
Palpable abnormality
1. What is the finding on the diagnostic mammogram?
2. What is the next step in the workup of the patient?
3. If ultrasound does not show any abnormality, what is the next step?
4. What would be the next step if ultrasound demonstrates hypoechoic nodule with internal echoes?
5. What is the definition of a simple cyst—if that is the ultrasound finding what is the next step?
Simple cyst 1307
Case ranking/difficulty: ![]() Category: Diagnostic
Category: Diagnostic
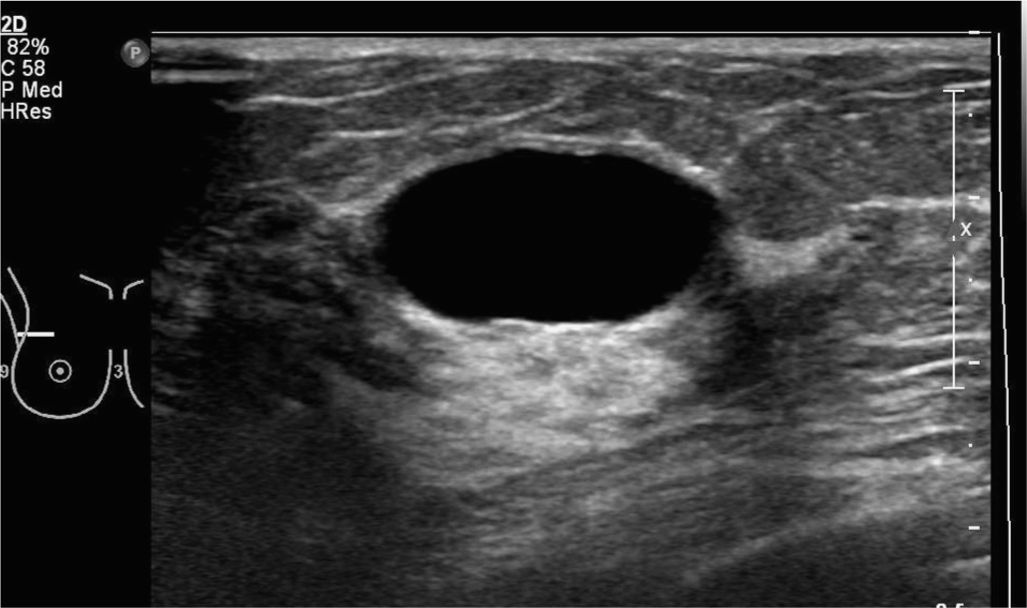
Gray-scale ultrasound demonstrating “anechoic,” “well-circumscribed” mass with “posterior acoustic enhancement.”
Gray-scale ultrasound demonstrating simple cyst.
Answers
1. Mammogram of right breast, including spot compression views, does not show any definite abnormality.
2. Next step in workup is targeted ultrasound directed to the right upper outer quadrant.
3. If ultrasound does not show abnormality, the final assessment is BI-RADS 1 negative, and a sentence should be added that “further assessment of the palpable abnormality should be based on clinical grounds.” If patient is high risk or if the clinical findings are overwhelming and the breast parenchyma is dense and might obscure abnormality, MRI might be an option as problem-solving tool.
4. In case of corresponding hypoechoic mass with internal echoes but without flow on duplex, this is called “complicated cyst” and cyst aspiration should be performed. Since the mass was not seen on mammogram, there is no need to repeat mammogram. Alternative could be to call “complicated cyst” “probably benign” and perform follow-up ultrasound in 6 months, another after 6 months, and then after 1 year.
5. Simple cyst is defined as round and oval “well-circumscribed,” “anechoic” mass with “posterior acoustic enhancement.” This is the description of the finding seen on this particular patient. Assessment is BI-RADS 2, benign, and patient can return to normal screening exam.
Suggested Readings
Berg WA, Campassi CI, Ioffe OB. Cystic lesions of the breast: sonographic-pathologic correlation. Radiology. 2003;227(1):183-191.
Dennis MA, Parker SH, Klaus AJ, Stavros AT, Kaske TI, Clark SB. Breast biopsy avoidance: the value of normal mammograms and normal sonograms in the setting of a palpable lump. Radiology. 2001;219(1):186-191.
Rinaldi P, Ierardi C, Costantini M, et al. Cystic breast lesions: sonographic findings and clinical management. J Ultrasound Med. 2010;29(11):1617-1626.
Screening—asymptomatic
1. What BI-RADS classification should be used here?
2. What are the potential pathologies based on the imaging?
3. What should be the next imaging investigation?
4. How should the lesion be managed if it turns out to be a cystic lesion?
5. If you aspirate a cyst, should you send the fluid for cytology?
Multiple cysts 582
Case ranking/difficulty: ![]() Category: Screening
Category: Screening
Answers
1. This is a characteristic finding, where using the ‘multiple masses’ finding note allows you to give this a BI-RADS 2. If you are uncertain about any of the masses, with indistinct margins, or the mass is partially obscured, you should give the patient a BI-RADS 0 and perform a diagnostic workup to include spot views and ultrasound scanning.
2. The most common cause of these findings are cysts and fibroadenomas, sometimes a mix of both. Metastases have circumscribed margins and should be considered in the presence of a known OTHER cancer, which could potentially metastasize to the breast. Rarely a triple negative ductal cancer may present as a circumscribed mass, but does not tend to have the appearances as of this exam.
3. If you have not used the multiple masses, and given a BI-RADS 2, then the next test should be a routine follow-up mammogram (1 year in the United States). If the patient has a palpable lump being worked up, then an ultrasound may be the best first-line investigation, as we need to confirm whether the lump is cystic or solid. For margins, a single tomosynthesis projection is showing promise in the workup of women with masses.
4. Simple cysts can come and go rapidly, changing even day to day. Some cysts remain over a long period, developing thick proteinaceous debris, which may show as a snowstorm appearance on ultrasound. Sometimes, this debris is adherent to a cyst wall, and prompt shortterm surveillance or even biopsy. Historically, cysts were sometimes surgically excised.
5. Cyst aspirations are not routinely performed anymore. It may help if the fluid is bloody, but this is usually due to a traumatic tear of a small vessel around the cyst wall, and not related to the cyst at all (a bloody tap—especially at the end of aspiration).
Suggested Readings
Lister D, Evans AJ, Burrell HC, et al. The accuracy of breast ultrasound in the evaluation of clinically benign discrete, symptomatic breast lumps. Clin Radiol. 1998;53(7):
490-492.
Shetty MK, Shah YP. Sonographic findings in focal fibrocystic changes of the breast. Ultrasound Q. 2002;18(1):35-40.
Screening—asymptomatic
1. What BI-RADS classification should be used here?
2. What is the most likely pathology based on the imaging?
3. What is the next best imaging test?
4. What type of intervention would you recommend?
5. What is the risk of breast cancer in patients with multiple cysts?
Multiple masses—cysts or fibroadenomas 586
Case ranking/difficulty: ![]() Category: Screening
Category: Screening
Multiple simple cysts in both breasts confirmed on ultrasound exam.
Answers
1. The multiple, noncalcified, circumscribed, bilateral masses are likely due to fibroadenomas or cysts. A BI-RADS 2, benign, note is appropriate.
2. The findings are most likely cysts or fibroadenomas, although rarely you can get multiple phyllodes tumors in both breasts; the key here is that those lesions are not stable and tend to be rapidly growing. Metastases to the breast can look identical to this, but is in the setting of a known “other” cancer that has the potential to metastasize to the breast.
3. If you wish to work this up, then ultrasound on its own can distinguish between solid and cystic masses. Some claim that tomosynthesis has a role here, but the data are currently lacking. As this is a benign finding, routine mammograms are indicated.
4. No intervention is required for multiple benign lesions.
5. There was a reported statistical relationship between simple cysts and subsequent breast cancer, likely related to the sensitivity of breast tissue to circulating estrogens, but this has not been validated, and does not reach the risk levels associated with hyperplastic or borderline neoplastic lesions of the breast.
Suggested Readings
Berg WA, Sechtin AG, Marques H, Zhang Z. Cystic breast masses and the ACRIN 6666 experience. Radiol Clin North Am. 2010;48(5):931-987.
Chang YW, Kwon KH, Goo DE, Choi DL, Lee HK, Yang SB. Sonographic differentiation of benign and malignant cystic lesions of the breast. J Ultrasound Med. 2007;26(1):47-53.
Heinig J, Witteler R, Schmitz R, Kiesel L, Steinhard J. Accuracy of classification of breast ultrasound findings based on criteria used for BI-RADS. Ultrasound Obstet Gynecol. 2008;32(4):573-578.
Screening—asymptomatic
1. What BI-RADS classification should be used here?
2. What is the inheritance pattern of neurofibromatosis?
3. Which chromosome is affected by the NF-1 mutation?
4. What type of breast biopsy should be performed to confirm the diagnosis?
5. What are the other supportive features for the diagnosis of NF-1?
Von Recklinghausen disease—type 1 neurofibromatosis 1864
Case ranking/difficulty: ![]() Category: Screening
Category: Screening
Close-up view of irregular, lobulated, overgrowth of nipple, and two circumscribed superfi cial masses.
Answers
1. This is a benign finding, and therefore a BI-RADS 2 assessment would be appropriate.
2. The defect on chromosome 17 arises by autosomal dominant genetics, but 50% occur by spontaneous mutation.
3. Chromosome 17 has the locus for the mutated gene affected in NF-1.
4. No biopsy of the breast needs to be performed to confirm the diagnosis. The diagnosis is usually obvious on physical examination. Also, they may be under preexisting care for known neurofibromatosis.
5. The NF-1 gene is on chromosome 17 and affects cell signaling. As a result, there is overgrowth causing benign tumors and also scoliosis (in 20%) or other limb deformities. Epilepsy is observed in approximately 7% of patients. Learning difficulties or other psychological issues are common. The gastrointestinal system is generally not involved with tumors in NF-1. Tumors are more common in the nervous system with plexiform neurofibromas, and schwannomas. Pheochromocytoma is a complication.
Suggested Readings
Cao MM, Hoyt AC, Bassett LW. Mammographic signs of systemic disease. Radiographics. 2012;31(4):1085-1100.
Goksugur N, Gurel S. Neurofibromatosis of nipple-areola complex. Breast J. 2012;17(4):424.
Sherman JE, Smith JW. Neurofibromas of the breast and nipple-areolar area. Ann Plast Surg. 1981;7(4):302-307.
Screening mammogram—status post–right lumpectomy many years ago
1. What is the significance of the lesion in the right breast?
2. What is the diagnosis?
3. How can fat necrosis appear on mammogram?
4. If there is concern for recurrent malignancy, what would be the next step?
5. If there is remaining concern for recurrent malignancy, what would be the next step?
Fat necrosis 737
Case ranking/difficulty: ![]() Category: Screening
Category: Screening
Old mammogram, right spot compression CC view demonstrating fat necrosis.
Current mammogram, right spot compression CC view demonstrating retraction of the scar and development of “coarse, heterogenous” calcifications.
Answers
1. Focal area does contain fat and is a benign finding. This is a benign lesion BI-RADS 2. Correlate with history—patient had lumpectomy.
2. This is typical appearance of scar after lumpectomy with fat necrosis.
3. Fat necrosis can present a wide variety of morphology, of which some are more pathognomonic and some are more difficult to distinguish from possible malignancy. If there is fat within the focal finding or the abnormality contains “coarse and heterogeneous” calcifications, it is relatively specific for fat necrosis. However, if the microcalcification or the mass is spiculated, it is unspecific and sometimes biopsy is warranted.
4. Diagnostic mammogram with spot compression MLO and CC views or, if calcifications are the concern, workup with magnification ML and CC views. In some breast centers, all patients after lumpectomy receive diagnostic mammograms in the first place, which often times includes spot compression or magnification views in the first place.
5. The best test for questionable recurrent malignancy would be to perform breast MRI—however, there should be at least 6-month time interval between surgery and MRI; otherwise, it is difficult to distinguish postoperative enhancement due to granulation tissue from enhancement as a result of recurrent tumor.
Suggested Readings
Hogge JP, Robinson RE, Magnant CM, Zuurbier RA. The mammographic spectrum of fat necrosis of the breast. Radiographics. 1995;15(6):1347-1356.
Taboada JL, Stephens TW, Krishnamurthy S, Brandt KR, Whitman GJ. The many faces of fat necrosis in the breast. AJR Am J Roentgenol. 2009;192(3):815-825.
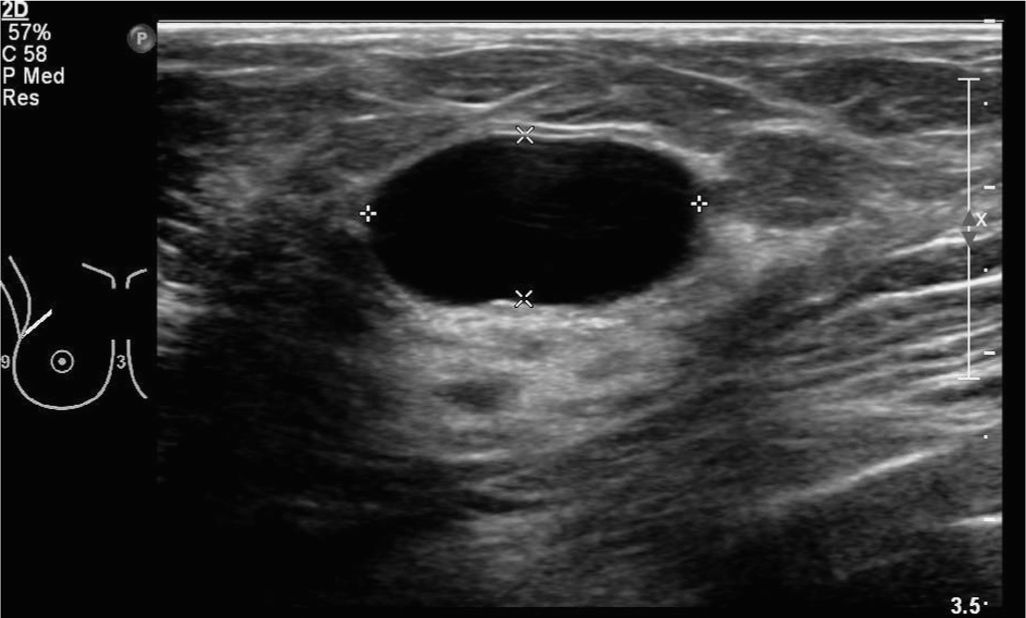
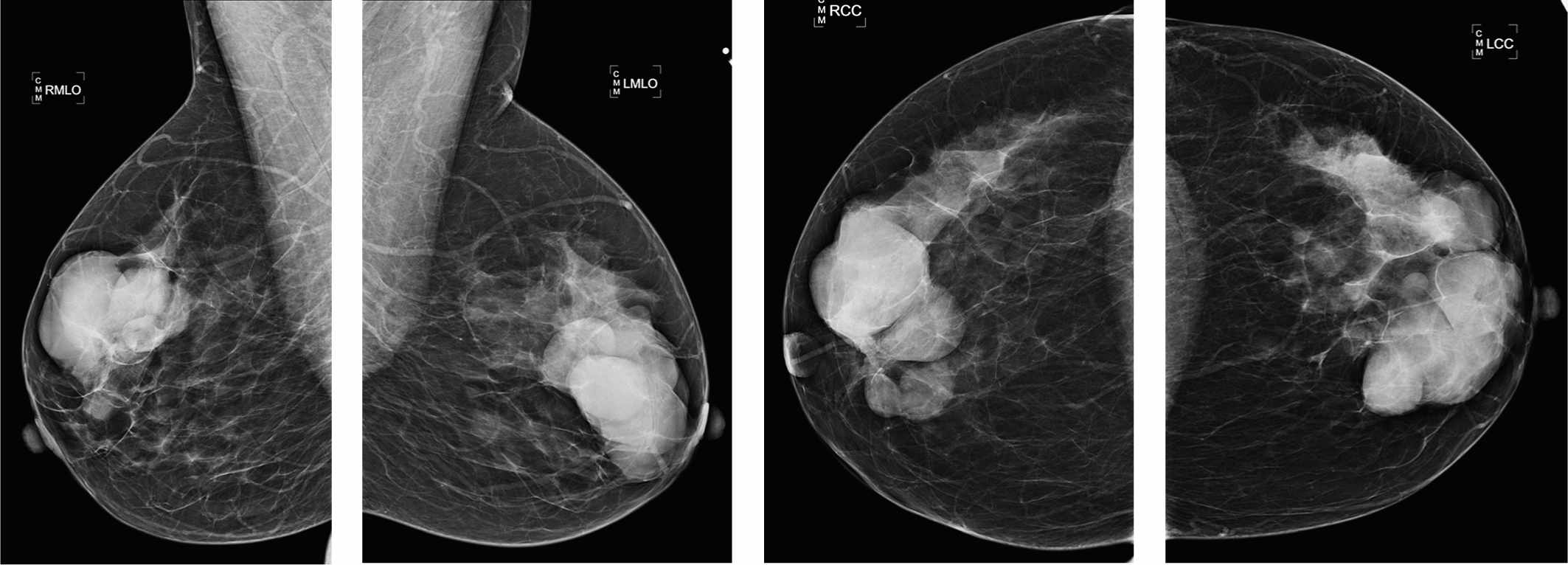
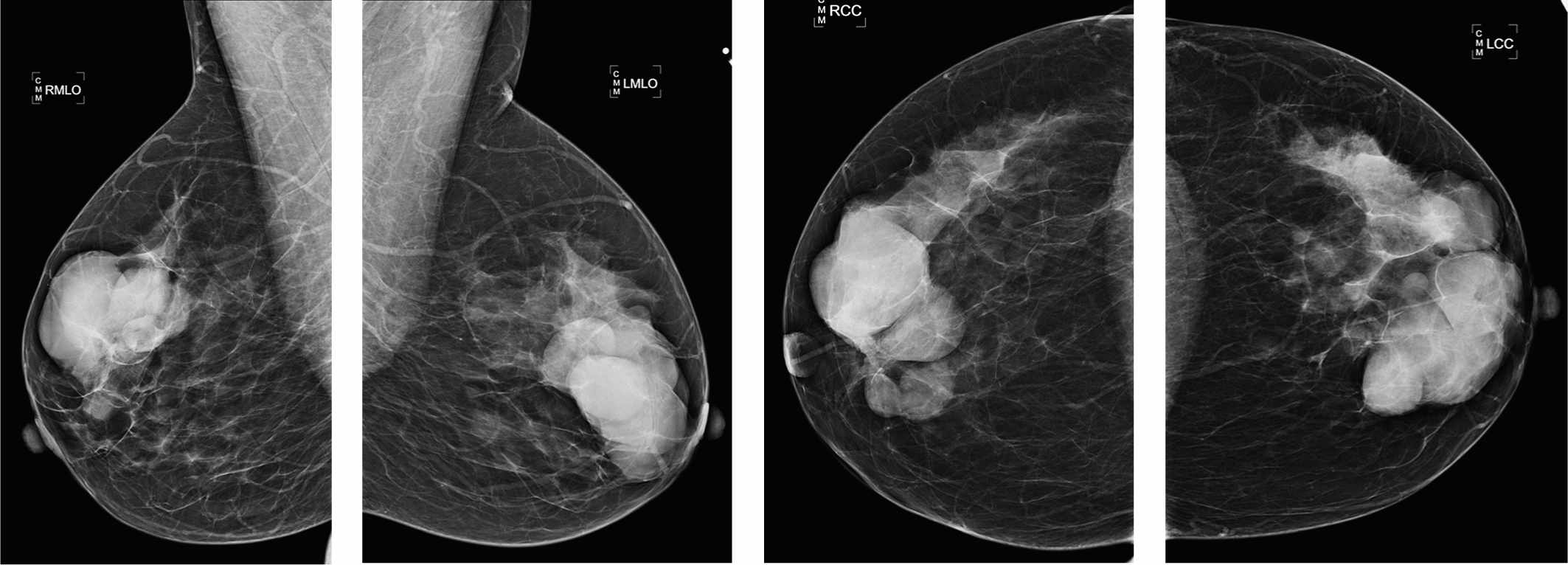
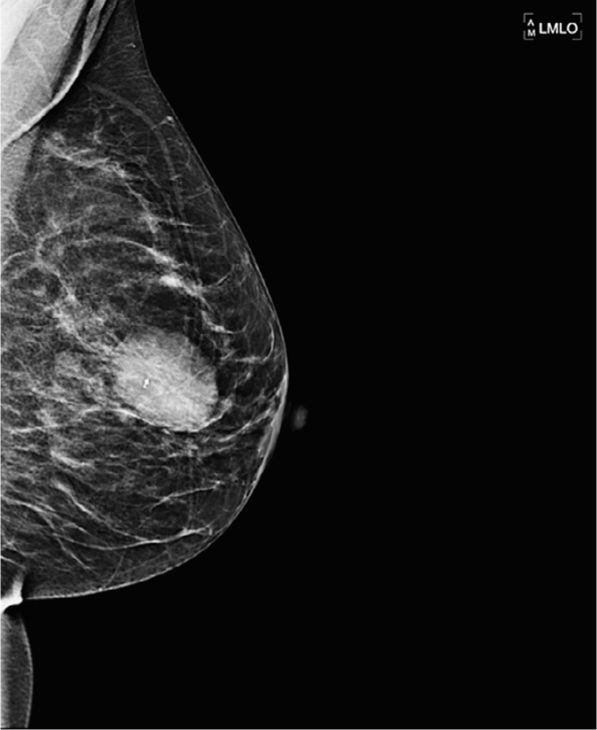
Palpable lump in the left breast
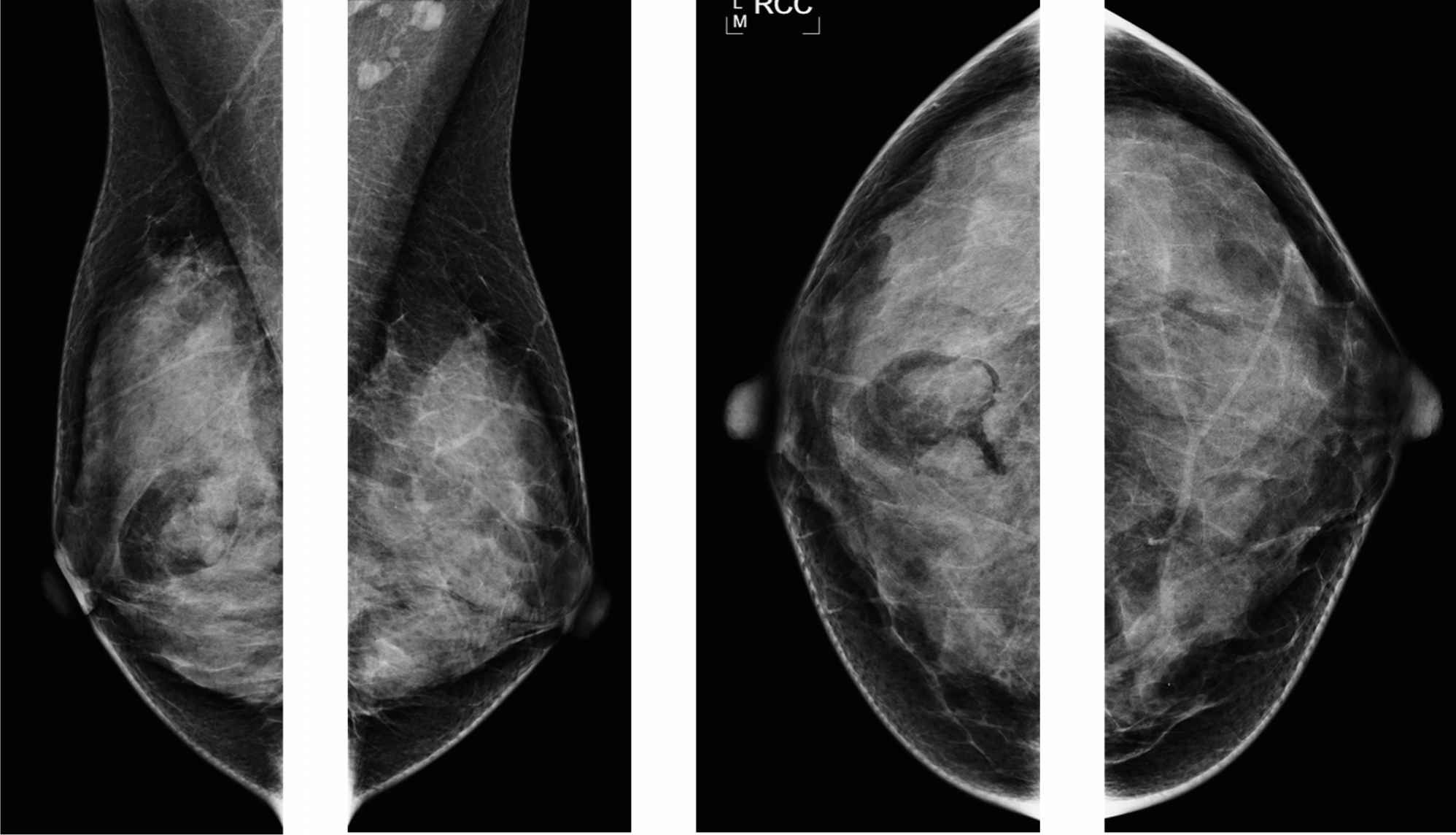
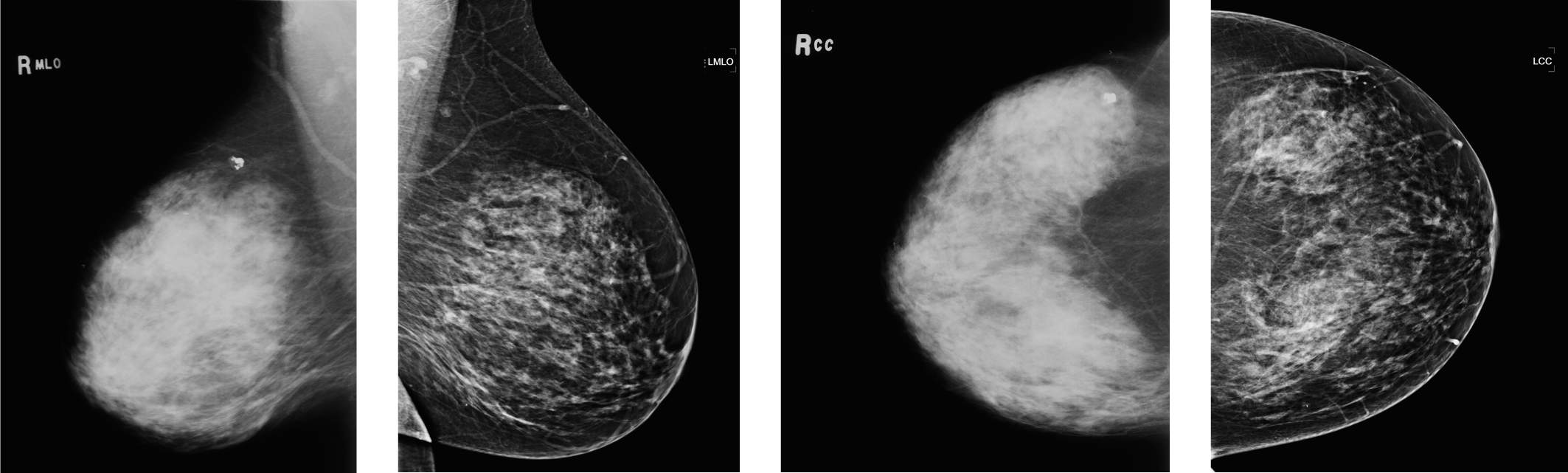
Right MLO.
Right CC.
Left CC.
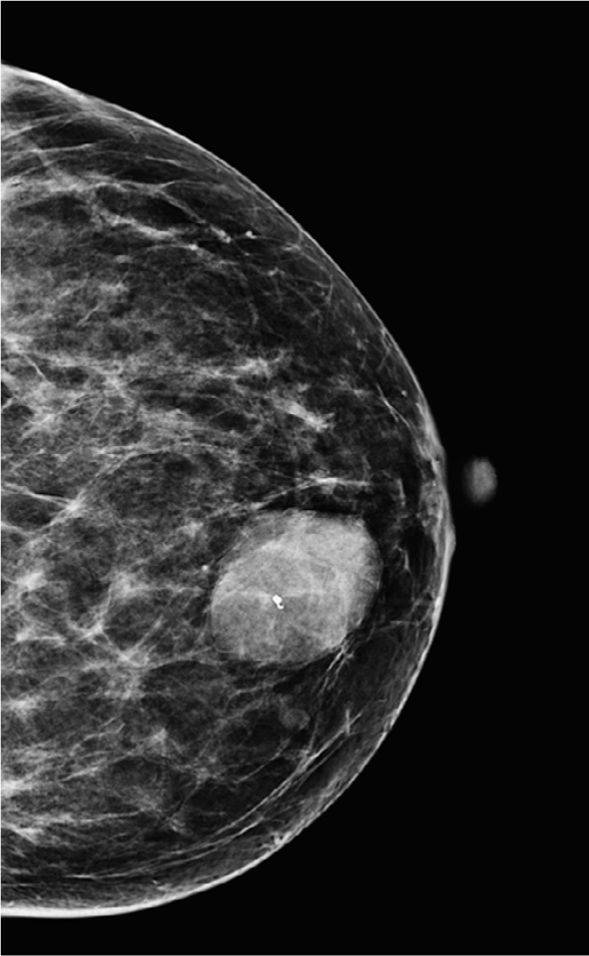
Left MLO.
1. What is the BI-RADS category for this diagnostic exam?
2. Which of the following are the Stavros benign criteria?
3. What is the risk of malignancy in a circumscribed mass in a woman younger than 25 years?
4. Which of the new technologies in breast imaging is likely to help our diagnosis of fibroadenoma?
5. What types of biopsies can make the diagnosis of fibroadenoma?
Fibroadenoma in young women 602
Case ranking/difficulty: ![]() Category: Screening
Category: Screening
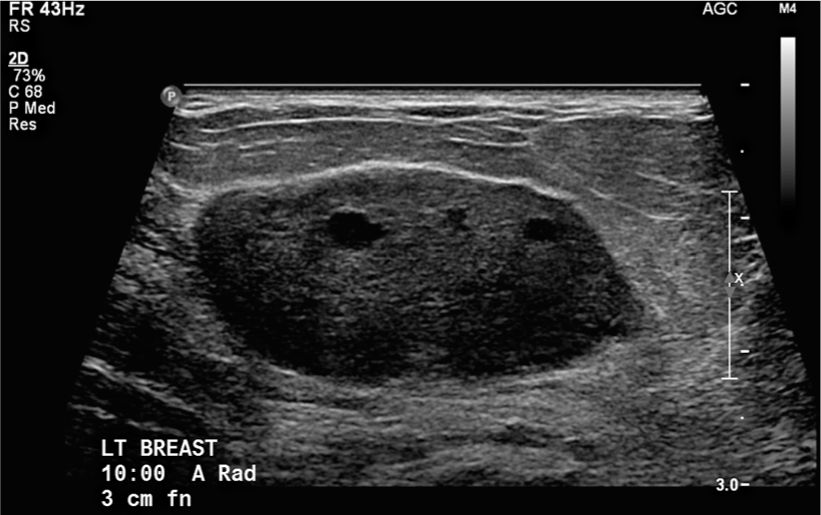
Ultrasound shows an “oval mass” with a “narrow zone of transition” (circumscribed). The echo texture is predominantly homogeneously hypoechoic, with some smaller cystic spaces within.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree