FIGURE 9.3 On the medial side of the elbow, the medial epicondyle of the distal humerus is the most prominent bony landmark. It is the origin of the ulnar collateral ligament complex as well as the flexor–pronator muscle mass.
Posteriorly, palpation should begin with the olecranon bursa, which overlies the triceps insertion into the olecranon. Any pain with palpation, thickening of the bursa, or the presence of an olecranon osteophyte (within the substance of the triceps) should be noted. The distal triceps should also be palpated for tenderness or for a frank defect, which may be present in the case of a triceps tear or avulsion. The tip of the olecranon and the olecranon fossa are more easily palpable with the arm flexed past 60 degrees. The posteromedial aspect of the olecranon is a frequent location of osteophyte formation in throwing athletes, resulting in elbow impingement symptoms and pain on full extension. Pain with palpation in this area may indicate osteophyte formation or the presence of loose bodies.
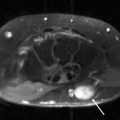
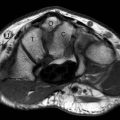
Working laterally, the radial head is palpated posteriorly. It is easily palpated and located by repetitively pronating and supinating the elbow while axially loading the elbow. Any pain or crepitation should be noted with this maneuver as well as subluxation of the radial head, which may be indicative of elbow instability. An elbow joint effusion may also be palpated in the area posteriorly between the olecranon tip, radial head, and lateral epicondyle (Fig. 9.4). The lateral epicondyle is located 2 cm proximal to the radial head and is less prominent than the medial epicondyle. The wrist extensors (or “mobile wad of Henry”) originate on the lateral epicondyle, and tenderness on palpation in this area may suggest lateral epicondylitis. Pain with palpation of the medial aspect of the extensor bundle distal to the radial head may be indicative of radial nerve entrapment, as in radial tunnel syndrome. The lateral ulnar collateral ligament complex is less defined than the ulnar collateral ligament complex.
Range of Motion
The evaluation of both active and passive range of motion is important in the complete physical examination of the elbow. Active range of motion is tested first and identifies the functional limitations of motion. Active elbow flexion–extension and pronation–supination as well as wrist dorsiflexion and palmar flexion should be assessed. Measurements of passive range of motion are performed when limitations in active motion are noted. Limitations of active and passive elbow motion may be the result of true mechanical or static restrictions such as soft tissue contracture, degenerative joint disease, or loose bodies. Limitations in active and passive motion may also be the result of patient guarding secondary to pain. Conversely, isolated limitations in active motion (with normal passive motion) may be the result of dynamic loss as is seen in patients with neurologic deficits or tendon ruptures. Again, both elbows should be examined to determine subtle differences in motion.
FIGURE 9.4 An elbow effusion may also be palpated in the area posteriorly among the olecranon tip, radial head, and lateral epicondyle. This area is sometimes known as the soft spot.
Normal elbow range of motion in the sagittal plane (extension–flexion) is typically 0 to 140 degrees 10 degrees, whereas forearm rotation values are normally between 80 and 90 degrees of pronation and supination (19–21). Range of motion in the sagittal plane should be tested with the forearm in neutral rotation and with the arm adducted at the side, because the patient may attempt to compensate for loss of motion by changing their shoulder position. Forearm rotation should be measured with the arm adducted and with the elbow flexed to 90 degrees.
When measuring elbow range of motion, the examiner should evaluate the patient’s reports of pain during motion and at the end points and also assess for crepitation during motion. The “feel” of the end point of full extension and full flexion is also important in the evaluation. In the normal elbow, the end point in terminal extension is hard (as a result of bony contact between the olecranon tip and the olecranon fossa) and soft in full flexion (as a result of muscle impingement). In the case of motion loss, a solid end point may indicate the presence of loose bodies or spurs that are blocking motion, whereas a soft end point may be caused by capsule contractures, joint effusion, tendon contracture, or ligament injury.
Strength Testing
Strength testing of the elbow should include motor examination of the entire extremity. This is particularly true for throwing athletes, because weakness of the rotator cuff or scapular stabilizers may lead to poor throwing mechanics and subsequent elbow injury. Therefore, a thorough motor examination of the rotator cuff, deltoid, and scapular stabilizers should be performed. Again, testing should be performed on both the injured and noninjured extremity.
In elbow strength testing, the brachialis is tested by resisting patient elbow flexion with the forearm in pronation. The strength of the brachioradialis may be tested by resisting patient elbow flexion with the forearm in neutral rotation. The biceps brachii is tested with the arm in 45 degrees of flexion with the forearm in full supination with the examiner resisting elbow flexion (22). Alternatively, the examiner may resist active patient supination with the elbow flexed to 90 degrees to test biceps brachii strength. Triceps strength may be evaluated by resisting active extension of the elbow with the forearm in neutral rotation. Resisted pronation, wrist extension, and wrist flexion should be evaluated with the arm adducted and the elbow flexed to 90 degrees and repeated with the elbow in extension. The evaluation of grip strength, thumb abduction strength, and intrinsic hand muscle strength should also be performed, because they may provide evidence of nerve entrapment syndromes of the median, posterior interosseous, and ulnar nerves, respectively (22).
Neurologic and Vascular Examination
In patients with subtle reports of elbow pain or weakness, a thorough neurologic examination must be performed. This includes an examination of sensory, motor, and reflex functions of the upper extremity because cervical spine conditions may cause referred elbow pain.
Sensation should be checked in the axillary nerve region (lateral deltoid patch), the musculocutaneous nerve (which distally becomes the lateral antebrachial cutaneous nerve, providing sensory innervation to the lateral volar aspect of the forearm), the superficial radial nerve (dorsal radial surface of the hand), the median nerve (volar surfaces of the thumb, second and third digits), and ulnar nerve (volar surfaces of the fourth and fifth digits).
Finally, a vascular examination should be performed to evaluate the patient for evidence of arterial compression or the brachial, radial, and ulnar arteries. The brachial artery and median nerve may be compressed as they pass under the ligament of Struthers, which is present in approximately 1% of the population. The ligament, when present, passes from the medial epicondyle to the supracondylar process of the humerus.
It is important to recognize that elbow symptoms may be present in thoracic outlet syndrome (TOS) or axillary venous occlusion. The modified Wright test, which is used to determine TOS, is performed by palpating the patient’s radial pulse. The patient’s arm is then placed in abduction and external rotation while the pulse is monitored. Patients are then instructed to rotate their head to the involved shoulder. A diminished pulse confirms TOS. In overhead athletes, axillary venous occlusion may occur as a result of repetitive impingement with the action of throwing (arm abduction) and is manifested by pain and venous engorgement of the upper extremity and a generalized “dead arm” feeling during throwing periods.
Specific Examinations for Elbow Pathology
There are many afflictions of the elbow that may be adequately evaluated using a thorough general physical examination complemented by the appropriate radiographic studies. These injuries include most fractures, acute dislocations, and arthritis. The clinical evaluation of soft tissue injuries of the elbow, which are some of the more common causes of elbow pain and dysfunction, may be much more difficult. These injuries include tendinitis and tendinopathies, tendon ruptures, ligamentous injuries, and nerve entrapment disorders. In the evaluation of these entities, many special signs and tests have been described to aid in the evaluation of these processes. MRI is also an important adjunct because of its ability to accurately evaluate soft tissue structures of the elbow. The following is a discussion of the evaluation of those entities in which MRI is most effectively used to improve diagnostic accuracy.
Examination of Elbow Tendinopathies
Lateral Epicondylitis
Lateral epicondylitis, or “tennis elbow,” was originally described by Major in 1883 (23, 24). Although 95% of cases are a result of causes other than tennis, it is estimated that 10% to 50% of people who regularly play tennis may have symptoms of lateral epicondylitis at some point (25–27). The onset of symptoms may be acute or gradual, and a history of repetitive flexion–extension or pronation–supination motions may be related. Among athletes playing racquet sports, the backhand is the most common swing to produce symptoms (26). Because the incidence of lateral epicondylitis is much less at the professional level, it is thought that poor swing mechanics initiate the process (27). Patients may describe a constant burning pain of the lateral aspect of the elbow that is aggravated by the actions of shaking hands, grasping objects, carrying luggage, and pouring from a pitcher.
On physical examination, patients have point tenderness over the origin of the extensor carpi radialis brevis or the entire extensor wad insertion on the lateral epicondyle. The pain increases with resisted wrist extension with the elbow extended and the forearm fully pronated. Resisted forearm supination may also aggravate the patient’s symptoms. In a modified test, the wrist may be passively volar-flexed while the elbow is in extension, further stressing the wrist extensors. The “chair test,” in which the patient is asked to lift a chair with the forearm pronated, may also elicit pain over the lateral epicondyle (28). It is important for the examiner to differentiate between the more proximal palpable tendon tenderness of lateral epicondylitis and deep pain in the midforearm extensor area, which may be elicited with resisted supination, findings more suggestive of posterior interosseous nerve entrapment.
Medial Epicondylitis
Medial epicondylitis, or medial tendinosis of the wrist flexor–pronator group, occurs far less frequently than lateral epicondylitis. Lateral epicondylitis is up to seven times more common, most likely because most grasping activities place the wrist in relative extension (29–31). Medial epicondylitis has been associated with a variety of sports and activities, including squash, racquetball, tennis, golf, and bowling. In racquet sports, the serve and forehand strokes are symptom aggravators. Medial epicondylitis (often referred to as “golfer’s elbow”) develops as a result of repetitive wrist flexion and pronation or repetitive valgus overload of the elbow as seen in throwing athletes. More rarely, an acute, violent injury may result in injury to the myotendinous junction. Symptoms of aching pain in the flexor musculature at the medial epicondyle are most common. Patients may also report weakness in their grip. Palpation of the elbow will elicit tenderness over the anterior aspect of the medial epicondyle. Patients will report forearm flexor muscle pain or pain over the medial epicondyle with resisted pronation and resisted wrist flexion performed with the elbow in extension. Pain may also be elicited by extending (dorsiflexing) the wrist with the elbow extended, putting passive tension force on the flexor muscles.
It is not uncommon for patients to report symptoms of mild ulnar nerve irritation. Nirschl (32) found ulnar nerve dysfunction in 60% of patients scheduled for surgical treatment of medial epicondylitis. Symptoms are usually mild and are sensory in nature and are presumed to be the result of local inflammation causing a compressive neuropathy of the ulnar nerve. Gently tapping on the nerve within the cubital tunnel may elicit a sensation of paresthesias distally, a positive Tinel sign, suggestive of ulnar nerve irritation.
It is important to differentiate medial epicondylitis from ulnar collateral ligament complex (UCL) insufficiency, especially in the overhead-throwing athlete. A thorough history will often help in differentiating between the two injuries, although they may occur together. While medial epicondylitis tends to have an insidious onset of symptoms, UCL injury may sometimes occur during an acute event that the patient will likely recall. Further instability testing, which is discussed later in this Chapter, will secure the diagnosis of UCL injury.
It is also important to differentiate medial epicondylitis from a medial epicondyle avulsion fracture or medial epicondylar apophysitis in the adolescent athlete. Medial epicondyle avulsion fractures result from a medial traction injury attributable to acute valgus stress and a violent flexor–pronator muscle contraction, usually during the act of throwing. The athlete reports an acute medial elbow pain after a pitch or throw and is unable to continue playing. The injury usually occurs in the late cocking or early acceleration phase of throwing, and a loud pop may be heard at the time of injury. Bruising and point tenderness will be noted over the medial epicondyle, and the athlete will resist elbow extension past 15 degrees and valgus stress testing as a result of discomfort. In contrast, medial epicondylar apophysitis presents as a more chronic problem with the insidious onset of medial elbow pain that occurs with throwing in athletes generally between the ages of 9 and 12 years. The injury is caused by traction of the flexor–pronator mass and the ulnar collateral ligament on the medial epicondylar apophysis mediated by the repetitive valgus stresses of throwing (33). Athletes may report medial epicondyle pain and a reduction in throwing velocity and effectiveness (34).
Triceps Tendinitis and Triceps Rupture
Triceps tendon injuries are relatively rare, with ruptures occurring even more rarely, with a predilection in men in their 30s. Triceps tendinitis occurs in weightlifters, baseball players, and carpenters as a result of repetitive elbow extension activities. It is often associated with loose bodies in the posterior compartment and lateral epicondylitis (35, 36). In the adolescent throwing athlete, repetitive forceful triceps contraction during the early acceleration phase of throwing may cause microtrauma to the olecranon apophysis, causing posterior pain, swelling, and a decrease in throwing effectiveness (33).
Partial or complete triceps tendon ruptures usually occur as a result of a fall on the outstretched hand or as a result of laceration or a direct blow (37). The tendon ruptures because a deceleration force is superimposed on the contracted triceps muscle, resulting in an eccentric musculotendinous overload. In the older adolescent throwing athlete, avulsion of the olecranon apophysis may occur with the dramatic onset of pain during the acceleration or followthrough phase of throwing (33). Triceps rupture may also occur spontaneously with minimal trauma in patients at risk as a result of hyperparathyroidism, renal osteodystrophy, chronic steroid use, or previous steroid injections into the triceps (38, 39). Ruptures most commonly occur at the triceps insertion into the olecranon, although musculotendinous junction tears may occur (40). On presentation, the patient may report pain in the posterior aspect of the elbow, and posterior bruising and swelling may be noted. When the rupture is complete, the patient may be unable to actively extend the elbow against gravity, and a palpable defect may be noted. In the case of a partial tear, there may be a partial loss or weakness of active extension, and sometimes a small or incomplete defect may be palpated (41). Viegas (42) described a test for differentiating complete and partial triceps tears, which is based on the Thompson test used for evaluation of Achilles tendon ruptures. In the test, the elbow is flexed to 90 degrees and the triceps muscle belly is compressed by the examiner’s hand. A complete lack of passive extension with this maneuver is indicative of a complete triceps tendon rupture.
Distal Biceps Rupture
Distal biceps ruptures are far less common than proximal biceps ruptures and usually occur in the dominant arm of men between the ages of 40 and 60 years. The mechanism of biceps rupture is generally an acute traumatic event in which the distal biceps tendon is eccentrically loaded with a sudden extension force, usually while the arm flexed to 90 degrees (43). This may occur during weightlifting or during a traumatic event. The biceps tendon is usually avulsed from the bicipital tuberosity of the radius, resulting in an abrupt and painful ripping sensation in the antecubital fossa. Patients may relate hearing a “pop” or feeling the retraction of the tendon proximally at the moment of injury.
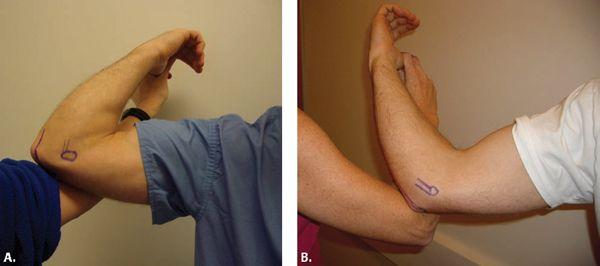
Acutely, bruising and swelling is noted in the antecubital fossa, often with proximal extension. Patients may report flexion and supination weakness in the acute phase with a dull ache in the elbow region. As the injury becomes less acute, flexion strength may partially recover and patients primarily report loss of supination and grip strength (44, 45). With active elbow flexion, a defect in the antecubital fossa may be palpated where the biceps normally resides and the biceps muscle retracts proximally (Fig. 9.5). If the tendon can be palpated, a partial biceps tear or musculotendinous injury may have occurred. On examination, most patients with biceps ruptures will have full passive range of motion but will demonstrate supination weakness and possibly flexion weakness. Flexion strength is tested with the arm in 45 degrees of flexion with the forearm in full supination with the examiner resisting elbow flexion. Supination strength is tested with the elbow flexed to 90 degrees with the examiner resisting active patient supination (22).
Examination for Instability
Medial (Valgus) Elbow Instability
The UCL is the primary structure providing valgus stability of the elbow. Aside from being torn during an acute elbow dislocation, injury to the UCL has been reported to occur with increasing frequency in overhead-throwing athletes. The mechanism of injury is attributed to the substantial forces placed across the elbow during throwing. The valgus forces generated during the cocking and acceleration phases of throwing exceed the intrinsic tensile strength of the UCL, resulting in microtears in the ligament. Additional cumulative stresses to the UCL resulting from improper throwing mechanics, poor flexibility, and inadequate conditioning may result in further attenuation and rupture of the UCL (46, 47).
FIGURE 9.5 Acute distal biceps rupture. With active elbow flexion, a defect in the antecubital fossa may be palpated where the biceps normally resides, and the biceps muscle retracts proximally.
FIGURE 9.6 Physical examination of the elbow for valgus instability may be performed with the patient supine with the patient’s arm abducted and externally rotated to minimize rotation of the upper arm during testing, allowing isolation of the ulnar collateral ligament.
Athletes with acute UCL injury usually experience the sudden onset of pain after throwing, with or without an associated popping sensation, and are unable to continue throwing. Patients with chronic injury usually describe a gradual onset of localized medial elbow pain during the late cocking or acceleration phase of throwing. Athletes may also describe pain after a lengthy or heavy throwing session, which results in a subsequent loss of throwing velocity. However, it is not uncommon for those with chronic UCL insufficiency to present with an acute episode. Most cases of symptomatic UCL injury requiring reconstruction are acute exacerbations of chronic insufficiency. Patients with chronic instability may report ulnar nerve symptoms caused by secondary irritation of the ulnar nerve within the cubital tunnel as a result of local inflammation of the ligamentous complex. They may also frequently develop medial epicondylitis resulting from increased stretching of the musculotendinous complex or as a result of compensatory overload of this muscle group as it attempts to compensate for the UCL laxity (47).
Physical examination of the elbow for valgus instability has been described many ways. The classic description and common technique to assess UCL function is to test the elbow with the patient seated and the wrist secured between the examiner’s forearm and trunk, usually with the patient’s forearm maximally pronated. Alternatively, the patient may be examined while lying supine with patient’s arm abducted and externally rotated. This position minimizes rotation of the upper arm during testing, allowing isolation of the UCL (Fig. 9.6) (22). In either test, the patient’s elbow is flexed to approximately 25 degrees as a valgus stress is applied. This maneuver stresses the anterior band of the anterior bundle (anterior oblique ligament) of the UCL. It is important to palpate the UCL along its course from the medial epicondyle toward the proximal ulna as valgus stress testing is performed. Valgus laxity is manifested by increased medial joint space opening as compared with the contralateral elbow. Comparison with the uninvolved elbow should always be performed to differentiate between physiological and pathologic laxity. In the normal elbow, the valgus stress test should not elicit any pain. Loss of a firm end point, pain, and/or increased medial joint space opening with valgus stress is consistent with an attenuated or incompetent UCL (5).
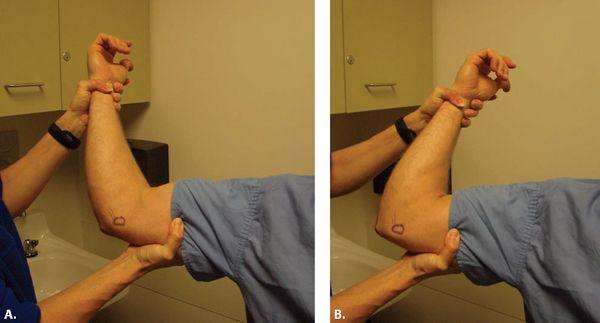
More recently, O’Driscoll has described a new test for UCL insufficiency, referred to as the “Mayo moving valgus stress test” or the “painful arc test” (48). During the test, the patient’s shoulder is placed in an abducted and externally rotated position. The examiner applies a valgus force to the elbow while the elbow is taken through its full range of motion. Patients with UCL insufficiency typically report pain when the elbow is flexed between 80 and 120 degrees of flexion (the “painful arc”) (Fig. 9.7A–B).
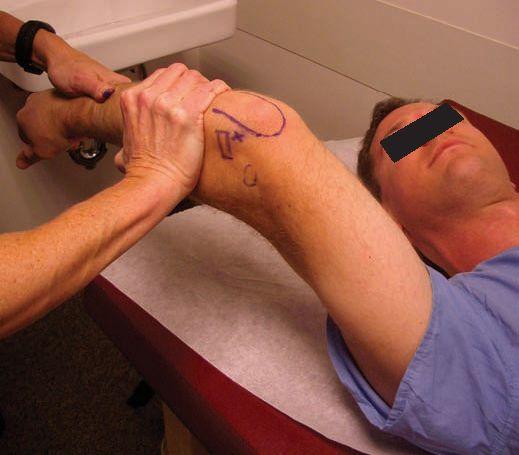
The posterior band of the anterior bundle (anterior oblique ligament) of the UCL is functionally important in the overhead-throwing athlete. The posterior band contributes to valgus stability at elbow flexion angles greater than 55 degrees, and it is the primary restraint to valgus stress with higher degrees of elbow flexion (4, 49). Testing of this posterior band may be accomplished using the “milking maneuver,” which is performed by pulling on the patient’s thumb with the patient’s forearm supinated, shoulder extended, and the elbow flexed past 90 degrees (Fig. 9.8A) (47). This maneuver generates valgus stress on the flexed elbow. A subjective feeling of apprehension and instability, in addition to localized medial-side elbow pain, is indicative of UCL injury.
The standard description for performing the “milking maneuver” requires the elbow to be flexed past 90 degrees and often near 120 to 140 degrees. As a result, this test is better for detecting injury or insufficiency of the posterior oblique ligament or the posterior band of the anterior oblique ligament. However, valgus laxity is often difficult to assess as a result of the increased contribution of the bony articulations to the stability of the elbow in these higher degrees of flexion. For this reason, a modification of the test has been described recently. With the patient’s arm in some abduction and external rotation, the elbow is flexed to only 70 degrees. This degree of flexion is used because biomechanical studies have shown that valgus laxity of the elbow is greatest between 70 and 90 degrees of elbow flexion in UCL insufficiency (4, 50, 51). The examiner then pulls on the patient’s thumb applying valgus force to the elbow while palpating the medial joint line with the examiner’s other hand, assessing for medial joint gapping and quality of the end point (Fig. 9.8B). Both elbows are examined and compared.
A loss of terminal extension secondary to flexion contractures (which develop as a result of the repeated attempts at UCL healing and stabilization) may also be present in cases of chronic valgus instability (52). However, flexion contractures and increased carrying angle (valgus alignment of the elbow) are common in high-level baseball players who lack valgus laxity.
FIGURE 9.7 O’Driscoll’s “moving valgus stress” test for ulnar collateral ligament (UCL) injury. During the test, the patient’s shoulder is placed in an abducted and externally rotated position. The examiner applies valgus force to the elbow while the elbow is taken through its full range of motion. Pain will be present in patients with an UCL insufficiency within a “painful arc” between 80 (A) and 120 (B) degrees of flexion.
FIGURE 9.8 A: Testing of the posterior band of the anterior bundle of the ulnar collateral ligament may be accomplished by the “milking maneuver,” which is performed by pulling on the patient’s thumb with the patient’s forearm supinated, shoulder extended, and elbow flexed past 90 degrees. B: The modified “milking maneuver” test positions the patient’s elbow at 70 degrees of flexion because biomechanical studies on cadavers suggest that this is the best position to evaluate for ulnar collateral ligament insufficiency.
Lateral and Posterolateral Elbow Instability
The lateral ulnar collateral ligament complex, comprised of the radial collateral ligament, the annular ligament, and the lateral ulnar collateral ligament, provides varus stability to the elbow. Varus instability resulting from injury of the radial collateral ligament of the lateral ulnar collateral ligament complex is a very infrequent acute isolated instability pattern, because pure varus stress to the elbow is not commonly generated from routine activities (53). A history of acute varus stress to the elbow associated with point tenderness and varus instability on physical examination is diagnostic. Physical examination of the elbow for varus instability is best performed with the elbow flexed between 15 and 30 degrees with the patient’s upper arm maximally internally rotated. Loss of a firm end point, pain, or increased lateral joint space opening with varus stress is consistent with an attenuated or incompetent radial collateral ligament (22).
In posterolateral rotatory instability, deficiency of the lateral ulnar collateral ligament (LCL) is the essential pathologic lesion (54, 55). LCL injury most commonly occurs as a result of acute dislocation or as a complication of tennis elbow release, although it has also been reported as a result of chronic cubitus varus (gunstock deformity) seen with malunions of supracondylar humerus fractures (53).
Patients give a history of a prior elbow dislocation and report symptoms resulting from subluxation of the radial head posterolaterally with rotatory subluxation of the humeroulnar joint. They may report having the sensation of a pop, catch, or “clunk” as the elbow goes from full extension to flexion, or they may state they feel like their elbow dislocates. They frequently have symptoms when driving, pushing up with their hands when getting out of a chair, and/or with pushups. In some cases, patients may only report pain over the lateral aspect of the elbow, because the laxity is often very subtle.
With standard varus stress testing, the patient may report pain in the posterolateral aspect of the elbow, and the lateral joint line will not gap open unless gross instability is present. The posterolateral rotatory–instability test, or “pivot shift” test, described by O’Driscoll et al. (55) aids in the diagnosis. The test is performed with the patient supine with the arm in forward flexion (Fig. 9.9). The forearm is fully supinated and both an axial load and valgus stress are applied to the elbow. With the elbow in the extended position, a dimple is demonstrated laterally (Fig. 9.10A), and the radial head becomes prominent. The elbow maximally subluxates at 40 degrees, and further flexion may cause a palpable and visible clunk as the elbow reduces (Fig. 9.10B). With greater degrees of laxity, greater flexion may be needed to demonstrate the reduction of the radial head. In some instances, the patient simply notices pain with this maneuver without a demonstrable pivot being noted, because patient guarding may make this test difficult to perform. Other functional tests have been described to elicit symptoms. Patients may report pain or giving way while doing pushups with the forearm in supination and pronation or when trying to lift their body out of a chair with their hands.
Valgus Extension Overload
Valgus extension overload is a condition that also causes medial elbow pain and is commonly seen in overhead-throwing athletes, gymnasts, and shot putters. Repetitive valgus stress across the elbow causes impingement of the posteromedial olecranon tip against the medial wall of the olecranon fossa. Over time, osteophyte formation may occur on the olecranon at the site of impingement or within the olecranon fossa. Additionally, hypertrophy of the soft tissues and the synovium may occur, leading to increased pain and swelling. Throwers report pain in the posteromedial aspect of the elbow at the start of the acceleration phase of throwing (56). Symptoms may be similar to those seen with injury to the UCL complex, except for the location of pain. Patients with valgus extension overload have the most pain with palpation of the posterior medial tip of the olecranon. Posteromedial pain during the valgus extension overload test is diagnostic. During this test, the elbow is repeatedly forced into extension by the examiner while a valgus stress is also applied in an effort to mimic the acceleration phase of throwing (Fig. 9.11) (56).
FIGURE 9.9 The posterolateral rotatory–instability test, or pivot shift test. The test is performed with the patient supine with the arm in forward flexion. The forearm is fully supinated and both an axial load and valgus stress are applied to the elbow. In a patient undergoing the posterolateral rotatory–instability test with the elbow in the extended position, a dimple is demonstrated laterally, and the radial head becomes prominent. The elbow maximally subluxates at 40 degrees, and further flexion may cause a palpable and visible clunk as the elbow reduces.
Nerve Entrapment Syndromes
The unusual anatomy of the elbow makes it vulnerable to a variety of nerve entrapment syndromes. Symptoms are the result of nerve compression by a variety of structures, including muscle, fascia, or ligaments, and may be as varied as vague pain, numbness, or frank weakness.
Median Nerve Entrapment Syndromes
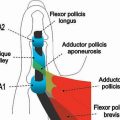
Median nerve entrapment may occur at the elbow at various locations. Above the elbow, the ligament of Struthers is a potential compression site. It originates from the humerus at the site where a supracondylar process may occur and attaches to the medial epicondyle. Entering the forearm, the nerve is subject to potential compression by the lacertus fibrosus. The median nerve then passes beneath the humeral head of the pronator teres, a potential site of compression. The nerve then courses beneath the proximal fibrous arch of the two muscular heads of the flexor digitorum superficialis, where compression is also possible. The median nerve continues distally in the forearm between the flexor digitorum superficialis and the flexor digitorum profundus. The anterior interosseous nerve, which is the last major branch of the median nerve in the proximal forearm, supplies the flexor pollicis longus, the flexor digitorum profundus to the index and long fingers, and the pronator quadratus. Anomalous arteries such as an aberrant radial artery or an enlarged bicipital bursa may also cause pressure on the nerve (57).
Pronator syndrome results from the compression of the median nerve at one of four potential compression sites: beneath the ligament of Struthers, beneath the lacertus fibrosis, between the two heads of the pronator teres muscle, or at the arch of the flexor digitorum superficialis muscle. Pronator syndrome commonly occurs with strenuous activities such as weightlifting and in occupations requiring repetitive pronation of the forearm with the elbow extended, but may be caused by other activities such as competitive automobile racing or fast-pitch softball pitching. Patients usually report pain in the proximal volar surface of the forearm, which increases with activity. Pronator syndrome can be confused with carpal tunnel syndrome, because both may cause numbness and paresthesias in the median nerve-innervated digits and pain or cramping symptoms in the wrist and forearm. One discriminator between the two compression syndromes is that in pronator syndrome, the patient reports dysesthesias in the skin overlying the thenar eminence. These same symptoms should not be present in carpal tunnel syndrome, because this area is innervated by the palmar cutaneous branch of the median nerve, which originates proximal to the transverse carpal ligament (the location of nerve compression in carpal tunnel syndrome) (57). Thumb interphalangeal weakness is indicative of median nerve entrapment proximal to the wrist, because the flexor pollicis longus is innervated by the anterior interosseous nerve.
FIGURE 9.10 A: Clinical picture of patient with posterolateral rotatory–instability demonstrated during the pivot shift test. With the elbow in the extended position, a dimple is demonstrated laterally, and the radial head becomes prominent. B: Further flexion during the pivot shift test in a patient with posterolateral rotatory instability reduces the radial head.
FIGURE 9.11 During the valgus extension overload test, the elbow is repeatedly forced into extension by the examiner while valgus stress is also applied in an effort to mimic the acceleration phase of throwing.
There are several provocative tests that have been described to help localize the site of median nerve compression. If symptoms are aggravated by flexion of the elbow against resistance between 120 and 135 degrees of flexion, the site of compression is likely to be the ligament of Struthers. Resisted elbow flexion and forearm supination may provoke symptoms if compression is at the area of the bicipital aponeurosis and lacertus fibrosis. If the site of compression is the arch of the flexor digitorum superficialis muscle, resisted flexion of the proximal interphalangeal joint of the middle finger will provoke symptoms (58).
If the location of compression is specifically at the pronator teres, resisted pronation of the extended elbow will compress the median nerve between the heads of the pronator teres and will provoke symptoms (59). Additionally, palpation of the anterior compartment of the forearm may reveal localized tenderness over the proximal third of the pronator teres. The pronator compression test involves manual compression of the median nerve at or near the pronator teres. When positive, the patient reports a recreation of his or her symptoms (60). Patients may also have a positive Tinel percussion test about the pronator teres.
Anterior interosseous syndrome causes deep pain in the proximal forearm and motor weakness in the hand in the absence of sensory symptoms. The most frequent cause of entrapment is the result of the presence of fibrous bands in the pronator teres muscle or constriction about the ulnar head of the pronator teres as it crosses the posterolateral aspect of the anterior interosseous nerve as it branches off the median nerve. Patients note a lack of finger dexterity or weakness in their thumb tip to index tip pinch (the Kiloh-Nevin sign) (61). Clinically, patients have a loss of function of the flexor pollicis longus and flexor digitorum profundus to the index and middle fingers and weakness of the pronator quadratus. Pronator quadratus function may be tested by flexing both elbows past 90 degrees and resisting forearm pronation. In contrast to pronator syndrome, pain may be elicited by resisted flexion of the flexor digitorum superficialis of the long finger and may also be present at rest and on local palpation of the nerve. No sensory changes occur, and the hand assumes a characteristic posture such that the patient is unable to position the thumb and index finger in the shape of a circle or “OK” sign as a result of the inability of the patient to flex the distal interphalangeal joint of the index finger and the interphalangeal joint of the thumb.
Radial Nerve Entrapment Syndromes
The radial nerve also follows a complex course as it travels distally past the elbow. Above the elbow, the radial nerve courses distally along the humerus and passes from the posterior to the anterior compartment of the arm through the lateral intermuscular septum, a potential site of compression. The radial nerve then splits into a superficial branch and a deep branch under the brachioradialis and the extensor carpi radialis longus muscles. The sensory superficial branch continues beneath the brachioradialis into the forearm, passing between the brachioradialis and the flexor carpi radialis in the distal third of the forearm. The deep branch of the radial nerve (the posterior interosseous branch) passes through the radial tunnel, an area of potential compression. The radial tunnel is composed of the anatomic structures between the radiohumeral joint and the distal aspect of the supinator muscle. Potential sites of compression within the radial tunnel include the fibrous bands at the entrance to the radial tunnel at the level of the radiocapitellar joint, the radial recurrent artery leash of vessels (the “leash of Henry”), the fibrous margin of the extensor carpi radialis brevis muscle, the arcade of Frohse where nerve passes through the proximal portion of the supinator muscle, and a fibrous band at the distal margin of the supinator muscle. Once through the supinator, the deep branch of the radial nerve divides further into superficial and deep components. The superficial branch courses medially, innervating the extensor digitorum, the extensor digiti minimi, and the extensor carpi ulnaris muscles. The deep branch continues distally to supply the abductor pollicis longus, the extensor pollicis brevis, the extensor indicis proprius, and the extensor pollicis longus (57).
Radial tunnel syndrome occurs as a result of compression of the posterior interosseous nerve in the radial tunnel. It may be seen in manual laborers or in athletes who perform repetitive rotatory movements of the forearm such as rowers, tennis players, or discus throwers. Pain is the most common primary presenting symptom in radial tunnel syndrome, because objective findings of sensory or motor loss are absent. Roles and Maudsley (61) were the first to describe radial tunnel syndrome in a patient with resistant tennis elbow. Examination of patients presenting with radial tunnel syndrome will reveal a point of maximal tenderness at the site of compression, which is usually located over the supinator at the level of the arcade of Froshe (63). At any of the potential sites, compression of the radial nerve is greatest with the elbow extended, the forearm pronated, and the wrist flexed. Resisted extension of the middle finger with the elbow extended may produce pain at the site of tenderness (62, 64). Additionally, active wrist extension and forearm supination against resistance may reproduce the pain.
Although radial tunnel syndrome results in purely subjective reports of pain, posterior interosseous nerve syndrome presents as a partial or complete paralysis of the musculature innervated by the posterior interosseous nerve. The syndrome is the result of compression of the posterior interosseous nerve, including the areas of compression seen in radial tunnel syndrome. Other causes of compression include elbow synovitis caused by rheumatoid arthritis and benign tumors. Partial lesions occur when only one nerve branch is involved. Compression of the superficial or medial branch may cause paralysis of the extensor carpi ulnaris, extensor digiti quinti, and extensor digitorum communis. Compression of the lateral branch may cause paralysis of the abductor pollicis longus, extensor pollicis brevis, extensor pollicis longus, and extensor indicis proprius.
Patients with posterior interosseous nerve syndrome occasionally report deep forearm or lateral elbow pain, but the most common finding is that of motor weakness. Weakness or paralysis affects finger extension at the metacarpophalangeal joints, thumb extension, and thumb abduction with the wrist in a neutral position. Because extensor carpi radialis longus function is preserved (its innervation is provided by the radial nerve above the level of the posterior interosseous nerve), the wrist extends and deviates radially because it is not opposed by the extensor carpi ulnaris.
Ulnar Nerve Entrapment Syndromes
Ulnar neuropathy is the most common nerve problem in the elbow. The boundaries for potential ulnar nerve compression about the elbow begin approximately 10 cm proximal to the elbow and end approximately 5 cm distal to the joint. The ulnar nerve can be compressed along this pathway at any of five sites.
The first area of potential compression begins proximally at the arcade of Struthers and ends distally near the medial epicondyle. Thearcade, which runs obliquely and superficial to the ulnar nerve, is composed of the deep investing fascia of the arm, superficial muscle fibers from the medial head of the triceps, and the “internal brachial ligament,” which arises from the coracobrachialis tendon.
The second site of potential compression is the distal end of the humerus at or just proximal to the medial epicondyle. Compression in this area develops as a consequence of a valgus deformity of the bone secondary to an old epiphyseal injury to the lateral condyle or a malunited supracondylar fracture (65).
The third area of potential compression is the epicondylar or olecranon groove. Compression at this site can be caused by a wide variety of lesions and conditions, which can be grouped into three categories: lesions within the groove, conditions outside the groove, and conditions that predispose the nerve to sublux or dislocate from the groove (65).
The fourth site of potential compression is where the nerve passes through the cubital tunnel between the humeral and ulnar heads of the flexor carpi ulnaris muscle. This site and the epicondylar groove are the most common sites for ulnar nerve compression. The floor of the tunnel is the ulnar collateral ligament of the elbow. Its roof is “Osborne’s ligament,” a fibrous band that is a continuation of the fibroaponeurotic covering of the epicondylar groove. The nerve is vulnerable to compression within the cubital tunnel during elbow flexion, because the tunnel normally narrows as Osborne’s ligament stretches and becomes taut and the ulnar collateral ligament relaxes and bulges medially (65–67).
The fifth site of potential compression is where the ulnar nerve leaves the flexor carpi ulnaris. Normally, the nerve enters the muscle at the cubital tunnel, remains intramuscular for a distance of approximately 5 cm, and then penetrates a fascial layer to lie between the flexor digitorum superficialis and the flexor digitorum profundus. The nerve can be constricted by this fascia, which has been referred to as the “flexor pronator aponeurosis” (65, 66).
Ulnar nerve compression symptoms can vary from mild numbness and paresthesias in the ring and little fingers to severe pain on the medial aspect of the elbow and dysesthesias radiating proximally and distally. Patients with early stages of nerve compression may not report any actual weakness, although they may be aware of some clumsiness or heaviness of the hand. With subluxation or dislocation of the ulnar nerve, the patient may report a painful snapping or popping sensation over the medial side of the elbow when flexing and extending their elbow combined with shooting pains radiating to the ulnar digits.
In examining a patient with symptoms of ulnar nerve compression, the ulnar nerve is first palpated along its course to detect any potential compressive masses and also to detect the location of maximal tenderness, which aids in identifying the potential site of compression. Gently tapping on the nerve in the areas of potential compression may elicit a sensation of paresthesias distally, or a positive Tinel’s sign, suggestive of ulnar nerve irritation. Another provocative test for ulnar nerve compression involves maintaining the elbow in full flexion with the wrist in full extension for 1 minute (69). The test is considered positive if paresthesias or numbness occurs in the ulnar nerve distribution, although the test does not have high specificity. Numbness in the ulnar nerve distribution of the hand is a common finding. The sensory deficits usually include both sides of the little finger and the ulnar half of the ring finger. A sensory deficit over the dorsoulnar aspect of the hand and the dorsum of the little finger aids in differentiating ulnar neuropathy resulting from compression at the elbow versus at the wrist. When nerve compression occurs at the wrist in Guyon’s canal, dorsoulnar sensation remains intact because the area is innervated by the dorsal sensory branch of the ulnar nerve, which leaves the main body of the nerve at a more proximal level (65).
Muscle weakness generally occurs later than numbness, although the inability to adduct the little finger (Wartenberg’s sign) occasionally presents early. Weakness affects the intrinsic muscles in the hand more commonly than the extrinsic muscles in the forearm (70). A useful test for ulnar nerve function is the “crossed fingers” test, in which the patient is asked to cross his or her middle finger over the index finger. Chronic nerve compression may eventually result in intrinsic weakness and muscle wasting. Muscle weakness in these cases is commonly associated with clawing of the ring and little fingers and weakness of key pinch. The patient may exhibit a positive Froment’s sign (the patient compensates for weak pulp–to-pulp pinch between the thumb and index finger by flexing the interphalangeal joint of the thumb) and a positive Jeanne’s sign (hyperextension of the metacarpophalangeal joint of the thumb). When extrinsic weakness occurs, it always involves the flexor digitorum profundus to the little finger (Pollock’s test). The flexor digitorum profundus to the ring finger may also be weak, but usually not to the same degree.
Finally, attempts should be made to check for ulnar nerve subluxation or dislocation. The stability of the nerve is best tested with the patient supine or seated and the arm abducted 90 degrees and externally rotated. The elbow is flexed from 20 to 70 degrees repeatedly while the physician observes and feels for subluxation of the nerve (71–73). In positive cases, the nerve will sublux out of its groove during elbow flexion and reduce into its groove in extension.
Conclusion
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree