Spinal cord diseases generally have distinctive clinical findings that reflect dysfunction of particular sensory or motor tracts. The abnormalities on MR images reflect the pathologic changes that occur in the affected pathways. The complexity and the wide spectrum of diseases affecting the spinal cord require a profound knowledge of neuropathology and exactly tuned imaging strategies. This article describes and illustrates the clinical and imaging characteristics in various demyelinating and infectious conditions of the spinal cord.
Spinal cord diseases generally have distinctive clinical findings that reflect dysfunction of particular sensory or motor tracts. The abnormalities on MR images reflect the pathologic changes that occur in the affected pathways. The complexity and the wide spectrum of diseases affecting the spinal cord require a profound knowledge of neuropathology and exactly tuned imaging strategies. This article describes and illustrates the clinical and imaging characteristics in various demyelinating and infectious conditions of the spinal cord.
Demyelinating diseases of the spinal cord
Multiple sclerosis
Multiple sclerosis (MS) is a chronic inflammatory demyelinating disease of the central nervous system (CNS). Recent data suggest that MS is a T-cell–mediated disease with secondary macrophage activation. The pathologic hallmark of MS is inflammatory demyelination, which can lead to irreversible tissue loss or partial demyelination in cases where reparative processes occur with subsequent remyelination. Three mechanisms of tissue injury in MS have been proposed: immunologic, excitotoxic, and metabolic . The spinal cord is frequently involved in MS, with cord lesions found in up to 99% of autopsy cases . The first pathologic descriptions of the macroscopic distribution of MS lesions in the spinal cord were by Carswell in 1838 and Cruveilhier in 1841 . In 70% to 80% of patients who have MS, cord abnormalities are detected on T2-weighted MR images . MS spinal cord abnormalities can be divided into three main types: (1) focal, well demarcated areas of high signal intensity on T2-WI; (2) diffuse abnormalities seen as poorly demarcated areas of increased signal intensity on T2-WI; and (3) spinal cord atrophy and axonal loss.
Focal lesions
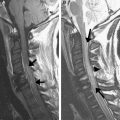
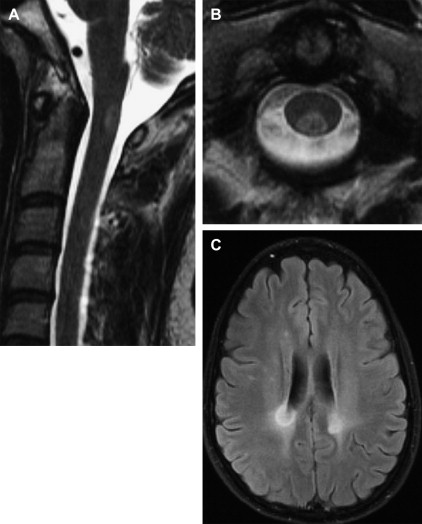
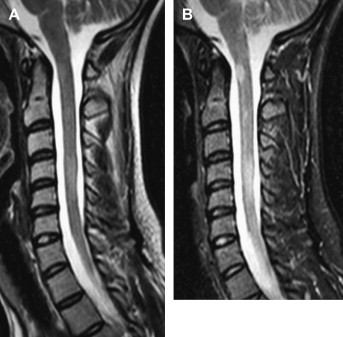
Macroscopically, spinal cord lesions appear elongated in the direction of the long axis of the cord and vary in length from a few millimeters to lesions that extend over multiple segments . MR imaging is the most sensitive technique for detecting MS lesions in the brain and spinal cord. Its role as a tool in the diagnosis and longitudinal monitoring of patients who have MS has been well established in numerous studies . The recent introduction of the McDonald criteria has further strengthened the role of MR imaging in the diagnosis of MS. MS plaques are best seen with T2-weighted MR sequences and are hyperintense on T2-WI and iso-hypointense on T1-weighted MR images. Spinal cord demyelinating plaques present as well circumscribed foci of increased T2 signal that asymmetrically involve the spinal cord parenchyma. They are characteristically peripherally located, are less than two vertebral segments in length, and occupy less than half the cross-sectional area of the cord. On sagittal sections, plaques have a cigar shape and may be located centrally, anteriorly, and dorsally. On axial MR images, the lesions located in the lateral segments have a wedge shape with the basis at the cord surface or a round shape if there is no contact with the cord surface ( Fig. 1 ). The distribution of MS lesions in the spinal cord closely corresponds to venous drainage areas. Cord swelling is usually found only in the relapsing-remitting form of MS . Because acute lesions are associated with transient breakdown of the blood–brain barrier, enhancement may be seen on postcontrast images ( Figs. 2 and 3 ). The incidence of enhancing lesions is significantly lower than in the brain . Sixty-two percent of the plaques occur in the cervical spinal cord. Chronic foci of hypointensity on T1-WI images, known in the brain as “black holes,” are not present in the spinal cord .
Diffuse abnormalities
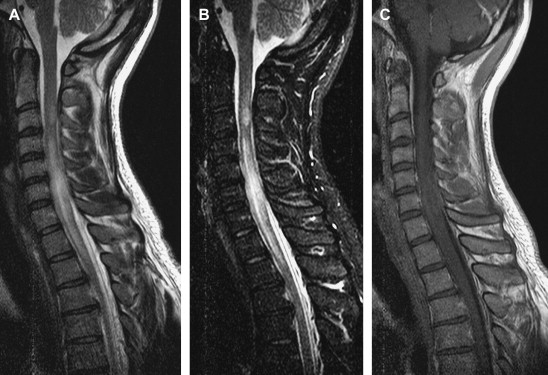
Diffuse abnormalities are more common in primary progressive MS and secondary progressive MS. Diffuse signal changes of the spinal cord are recognized on images as mild intramedullary hyperintensities on T2-weighted MR images ( Fig. 4 ).
Spinal cord atrophy
In addition to plaques and diffuse spinal cord abnormalities, spinal cord atrophy has been recognized for many years ( Fig. 5 ). Axonal degeneration, or an alternative atrophic process, may be responsible for spinal cord atrophy in MS. One recent study has shown that the degree of atrophy varies in different parts of the cord, being more prominent in upper parts of the cord . Studies have also shown that spinal cord atrophy correlates with clinical disability . Analysis of the amount of atrophy revealed a correlation between upper cervical cord and cerebral white matter atrophy and an expanded disability status scale . Significant cerebral and spinal cord volume reductions have been found in all patient subgroups of MS compared with control subjects . Higher rates of atrophy have been reported in relapsing-remitting MS than in secondary progressive forms of the disease . Plaques associated with cord atrophy are more likely to occur with the relapsing-progressive form of MS.

Axonal loss
Postmortem studies have shown convincingly that cord damage is not limited to lesions visible on T2-WI . According to the neuropathologic studies about MS of the spinal cord, axonal loss can be found in 60% to 70% of chronic MS lesions. Magnetic Resonance Spectroscopy studies have shown reduced N-acetyl aspartate in areas of the cord that were normal on conventional MR images. Significant abnormalities in normal-appearing spinal cord have also been observed . Decreased small fiber density was found in one study in the lateral column of the cervical spinal cord of patients who have MS compared with control subjects . Data from recent neuropathologic studies suggest that extensive axonal damage occurs during plaque formation soon after the onset of demyelination . Furthermore, during that process, significant axonal injury is found in the normal white matter. Ongoing, low-burning axonal destruction has also been found in inactive demyelinated lesions in the brain .
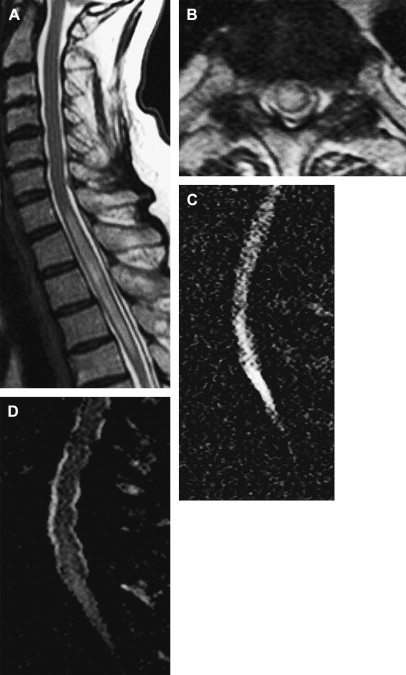
The entire spinal cord should be imaged in patients who have spinal symptoms and who have a known or presumptive diagnosis of MS. Slice thickness should not exceed 3 mm, with a maximum interslice gap of 10% . The imaging protocol should include the following sequences: sagittal T2-WI, T1-WI, axial T2-WI for exact anatomic location of the lesion, and contrast-enhanced T1-WI. Studies have shown the superiority of short-tau inversion-recovery sequences to Fast Spin Echo sequences in the detection of MS lesions in the spinal cord ( Fig. 6 ) . Fast fluid inversion recovery was rated unsatisfactory .
The value of spinal MR imaging in the differentiation of MS from other inflammatory or cerebrovascular disorders has been evaluated in a recent study . Specificity, sensitivity, and positive and negative predictive values for MR imaging were calculated for 66 patients who had other neurologic diseases and 25 patients who had MS. Brain images were abnormal in all patients who had MS but in only 65% of patients who had other brain disorders. Spinal cord abnormality was found in 92% of patients who had MS but in only 6% of patients who had other diseases. With the combination of brain and spinal cord MR imaging in that study, the accuracy of differentiating MS from other disorders reached 95% based on the criteria of Paty and colleagues , 93% based on the criteria of Fazekas and colleagues , and 93% based on the criteria of Barkhof and colleagues .
Diffusion-weighted MR imaging (DWI) has been increasingly used for the evaluation of spinal cord diseases, especially in spinal cord ischemia . Clark and colleagues were the first to use a conventional, cardiac-gated, navigation diffusion-sensitized spin-echo sequence for in vivo DW imaging of the spinal cord. MS lesions were found to have increased rates of diffusivity, with a significantly higher isotropic diffusion coefficient, compared with healthy control subjects. Differences in diffusion anisotropy did not reach statistical significance. The decrease in anisotropy is probably due to several factors, such as loss of myelin from white matter fiber tracts, expansion of the extracellular space fraction, and perilesional inflammatory edema. Reduced anisotropy is also seen in MS brain lesions . A large standard deviation in the lesion values was observed by Clark and colleagues, which could be explained by lesion heterogeneity. On postmortem high-resolution MR imaging of the spinal cord in MS, two main types of lesions have been found: lesions with marked signal intensity (SI) changes that corresponded with complete demyelination and lesions with mild SI abnormalities where only partial demyelination was found histologically .
To assess whether diffusion tensor-derived measures of cord tissue damage are related to clinical disability, mean diffusivity (MD) and fractional anisotropy (FA) histograms were acquired from the cervical cords obtained from a large cohort of patients who had MS . In that study, diffusion-weighted, echo planar images of the spinal cord and brain DW images were acquired from 44 patients who had MS and from 17 healthy control subjects. The study showed that average cervical cord FA was significantly lower in patients who had MS compared with control subjects. Good correlation was found between the average FA and average MD and the degree of disability. In another recently published study, axial diffusion tensor MR imaging (DTI) was performed in 24 patients who had relapsing-remitting MS and 24 age- and sex-matched control subjects . FA and MD were calculated in the anterior, lateral, and posterior spinal cord bilaterally and in the central spinal cord at the C2-C3 level. Significantly lower FA values were found in the lateral, dorsal, and central parts of the normal-appearing white matter in patients who had MS. The results of this study show that significant changes in DTI metrics are present in the cervical spinal cord of patients who have MS in the absence of spinal cord signal abnormality at conventional MR examination . The exact value of DW imaginging and DTI in MS of the spinal cord has not been completely evaluated .
Studies have been performed to evaluate the usefulness of T1 relaxation time and magnetization transfer ratio . In one study of 90 patients who had MS and 20 control subjects, reduced histogram magnetization transfer ratio values were found in patients who had MS . Although the results were encouraging, the long acquisition times are clinically questionable.
Devic’s neuromyelitis optica
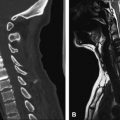
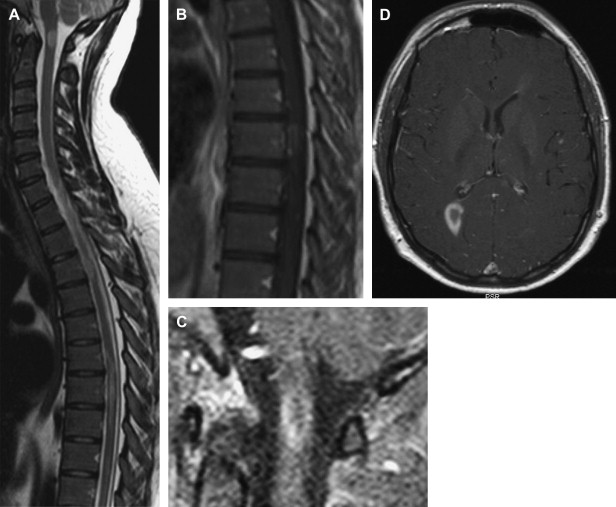
Devic’s neuromyelitis optica (DNMO) is a demyelinating disease characterized by bilateral visual disturbance and transverse myelopathy. It was first described in 1894 by Eugene Devic in a woman who suffered from a bilateral optic neuritis and acute transverse myelitis. Pathologically, lesions are restricted to the optic nerves and spinal cord, with areas of necrosis of gray and white matter, cavitations, lack of inflammatory infiltrate, vascular hyalinization, and fibrosis . Clinically, the disease may have a mono- or multiphasic course . The nosology is not clear, and the reports from the literature are confusing. Historically, the disease was defined as a monophasic disorder consisting of fulminant bilateral optic neuritis and myelitis, occurring in close temporal association. Cases of DNMO that followed in the literature described more extensive findings, with a relapsing course, which raised the question of whether DNMO represents a separate syndrome or a variant of MS. One of the largest series published by a group from the Mayo Clinic included 71 patients who had DNMO . Based on their findings, the initial definition was revised. Clinical characteristics, course, and prognosis have been evaluated further on 46 patients from 15 Italian MS centers . Compared with patients who had MS, patients who had DNMO had a poor prognosis, higher age at onset, and a more sever clinical course. DNMO was most like to affect female patients. Corticosteroids are not helpful in DNMO, and the prognosis is poor. Cerebral spinal fluid (CSF) abnormalities include pleocytosis, high protein, and high albumin ratio levels . The most common abnormality observed on MR images of the spinal cord is longitudinal, confluent lesions extending across five or more vertebral segments, with a hyperintensity on T2-weighted images ( Fig. 7 ) . Cord swelling and enhancement were present in 24 of 100 MR scans evaluated in one study . In one study with nine patients diagnosed with possible DNMO in French hospitals, the authors observed that cord atrophy was associated with complete para- or quadriplegia, whereas cord swelling was associated with possible neurologic improvement . Short inversion time inversion recovery techniques depict the lesions of the optic nerves in cases of presumed neuromyelitis optica . MR imaging findings can be used to differentiate between DNMO and MS: In DNMO, no cerebral white matter lesions are present; spinal cord lesions are confluent and extend to multiple segments in DNMO, which is uncommon in MS; spinal cord atrophy is present in MS but is often described as part of the course of DNMO; and cranial nerves or cerebellar involvement are common in MS but are not present in DNMO . The discovery of a novel serum autoantibody, NMO-IgG, with high sensitivity and specificity for DNMO, has significantly improved the early diagnosis of this severe demyelinating syndrome . Clinical findings that favor DNMO are higher age at onset and severe course . Results from the recently published study challenge the classic belief of a sparing of the brain tissue in DNMO; compared with healthy control subjects, patients who had DNMO showed a reduced magnetization transfer ratio and increased mean diffusivity of the normal-appearing gray matter of the brain .
Transverse myelitis
The first cases of acute transverse myelitis (ATM) were described in 1882 by Bastian . In 1922 and 1923, 200 cases of so-called “post-vaccination encephalomyelitis” were reported in Holland and England. It was in 1948 that the term ATM was used in reporting a case of severe myelopathy after pneumonia .
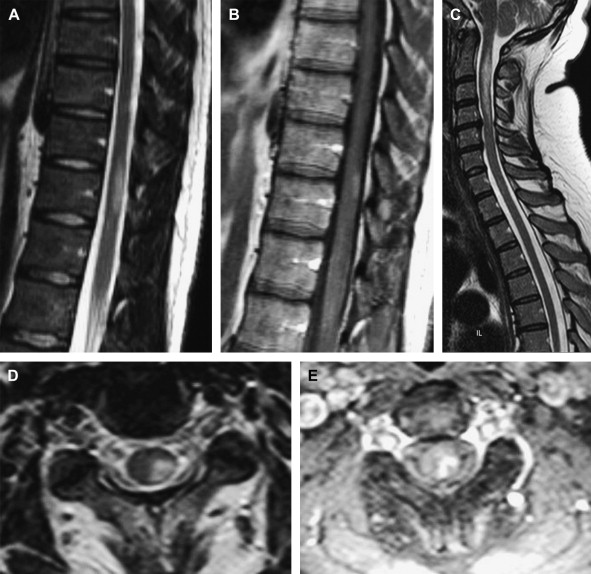
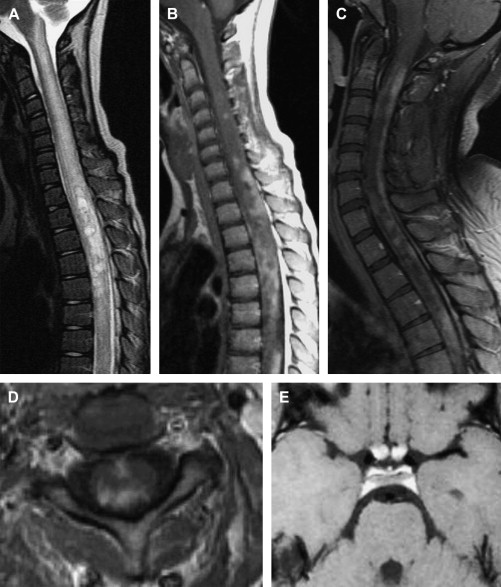
Transverse myelitis is a clinical syndrome characterized by bilateral motor, sensory, and autonomic disturbances . About 50% of patients have paraparesis; 80% to 94% have numbness, paresthesias, and band-like dysesthesias; and all have bladder dysfunction . The histopathologic features of TM include perivascular monocytic and lymphocytic infiltration, demyelination, and axonal injury . TM may exist as part of a multifocal CNS disease; as a multi-systemic disease; or as an isolated, idiopathic entity. The immunopathogenesis of disease-associated TM is varied and includes vasculitis neurosarcoidosis, MS, and lupus. Several reports of TM after vaccination have been published . Recently, the term “parainfectious TM” has been introduced for TM cases with antecedent respiratory, gastrointestinal, or systemic illness . A variety of immune stimuli (eg, molecular mimicry, superantigen-mediated immune activation) may trigger the immune system to injure the nervous system . In a retrospective study of 288 patients who had TM, 45 (15.6%) met the criteria for idiopathic TM . According to the published series, approximately one third of patients recover with little or no sequelae, one third are left with a moderate degree of permanent disability, and one third develop severe disability . In 2002, the Transverse Myelitis Consortium Working Group proposed criteria for idiopathic ATM, with incorporation of CSF testing and MR imaging findings . The criteria include (1) bilateral sensory, motor, or autonomic spinal cord dysfunction; (2) defined sensory level and bilateral signs and symptoms; (3) proof of inflammation within the spinal cord by MR imaging or CSF examination; (4) symptoms from onset to reach maximal deficit between few hours and 21 days; and (5) exclusion of extra-axial compressive etiology . The thoracic spine is most commonly involved, and middle-aged adults are usually affected. MR imaging findings include focal, centrally located increased signal on T2-weighted MR images, usually occupying more than two thirds of the cross-sectional area of the cord ( Fig. 8 ) . This was observed in 88% of patients in a series of 17 patients who had idiopathic TM . Usually, the signal abnormality extends more than three to four vertebral segments in length. Cord expansion may or may not be present; it was found in 47% in published series . Enhancement is usually absent; when enhancement was present, two patterns have been described: moderate patchy enhancement or diffuse abnormal enhancement ( Figs. 9 and 10 ) . Enhancement was found in only 38% of cases of idiopathic TM in one series and in 47% and 53% in the two other series . About 40% of TM cases display a normal MR imaging study . MS is the most important differential diagnosis of TM. Signal abnormality located peripherally in the spinal cord that is less than two vertebral segments in length and occupying less than half the cross-sectional area of the cord favors a diagnosis of MS rather than TM .

There is growing evidence that the length of the lesion is likely important from a pathogenic and a prognostic standpoint. Patients who have acute partial transverse myelitis have signal abnormalities extending less than two segments on MR imaging, and patients who have complete longitudinally extensive transverse myelitis have abnormalities that extend to multiple segments (see Fig. 8 ). Patients in the first group are at higher risk for developing MS compared with those in the second group, where the risk is low .
DTI was recently used to characterize inflammatory processes of the spinal cord . In cases of inflammatory myelitis, decreased FA values have been found in the region of a T2-weighted lesion and increased FA values in the lesion’s boundaries. This pattern is different from that seen in invasive tumors, in which FA is low in peripheral regions of edema.
Novel biomarkers, such as cytokine interleukin-6 and collapsin response-mediator protein–5 are potentially useful prognostic indicators and markers of disease severity. The “idiopathic” form of ATM is rarely seen .
Acute disseminated encephalomyelitis
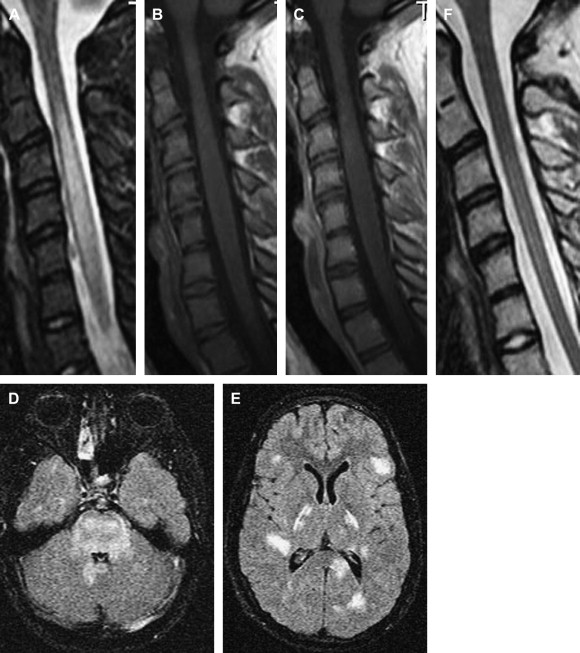
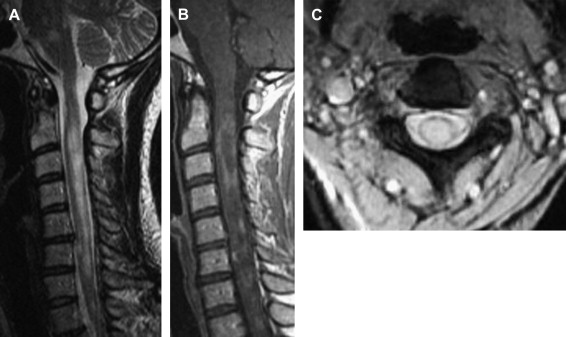
Acute disseminated encephalomyelitis (ADEM) is an acute demyelinating disorder of the CNS, usually occurring after infections and vaccinations. The most probable pathophysiology is an autoimmune response to myelin basic protein, triggered by infection or immunization. Although ADEM is usually considered a monophasic disease with a good prognosis, recurrent or multiphasic forms have been described . ADEM seems to occur more frequently in children and young adults. The most frequent clinical symptoms include motor deficits, sensory deficits, brain stem signs, and ataxia . CSF findings are nonspecific, with oligoclonal bands detected in up to 65% of patients . On MR imaging, ill-defined hyperintense lesions on T2-WI and hypointense lesions on T1-WI in the spinal cord can be recognized ( Figs. 11 and 12 ) . Lesions are usually large and extend over a long segment of the spinal cord with cord expansion (see Figs. 11 and 12 ). The thoracic cord is most commonly affected. Spinal cord involvement was reported in 71% of patients in one series . All patients who had spinal involvement had cerebral lesions and signs of myelopathy . The MR imaging appearance of ADEM is nonspecific and indistinguishable from other inflammatory lesions, particularly MS plaques. Many patients initially diagnosed with ADEM develop clinically definite MS upon long-term follow-up. In one clinical study, 35% of all adult patients initially diagnosed with ADEM developed MS over a mean observation period of 38 months . Similar results have been reported in children, with 17 of 121 children initially diagnosed with ADEM later developing MS .