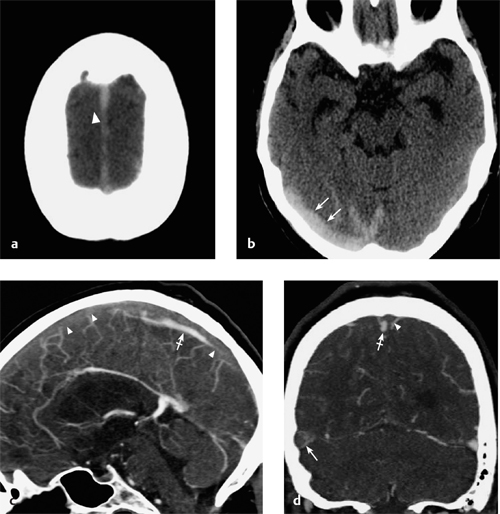
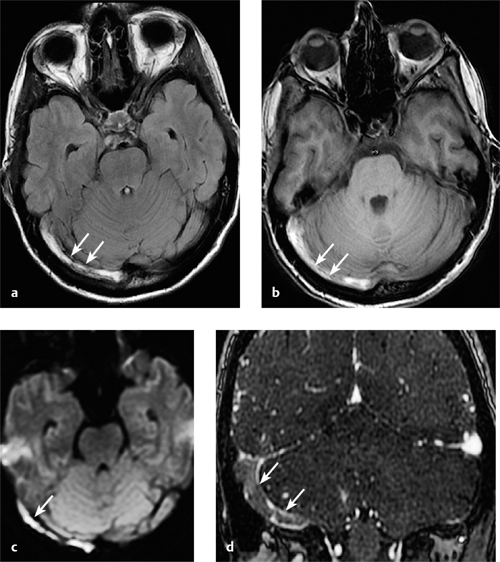
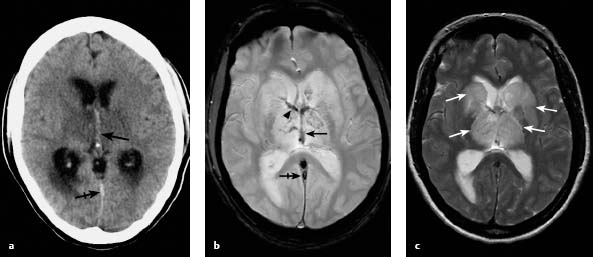
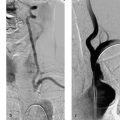
5 Cerebral Venous and Sinus Thrombosis Cerebral venous and sinus thrombosis (CVST) is a relatively rare but important cause of stroke. It accounts for less than 1% of all strokes in Europe. The estimated annual incidence of CVST is ~3–4 cases per 1 million in adults, and ~7 cases per 1 million in newborns, infants, and children. The disease may occur in all age groups and in both sexes, although young and middle-aged women (< 40 years) are most commonly affected (Stam 2005). To date, a wide variety of predisposing factors as well as several important direct causes for CVST are known. The most important risk factors and causes of CVST are acquired or congenital coagulation disorders; oral contraceptive use; pregnancy; lactation; and ear, nose, and throat infections. Over 40% of patients are found to have two or more predisposing factors, but 15–20% of all patients have no identifiable risk factors (Ferro et al. 2009). Three subtypes of CVST are distinguished according to the location of the thrombosis—that is, the venous structures affected. This distinction is clinically relevant because the subtypes differ in their symptoms and prognosis. Also, the value of different imaging sequences differs considerably depending on the site of the thrombosis (Linn and Brückmann 2010). • Sinus thrombosis: This refers to the thrombotic occlusion of one or more of the dural venous sinuses. Sinus thrombosis is by far the most common form of CVST. The superior sagittal sinus is most often affected, followed by the transverse sinus (Ferro et al. 2009; Figs. 5.1 and 5.2). • Deep cerebral venous thrombosis: This refers to thrombosis of the internal cerebral veins, vein of Galen, and/or the basal veins of Rosenthal and their tributaries. Most authors also include the straight sinus with the deep cerebral veins. Involvement of the deep cerebral veins is present in ~10% of all patients with CVST. It is usually accompanied by sinus thrombosis. Isolated thrombosis of the deep cerebral veins is much less common (Ferro et al. 2004; Fig. 5.3). • Cortical vein thrombosis: Thrombosis of the cortical veins refers to a thrombosis of the superficial veins of the cerebral convexities including the vein of Labbe. Like deep cerebral vein thrombosis, cortical vein thrombosis occurs most often in combination with sinus thrombosis. In these cases, the superior sagittal sinus is most often involved. Cortical vein thrombosis often develops secondary to superior sagittal sinus thrombosis due to retrograde spread of thrombotic material from the sinus into the cerebral veins draining into the sinus (Fig. 5.4). This process most commonly affects the frontal cortical veins, followed by the parietal veins (Linn et al. 2010). Isolated thrombosis of one or more cortical veins is very rare and has been described only in isolated case reports and small case series. Evaluation of the cortical veins poses a special diagnostic challenge to the radiologist. This is mainly because the cortical veins, unlike the dural sinuses and deep cerebral veins, show striking intra- and interindividual variations in number, diameter, and anatomic location. These hamper the interpretation of angiographic studies. Therefore, these techniques are of limited used for the evaluation of the cortical veins and cannot serve as gold standard technique. More recently, T2*-weighted gradient-echo sequences have proven very effective for this application (see below and Fig. 5.4). Consequently, the number of reported cases has risen sharply in recent years. Today many authors believe that cortical vein involvement is much more common than previously described. It is also reasonable to assume that isolated cortical vein thrombosis is not as rare as previously thought but simply went undetected in earlier studies. In contrast to arterial strokes, the symptoms of CVST usually have a subacute onset. The clinical presentation is nonspecific, and heterogeneous. The most common initial, very unspecific symptom is severe headache, which occurs in 75–90% of all patients. In addition to headache, patients often develop other signs of increased intracranial pressure such as dizziness, nausea, and visual disturbances. Other symptoms of CVST depend basically on the location and extent of the thrombosis (Ameri and Bousser 1992; Stam 2005). Other important factors that determine clinical presentation are patient age, the presence of concomitant parenchymal changes, and the interval from symptom onset to diagnosis. Focal neurologic deficits can occur, depending on the site of the venous occlusion, and may include cranial nerve deficits and focal seizures. Fig. 5.1a-d Sinus thrombosis on non-contrast CT and CTA. A 70-year-old woman who suffered from predominantly right-sided headaches for several days due to thrombosis of the superior sagittal sinus (arrowheads in a, c, and d) and right transverse sinus (arrows in b and d). a, b Noncontrast CT scans (a, b) show a hyperdense vessel sign (cord sign) in the affected sinuses (arrows and arrowheads in a and b, respectively) as a direct sign of thrombosis. c, d CT angiography. Sagittal and coronal multiplanar reconstruction from MPRs (c and d) demonstrate the thrombosis as a filling defect in the affected vessels (arrows and arrowheads in c and d, respectively). The crossed arrows in c and d indicate a prominent cortical vein that drains into the thrombosed superior sagittal sinus. Fig. 5.2a-d Direct MR signs of subacute right transverse sinus thrombosis (arrows in a-d) in a 32-year-old man who had been symptomatic (headaches and nausea) for 10 days, consistent with a subacute phase of thrombosis. a FLAIR sequence. The thrombotic material in the right transverse sinus (arrows) appears hyperintense. b T1w sequence. Again, the thrombotic material in the right transverse sinus (arrows) appears hyperintense. c The thrombotic material also has high signal intensity on diffusion-weighted MRI (arrow). d Coronal reconstruction of contrast-enhanced MRA shows no contrast filling of the affected sinus (arrows). Fig. 5.3a–c Direct and indirect signs of deep cerebral vein thrombosis in a 32-year-old woman with thrombosis of the deep cerebral veins (arrows in a and b), thalamostriate veins (arrowhead in b), and straight sinus (crossed arrows in a and b) causing bilateral edema in the thalamus and basal ganglia (arrows in c). a The thrombotic material shows high attenuation on noncontrast CT (dense vein sign, arrow). b The thrombotic material has low signal intensity on T2*w MRI (arrow, arrowhead, crossed arrow). c T2-weighted sequence vividly defines the extent of associated venous edema (arrows). Fig. 5.4a–c Value of T2*w gradient-echo MRI for detecting cortical vein thrombosis. A 45-year-old woman with thrombosis of the superior sagittal sinus (arrowheads in a and b) and bilateral frontal cortical veins (arrows in a and b). Right frontal hemorrhage due to venous stasis (crossed arrow in c) is present as an indirect sign of thrombosis. Cortical vein involvement is clearly appreciated only in the T2*w sequence where the affected veins appear as very hypointense tubular structures. The other MR sequences (not shown) showed direct signs of thrombosis only in the superior sagittal sinus. CVST is an important differential diagnosis that should be particularly noted in the following patient groups: • Young and middle-aged patients with very severe headache of recent onset • Young and middle-aged patients with stroke symptoms in the absence of known risk factors • Patients with signs of increased intracranial pressure • Patients with hemorrhagic stroke Involvement of the deep cerebral veins or cortical veins significantly affects the clinical presentation. Patients with deep cerebral vein thrombosis present with a decreased level of consciousness in over 70% of cases (Pfefferkorn et al. 2009). Cortical vein thrombosis is often characterized by focal or generalized seizures, hemiparesis, aphasia, hemianopsia, or other focal neurologic deficits. Symptoms of increased intracranial pressure may be absent, especially when thrombosis is limited to the cortical veins (Jacobs et al. 1996). Normal D-dimer levels have a high negative predictive value for suspected CVST. Nevertheless, D-dimer levels may be normal in up to 25% of cases, especially in patients with isolated thrombosis of the deep cerebral veins. False-negative results in these cases are presumably due to the relatively small thrombus volume (Pfefferkorn et al. 2009). The outcome of CVST has improved significantly in recent decades. This is due largely to improvements in imaging modalities and effective treatment methods using intravenous or subcutaneous low-molecular-weight heparin. Today CVST has a very good prognosis when diagnosed early, with complete recovery achieved in 80% of patients (Diener and Putzki 2008). It should be added, however, that the interval from symptom onset to definitive diagnosis still averages 7 days, despite modern imaging modalities (Stam 2005). This interval may be considerably longer in patients with deep cerebral vein thrombosis, in males, and in patients who present only with signs of increased intracranial pressure. This is due mainly to the very unspecific and variable symptoms of the disease and its delayed or subacute clinical onset, especially in the small subset of patients who have normal D-dimer levels. This delay accounts for the poorer outcomes in ~10–15% of patients with CVST. Besides a delay in diagnosis, there are other risk factors that are associated with a poor outcome: advanced age, male gender, parenchymal hemorrhage secondary to venous congestion, involvement of the deep cerebral veins or right transverse sinus, and the presence of CNS infection or an intracerebral tumor as a precipitating cause (Ferro et al. 2004). Although involvement of the deep venous system is a risk factor for a poor or even fatal course, a recent study found that even this condition has a better outcome today than in earlier studies. It was shown that 75% of patients improved significantly when treated with intravenous or subcutaneous low-molecular-weight heparin, achieving a modified Rankin Score (mRS) of 2 or higher, signifying little or no functional disability. The remaining 25% of patients deteriorated with progressing coma, even though most of them received endovascular recanalization therapy (Pfefferkorn et al. 2009). Imaging studies can reveal both direct and indirect signs of CVST, regardless of the site of the venous occlusion. Direct signs are signal or density changes caused by the thrombotic material itself; indirect signs are associated signal abnormalities in the brain parenchyma. • Direct signs: “Positive” visualization of the thrombus in an affected vein or sinus by noncontrast CT or MRI, or “negative” visualization of the thrombus as a filling defect in digital subtraction angiography (DSA), CT angiography (CTA), or other contrast-enhanced images, as well as absence of a flow signal in flow-sensitive venous time-of-flight MR angiography (TOF MRA). • Indirect signs: The following parenchymal changes can be found as indirect signs of CVST on CT and MR images: venous edema or venous infarction, subarachnoid hemorrhage, and parenchymal hemorrhage due to venous congestion. In contrast to arterial strokes, the edema in CVST typically does not conform to arterial territories but crosses territory boundaries. Most often a vasogenic edema is found, while acute ischemic arterial infarctions typically present with a cytotoxic edema. In the case of dural sinus or cortical vein thrombosis, the edema typically affects the cortex and/or the adjacent subcortical white matter. By contrast, deep cerebral vein thrombosis is typically associated with unilateral or most often bilateral edema or venous infarction in the thalamus and basal ganglia (Linn and Brückmann 2010; see Fig. 5.3). If parenchymal hemorrhage is detected at the time of diagnosis, it correlates with more severe initial symptoms and a poorer outcome (Ferro et al. 2004). Long considered the diagnostic gold standard for CVST, DSA no longer has a significant role in the diagnosis of this disease, having been largely replaced by CTA and MRI. Note Today DSA is no longer a standard tool for suspected CVST but is reserved for cases being considered for interventional treatment such as local thrombolysis or mechanical recanalization (Diener and Putzki 2008). However, DSA is still superior to MRI and CTA in its spatial and temporal resolution and can provide very precise dynamic information, especially on collateral venous drainage pathways. This capability can yield important additional information in selected cases. For the cortical veins, a few authors still claim that DSA can provide higher sensitivity than other modalities, although no systematic data have been published to support this hypothesis. In patients with isolated thrombosis of one or more cortical veins, DSA may show an “absent” cortical vein and/or a partially opacified vein with an abrupt cutoff. Dilated cortical veins functioning as collaterals may be visible in the surrounding area. The value of this sign is limited, however, by the large intra- and interindividual variations of the number and anatomic location the cortical veins as described above. As a result, the direct signs of thrombosis on DSA are of limited value and the diagnosis of cortical vein thrombosis by DSA is based mainly on the following indirect signs: • Detection of a focal delay in venous drainage • Signs of venous congestion in parenchyma drained by the occluded vein • Detection of cortical collaterals, also known as “corkscrew vessels” Caution The above limitations of DSA for evaluating the cortical veins also apply to other angiographic techniques including CTA and the various MRA techniques. Today MRI is regarded as the gold standard for the diagnosis of CVST (Stam 2005), although CTA is increasingly found to be equivalent to MRA alone (see below; Diener and Putzki 2008). Cerebral venous thrombosis shows rather complex signal characteristics on MRI depending on the age of the thrombus (acute, subacute, or chronic stage) and on the type of MRI sequence used. In contrast, the location of the thrombus does not influence its imaging appearance—that is, the signal characteristics of the thrombotic material are the same regardless of whether the dural sinuses, deep cerebral veins, or cortical veins are affected (Linn and Brückmann 2010). Note A detailed knowledge of the complex, time-dependent signal characteristics of the venous thrombus is essential for the correct interpretation of MR images in CVST.
Introduction
Epidemiology
Risk Factors
Subtypes
Clinical Signs and Symptoms
Laboratory Findings
Prognosis and Outcome
Imaging Studies
Direct and Indirect Signs of Cerebral Venous and Sinus Thrombosis
Digital Subtraction Angiography
Magnetic Resonance Imaging
Direct Signs of CVST on MRI
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Cerebral Venous and Sinus Thrombosis