Abstract
Gestational trophoblastic disease refers to a spectrum of disorders that results from abnormal proliferation of the trophoblastic epithelium. These include premalignant disorders (hydatidiform moles) and malignant ones (persistent/invasive gestational trophoblastic neoplasia, placental site trophoblastic tumors, epithelioid trophoblastic tumors, and choriocarcinoma). Most present with abnormal beta hCG levels and an abnormal ultrasound. Before treatment, laboratory evaluation and imaging of the chest, abdomen, and pelvis is recommended to determine the appropriate course and follow-up.
Keywords
gestational trophoblastic disease, hydatidiform mole, placental site trophoblastic tumor, chemotherapy, multiple pregnancy, fetus, treatment
Introduction
Gestational trophoblastic disease (GTD) is a spectrum of disorders arising from abnormal proliferation of the trophoblastic epithelium of the placenta. There are several histologically distinct types of GTD that range from premalignant, complete, and partial hydatidiform moles (HMs), to malignant diseases, also known as gestational trophoblastic neoplasia (GTN), which includes persistent/invasive GTN, placental site trophoblastic tumors, epithelioid trophoblastic tumor (ETT), and choriocarcinoma. Choriocarcinoma is discussed separately ( Chapter 100 ).
Disease
Prevalence and Epidemiology
The incidence of GTD varies in different regions of the world. Within North America, Australia, and Europe, the incidence of HM is between 5.7 : 10,000 and 11 : 10,000 pregnancies. In contrast, in Southeast Asia and Japan, incidence is as high as 20 : 10,000 pregnancies. The two main risk factors include maternal age with an increased risk in women over age 35 and under 20, as well as a history of previous GTD. The risk of recurrence is 1%–2% following the first molar pregnancy, about 10–20 times the risk for the general population. There is also an increased risk for both a complete and partial mole in women with a history of prior spontaneous abortion and infertility. Inverse relationships between beta-carotene and a high animal-fat, diet with molar pregnancy are the only consistent environmental associations observed.
There are cases reported of a complete or partial mole arising with a coexistent fetus, although this is rarely occurring in 0.1 : 10,000 to 0.5 : 10,000 pregnancies. The majority of cases resulted in spontaneous or elective termination of pregnancy because of severe maternal complications including preeclampsia, thyrotoxicosis, or hemorrhage.
Placental site trophoblastic tumor (PSTT) is a rare form of GTN. It constitutes about 1%–2% of trophoblastic disease.
Etiology and Pathophysiology
GTD occurs after abnormal growth and fertilization with a proliferation of trophoblastic tissue. Complete moles have no identifiable embryonic or fetal tissue. Histologically, the chorionic villi have diffuse trophoblastic hyperplasia with marked atypia and generalized swelling. About 90% of complete moles are euploid and homozygous, arising from an anuclear ovum that has been fertilized by a haploid (23X) sperm, which then replicates its own chromosomes resulting in the most common karyotype 46XX, or by fertilization by two sperm (46XY or 46XX).
A partial mole is the result of fertilization of a haploid ovum by two sperm or duplication of one sperm, resulting in a triploid karyotype: 69XXY (most common), 69 XXX, or 69 XYY. It is characterized by chorionic villi that vary in size and have focal swelling with trophoblastic hyperplasia and mild atypia at the implantation site, and identifiable fetal or embryonic tissue. This can result in misdiagnosis of an incomplete or missed abortion, with the correct diagnosis made only after pathology review of the specimen.
Malignant GTD is diagnosed when there is clinical, radiologic, pathologic, or hormonal evidence of persistent or invasive trophoblastic tissue. Malignant forms include invasive GTN, choriocarcinoma, and PSTTs. The diagnosis is most commonly made following a molar pregnancy but can occur after any type of gestation. Any of the malignant forms of GTD can metastasize, most commonly to the lungs and/or vagina.
Locally invasive GTN develops in 15%–20% of patients following evacuation of a complete mole and less frequently after other gestations (<5% after partial mole). These may perforate through the myometrium or invade the uterine vessels, causing intraperitoneal or vaginal hemorrhage.
PSTTs are extremely rare, and can occur months or years after a term gestation, spontaneous abortion, or a molar pregnancy. Most cases of PSTT are diploid with an XX genomic composition in 90%; however, a few cases of tetraploidy have also been reported. PSTTs are tumors of the intermediate trophoblasts—a transitional form between cytotrophoblasts and syncytiotrophoblasts—with a gross appearance of a gray/yellow circumscribed mass, often containing areas of hemorrhage. The intermediate trophoblasts form sheets or nests of cells that invade the uterus and divide individual myometrial fibers. They can also extensively invade both blood vessels and lymphatic channels.
ETT is a rarer variant of PSTT, and appears to arise from malignant transformation of intermediate trophoblasts. Most ETTs are diagnosed many years after full-term delivery.
Manifestations of Disease
Clinical Presentation
In the past, complete moles were typically diagnosed in the second trimester, most commonly with signs/symptoms of excessive uterine size for the gestational age, vaginal bleeding, and hyperemesis. However, with the availability of accurate and sensitive tests for human chorionic gonadotropin (hCG) and the use of early ultrasound (US), the diagnosis is now made in the first trimester, before the classic signs or symptoms. Previous symptoms at presentation of a partial mole included vaginal bleeding and a uterine size that is small or appropriate for the gestational age, worrisome for incomplete or missed abortion.
Partial or complete moles with a coexistent fetus can be diagnosed by US findings of a complex, cystic placental component distinct from the fetoplacental unit or can present with vaginal bleeding or uterine size larger than the gestational age. Compared with singleton HMs, twin pregnancies with a fetus and a mole carry an increased risk for postmolar GTD, with a higher proportion of patients having metastatic disease and requiring multiagent chemotherapy. Many patients that continue such pregnancies develop early complications leading to termination of the pregnancy before fetal viability.
The majority of PSTT and ETT remain confined to the uterus at the time of diagnosis with only 10%–15% being clinically malignant. Symptoms can present weeks to years after the preceding pregnancy and most commonly occur as vaginal bleeding and enlargement of the uterus. Metastases are most commonly in the lung but have also been reported in the brain, stomach, liver, spleen, bowel, pancreas, kidney, and adjacent pelvic organs. The International Federation of Gynecology and Obstetrics (FIGO) staging determines prognosis. Patients with disease confined to the genital tract (stage I and II) have over 90% survival, whereas stage III and IV have only 33% survival. Disease localized to the uterus and diagnosis less than 2 years from the antecedent pregnancy are associated with a better outcome. Vascular space involvement, endomyometrial invasion, and brain metastases are poor prognostic factors.
Imaging Technique and Findings
Ultrasound.
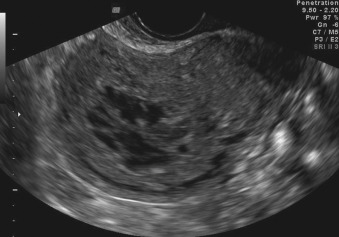
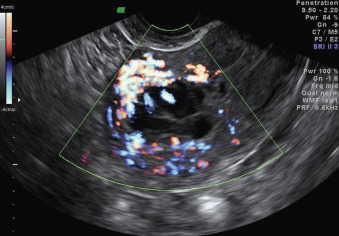
Ultrasonographic findings of a complete mole include absence of an embryo or fetus, absence of amniotic fluid, and a central heterogeneous mass containing multiple anechoic spaces, previously described as a “snowstorm” appearance ( Figs. 104.1 and 104.2 ). The smaller cystic areas correspond to the hydropic villi. Prior studies have demonstrated a 70%–90% sensitivity of pelvic US for the diagnosis of complete mole, with improved detection rates as gestational age increases. A partial mole often demonstrates either enlarged cystic spaces, and/or increased echogenicity within the placenta with a coexistent embryo or fetus ( Figs. 104.3 and 104.4 ). If the fetus is viable, it is often growth restricted, and the amniotic fluid volume is often reduced. It is therefore diagnosed as a missed or incomplete abortion in 15%–60% of cases.