Foreign Bodies
INTRODUCTION
Identification and removal of foreign bodies can be extremely challenging in some circumstances. Plain film radiography has traditionally been the imaging modality of choice for most foreign bodies. Foreign bodies that are not radiopaque are not visualized by these methods. Ultrasound is an excellent modality for identifying foreign bodies. It has high resolution and can frequently be used to identify the nature of the foreign body by the echotexture and surrounding artifact. It is also excellent for identifying the effect of the foreign body on the surrounding tissue. Ultrasound is also the ideal imaging modality for dynamic guidance for removal of the foreign body.
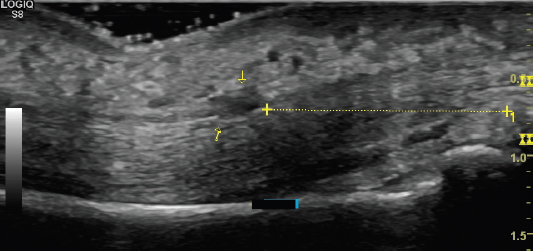
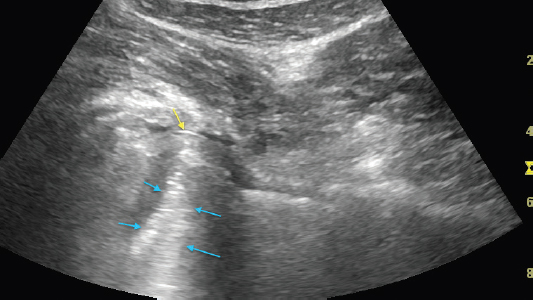
Identifying the size and relationship to other tissue can provide useful information prior to removal. Precise localization helps to minimize any surgical exploration or improve the approach to percutaneous removal (Figure 12.1). Most foreign bodies are hyperechoic with a hypoechoic ring of reactive tissue around it (Figure 12.2). Reverberation artifact is typical for foreign bodies and aids in detection (Figure 12.3). The posterior artifact tends to become larger and more irregular with larger foreign bodies. Reverberation artifact is discussed in more detail in Chapter 13. Detecting surrounding inflammation or infection also provides valuable information for the clinical approach Figure 12.4).
Detailed discussion of the nature of various foreign bodies is beyond the scope of this text. Metal, wood, and glass are some of the most commonly encountered foreign bodies and have some distinguishing characteristics.
FIGURE 12.1 Sonogram demonstrating an example of precise localization of a foreign body (yellow arrows) just superficial to the flexor digitorum profundus tendon. The linear measurement is used to provide precise distance from the midportion of the proximal interphalangeal joint.
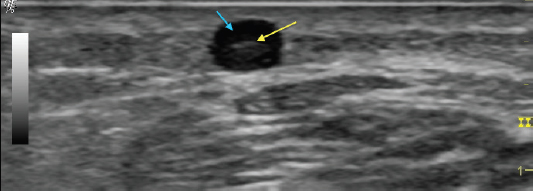
FIGURE 12.2 Sonogram demonstrating a relatively hyperechoic foreign body (yellow arrow) with an anechoic ring of reactive fluid around it (blue arrow).
FIGURE 12.3 Sonogram demonstrating reverberation artifact (blue arrows) deep to metal artifact (yellow arrow). Reverberation artifact occurs when the sound waves bounce between two interfaces with very high impedance, such as foreign bodies.
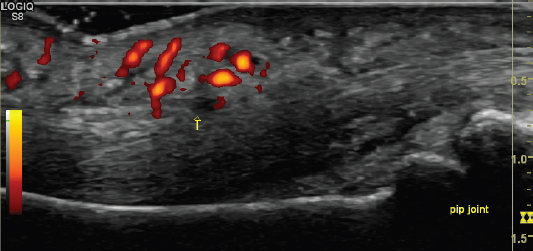
FIGURE 12.4 Sonogram demonstrating significant inflammatory reaction with increased Doppler signal around a foreign body (yellow arrow).
METAL
Metal appears hyperechoic and tends to have the most reverberation artifact of the foreign bodies (Figure 12.5).
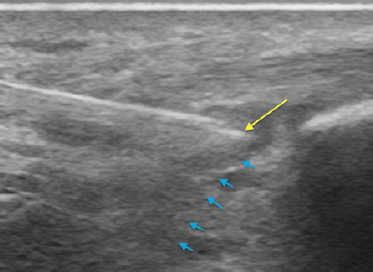
FIGURE 12.5 Sonogram demonstrating the reverberation artifact seen with metal as a foreign body. The tip of the needle is shown (yellow arrow) with the reverberation artifact deep to that (blue arrows).
WOOD
Wood initially appears hyperechoic but tends to become more hypoechoic over time. The foreign body itself can become somewhat less conspicuous, however, the reactive tissue around it tends to become more prominent. Wood tends to have a fairly large amount of posterior shadowing (Figure 12.6).
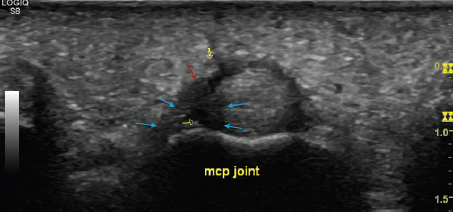
FIGURE 12.6 Sonogram demonstrating the appearance of a small wood splinter (red arrow) positioned against the flexor digitorum profundus and superficialis tendons (seen in short axis). Both reactive tissue edema (yellow arrows) is seen as well as posterior shadowing (blue arrows). In this case, the splinter had been present for many weeks and note that the wooden foreign body itself is relatively hypoechoic.
GLASS
Glass generally appears hyperechoic with a relatively small amount of posterior reverberation (Figure 12.7).
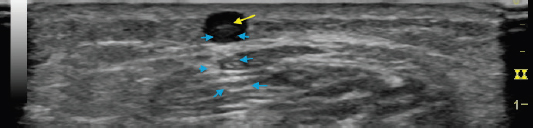
FIGURE 12.7 Sonogram demonstrating the appearance of a small sliver of glass (yellow arrow). Note that there is a combination of a small degree of reverberation artifact and shadowing (blue arrows). The reverberation artifact (seen best just beneath the glass sliver within the anechoic circle) is much less than is seen with metal. The posterior shadowing is significantly less than typically seen with wood.
Ultrasound can be used to assist with needle guidance when percutaneous removal of the foreign body is desired. This allows simultaneous visualization of the needle and foreign body in real time. It is generally best to approach this procedure with the needle in-plane with respect to the orientation of the transducer. See Chapter 14 for a detailed discussion on needle guidance with ultrasound.
REMEMBER 
1) It is helpful to not only assess the appearance of the foreign body, but also the extent of the surrounding tissue reaction and the degree and nature of the posterior artifact.
2) Precise localization and measurement of the foreign body should be performed to maximize the ease of removal.
3) Use Doppler imaging to assess the degree of inflammation, and also consider the possibility of infection.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree