Section I
BOARD IMAGES

1. A 45-year-old woman presents to clinic with a new pruritic rash on the flexor surface of her left forearm. Her medical history is significant for Wilson disease, and she was recently started on penicillamine, a copper-chelator. On exam she has Kayser-Fleischer rings in both eyes and purple, polyangular papules on her left forearm. On closer inspection, fine white streaks cover the surface of the papules. A clinical diagnosis of lichen planus is made. Penicillamine is discontinued. What is the best treatment option at this time?
2. A 36-year-old man presents to the clinic with a pruritic rash on his scalp, neck, and back. His social history is significant for intravenous (IV) drug use. On exam, violaceous, polygonal papules are noted in clusters on the scalp, neck, and back. White striae are noted on the lesional surfaces. On buccal mucosa there are tender, dendritic, lacy, white lesions bilaterally. Which of the following is/are true regarding his diagnosis?
A. Can be associated with chronic HCV
B. Disease is treated with oral steroids
D. Disease is treated with topical steroids
1. The answer is E: B and C only. This patient has lichen planus (LP) as a cutaneous inflammatory reaction to penicillamine. Clinical identifiers for LP include the Four Ps (purple, polygonal, pruritic, papules), as well as Wickham striae, the fine white lines covering the papules. Other drug exposures that have been linked with LP include gold, chloroquine, and methyldopa. This is a local rash, so the best initial treatment would be topical steroid and oral antihistamine for relief from itching (E). Oral steroids and more potent immune modulators (azathioprine, cyclosporine) should be used with more generalized, systemic LP.
2. The answer is E: All of the above. This patient has oral and cutaneous lichen planus (LP) most likely related to chronic HCV status. Biopsies on dermal and oral lesions reveal mononuclear cells at the dermoepidermal junction and a T cell–mediated cytotoxic reaction against keratinocytes. HCV is thought to trigger LP via dermal and mucous membrane replication. LP usually affects flexor surfaces such as the wrists, pretibial shafts, scalp, trunk, and glans penis, and may also involve the buccal mucosa, tongue, and lips. This patient has local cutaneous lesions that could be treated with topical steroids. However, due to his buccal mucosa LP he should be started on a short course of oral prednisone (E). Antihistamines should also be used to treat pruritis. The course of LP is largely unpredictable, ranging from spontaneous remission to chronic eruption.
Lichen planus is a common, distinct inflammatory disorder that affects the skin, mucous membranes, nails, and hair. Lesions appear as symmetric, grouped, erythematous to violaceous, flat-topped, polygonal papules. Close inspection of the lesions with a hand lens and after application of mineral oil will reveal fine white lines (Wickham striae). Etiology of the dermatosis is perse and includes drugs, metals, and infections (especially hepatitis C), which result in alterations of cell-mediated immunity. Women are affected more often than men, and the typical age of onset is between 30 and 60. Trauma may cause the Koebner phenomenon and linear arrangements. Treatment is with topical and systemic corticosteroids or cyclosporine.
▪ Four Ps: purple, polygonal, pruritic, papules
3. A 47-year-old man presents with a painless enlarging mass on the back of his right upper leg. He has no tenderness over the area, and the mass is firm on palpation. A biopsy reveals a leiomyosarcoma. All of the following are true except:
A. This tumor grows by direct local extension.
B. This tumor is derived from mature fat cells.
C. This tumor is derived from embryonic mesoderm.
D. Treatment options are guided by biopsy results.
E. The main prognostic factors are tumor grade and tumor size.
3. The answer is B: This tumor is derived from mature fat cells. Tumors or mature fat cells (B) are seen in benign lipomas rather than sarcomas. This man has a leiomyosarcoma, which is a malignant cancer derived from embryonic mesoderm (C). This tumor grows by direct local extension (A). Treatment options are guided by biopsy results (D) and the main prognostic factors are tumor grade and tumor size (E). Thus all of the above are true of sarcomas except (B).
A sarcoma is a malignant neoplasm that arises from mesenchymal embryonic cells and affects connective tissue cells such as bone, cartilage, muscles, blood vessels, or fat cells. Sarcomas can be pided into two groups: those derived from bone and those derived from soft tissue. These tumors are often highly aggressive, and biopsy is required for identification of cancer cells and to guide treatment. Imaging such as ultrasound, computed tomography (CT), or magnetic resonance imaging (MRI) may be useful before biopsy is performed. Treatment options include surgical excision, radiation, and chemotherapy. In adults the most common histopathologic subtypes are liposarcoma and leiomyosarcoma, and the most common sites of origin are the thigh, buttock, and groin. In children, small cell sarcomas (e.g., Ewing sarcoma, embryonal rhabdomyosarcoma, and primitive neuroectodermal tumor) are most common.
Kaposi sarcoma (KS) is the only sarcoma that is associated with a virus.
▪ Grows by direct local extension
▪ Soft tissue sarcoma that often presents as painless, enlarging mass
▪ Main prognostic factors are grade and tumor size.
▪ Radiation exposure is a risk factor for soft tissue sarcomas.
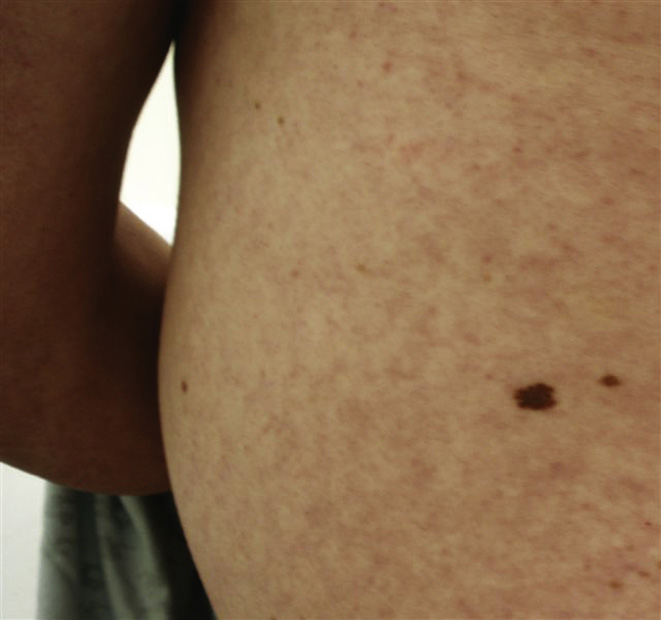
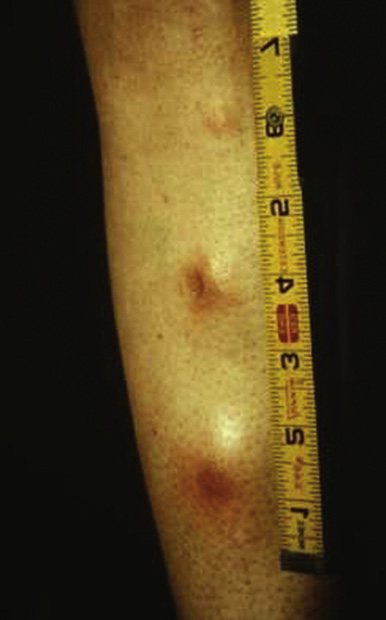
4. A 33-year-old man comes to the clinic in the winter with complaints of dry, itchy skin on his forearms (shown above) and eyelids, as well as in the creases of his elbows and knees. His past medical history is significant for mild, persistent asthma and seasonal allergies. He says that since childhood this problem has occurred annually in winter, when his asthma is also worse than usual. During the visit he is visibly uncomfortable and often scratches his arms. Which of the following should be considered when using a topical corticosteroid to treat this condition?
A. Topical corticosteroids are contraindicated in the setting of secondary staphylococcal infection.
B. Skin bleaching can occur with chronic use.
C. Application near the eye increases risk for ocular side effects.
D. Application over a large surface area can cause systemic corticosteroid effects.

5. A 27-year-old man complains of an itchy rash on his face. The rash appeared just after he returned from a day at the beach. He recently bought a new sunscreen that he first used two weeks ago. He used the same sunscreen on his face during his most recent trip to the beach. He has had similar rashes throughout his life. He has a history of hay fever and mild asthma. Other than discontinuing use of the sunscreen, which of the following preventive measures should be recommended?
A. Limit the number of showers per day
D. Apply topical corticosteroid daily
E. Apply antibacterial ointment daily
4. The answer is E: All of the above. This patient has atopic dermatitis (eczema). The classic triad of atopic disease includes asthma, allergic rhinitis, and atopic dermatitis. Topical corticosteroids are used to treat subacute, scaly lesions or chronic, dry, lichenified lesions of atopic dermatitis. They must, however, be used with caution for all of the reasons listed above (E). Patients with eczema are at an increased risk of developing a secondary infection, commonly due to staphylococcus, which is a contraindication to topical corticosteroids. Chronic use of topical corticosteroids may cause skin bleaching, and the risk of systemic side effects increases with application over a large surface area or in smaller inpiduals. Use on the eyelids is not recommended due to the risk of developing cataracts or glaucoma.
5. The answer is A: Limit the number of showers per day. Prevention of atopic dermatitis (eczema) includes avoidance of known triggers. In this case, sunscreen triggered the most recent reaction; however, other agents may have been associated with the patient’s past rashes. Patients should not take hot baths (C) or multiple showers per day (A), and they should avoid drying soaps (B). Topical steroids can be used for subacute and chronic reactions but not as a preventive measure (D). Steroids should be used with caution on the face. Eczema puts patients at increased risk of secondary bacterial infection, but prophylaxis with a topical antibacterial ointment is typically not indicated (E).
Atopic dermatitis is an inflammatory skin disease. It stems from a mixture of genetic susceptibility, defects in the innate immune system, and increased immunologic responses to allergens. Most patients show signs of skin disease before age 5. Lesions have a different appearance based on the duration (acute versus subacute versus chronic) and the age of the patient. Young patients often have a rash on the face and extensor surfaces, while adults have a rash on the flexural surfaces of the elbows and knees.
▪ Decreased skin barrier protection leads to an increased risk of secondary bacterial infection.
▪ Preventive treatment includes moisturizers and avoidance of known triggers.
▪ Subacute or chronic lesions are treated with topical corticosteroids.
6. A 20-year-old man presents with a 0.5-cm flat nonpalpable hyperpigmented lesion on his trunk. How would you classify his primary skin lesion?
7. A 75-year-old woman presents with several lesions on the dorsal surface of both of her hands. These hyperpigmented lesions are flat and nonpalpable, have distinct borders, and range from 0.1 to 0.8 cm in size. Which of the following best classifies this primary skin lesion?
6. The answer is A: Macule. This patient has a macule (A) because it is a flat lesion less than 10 mm in diameter. A patch (B) is a larger nonpalpable lesion greater than 10 mm. Plaques (C) are elevated palpable lesions greater than 1 cm. Papules (D) are palpable lesions less than 5 mm. Lichenification (E) is a secondary skin lesion characterized by epidermal thickening. Visible and palpable skin thickening is often present with accentuated skin markings.
7. The answer is D: Macule. This patient has several macules (D) on the dorsal surface of her hands, likely representing benign lesions called solar lentigines. The term macule is used to classify any flat lesion of less than 10 mm in diameter that is even with the surface of surrounding skin and differs in color from the surrounding skin or mucous membrane. Macules may be hyperpigmented, hypopigmented, or depigmented. Patches (A) are larger, flat nonpalpable lesions measuring greater than 10 mm in size. Plaques (B) are elevated palpable lesions greater than 10 mm. Papules (C) are palpable lesions less than 5 mm. A nodule (E) is a solid, round, or ellipsoidal palpable lesion with a diameter larger than 5 mm. Nodules are differentiated from papules and plaques by depth of involvement and/or substantive palpability.
A macule is a primary skin lesion defined by a nonpalpable change in surface color without elevation or depression that is generally less than 10 mm in size.
▪ Flat, nonpalpable, less than 10 mm
▪ Examples include vitiligo, tinea versicolor, café au lait spots, mongolian spots, freckles.
8. A 69-year-old man presents with several exophytic, brown papules and plaques that appear as though they could be scraped off. What typical finding would you expect to see on histology?
A. Islands of proliferating epithelium resembling the basal layer of the epidermis
B. Hyperplasia of benign, basaloid epidermal cells with horn pseudocysts
C. Focal increase in melanocytes
D. Intraepidermal atypia over a sun-damaged dermis
E. Intraepidermal atypical keratinocytes with penetration of the basement membrane
9. A 74-year-old man comes to you, his new primary care physician, after being urged by his granddaughter to get some spots on his back looked at. Physical exam demonstrates numerous “stuck-on,” waxy, verrucous papules and plaques of various sizes and colors. Which of the following is correct regarding this man’s condition?
A. These growths originate in keratinocytes.
B. Similar to warts, these lesions are viral in origin.
C. These lesions, if left untreated, may progress to melanoma.
D. Histologic examination would demonstrate a focal increase in melanocytes.
E. These growths could have been avoided if adequate preventive measures had been taken.
8. The answer is B: Hyperplasia of benign, basaloid epidermal cells with horn pseudocysts. These warty, brown lesions with a “stuck-on” appearance are seborrheic keratoses. Biopsy would show hyperplasia of benign, basaloid epidermal cells with horn pseudocysts (B). Horn pseudocysts are virtually pathognomonic. Islands of proliferating epithelium resembling the basal layer of the epidermis (A) is the histologic finding in basal cell carcinoma. A focal increase in melanocytes (C) is seen in lentigo. Intraepidermal atypia over a sun-damaged dermis (D) is seen in actinic keratosis. Intraepidermal atypical keratinocytes with penetration of the basement membrane (E) is indicative of squamous cell carcinoma.
9. The answer is A: These growths originate in keratinocytes. These warty brown lesions are seborrheic keratoses and originate in keratinocytes, hence the name (A). While these lesions are often referred to as seborrheic warts, there is not a viral association (B). These lesions are benign in nature and do not commonly progress to melanoma (C). A focal increase in melanocytes is seen in lentigo (D). While preventive measures such as sunscreen use and protective clothing are useful to prevent malignant skin lesions, seborrheic keratoses, commonly referred to as age barnacles, are simply a product of aging.
Seborrheic keratoses are raised 3- to 20-mm lesions with a stuck-on appearance. They can be flat or raised and typically have a velvety or warty surface. Although the lesions are often hyperpigmented, they range in color from light tan to black. These benign epidermal growths are a result of proliferation of immature keratinocytes. They tend to develop after age 50. Atypical lesions can be biopsied to rule out cancer. Shave biopsy reveals horn cysts which are virtually pathognomonic. Usually no treatment is necessary, but surgical excision is an option for cosmetic reasons.
▪ Increased incidence with increasing age
10. On a routine well-child exam of an 8-year-old girl, the patient’s mother raises concern for her daughter’s susceptibility to skin cancer due to the patient’s fair complexion with many freckles on her face and extremities. The patient’s mother notes that her daughter’s skin burns easily when out in the sun. Most of the family is unable to tan with sun exposure. Her family history is significant for a maternal grandmother with basal cell carcinoma and paternal aunt with melanoma. On exam the patient is a healthy, fair-complexioned girl with light blue irides and areas of dense ephelides (freckles) on her face, shoulders, arms, and legs. You counsel the patient and her mother of her risk of skin cancer. Which of the following provide(s) effective prevention for skin cancer in this patient?
A. Avoid excessive sun and ultraviolet (UV) light exposure.
B. Use titanium dioxide and zinc oxide sunscreens.
C. Use hydroquinone to bleach freckles.
D. Use skin-covering clothing and hats.
10. The answer is F: Only A, B, and D. This patient exhibits the phenotype of those with the highest lifetime risk of skin cancer (melanoma, basal cell carcinoma, squamous cell carcinoma): fair skin with an abundance of freckles, light irides usually with blond or red hair, unable to tan, and easily sunburned. Exposure to ultraviolet A (UVA) and ultraviolet B (UVB) light poses a higher risk in these inpiduals. Frequent UV light exposure and blistering childhood sunburns put these inpiduals at higher risk for melanoma. Chronic UV light exposure correlates more with a higher risk of basal cell carcinoma and squamous cell carcinoma. Paramount to skin cancer prevention is avoiding and blocking exposure to UVA and UVB light (F). Hydroquinone has been shown to bleach freckles, but it offers no added protection from UV light.
An ephelis is commonly known as a freckle and first appears during childhood in fair-skinned inpiduals, presumably developing after sun exposure. When sun exposure is discontinued, the ephelides will typically fade or may even disappear. They represent an increase in melanin production in response to UV radiation exposure. It may be difficult to distinguish clinically between an ephelis and solar lentigo.
▪ Common on the central face and first noted in childhood
▪ More prominent after exposure to sunlight, fading after cessation of sunlight exposure
▪ Familial inheritance and more commonly seen in fair-skinned inpiduals
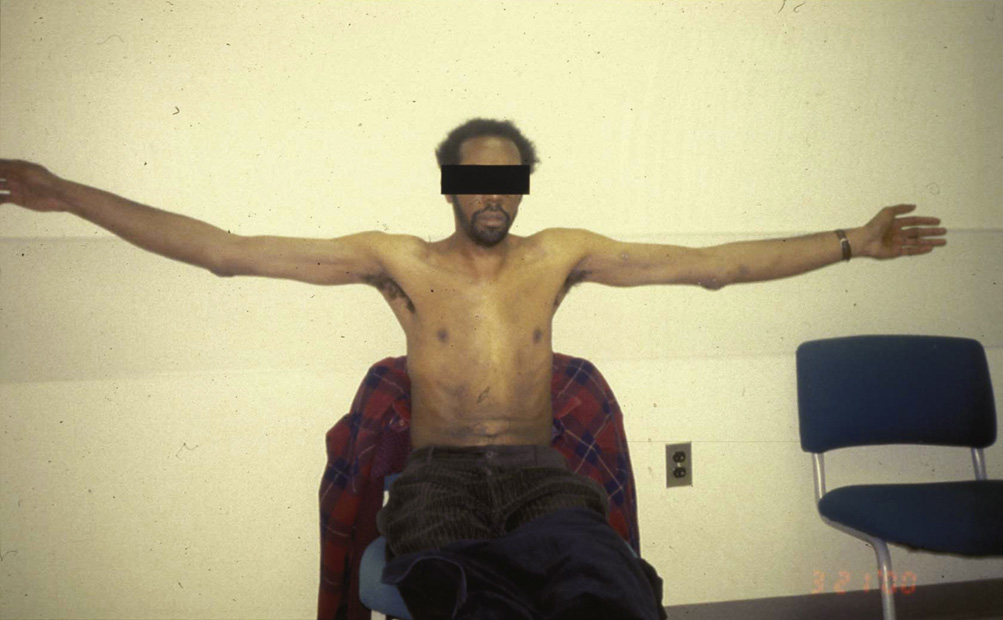
11. A 13-year-old girl presents to your clinic with the chief complaint of several red lumps on her back, arms, legs, and forehead which have been growing in number for 2 months. She adds that she has had coffee-colored marks on her skin since she was a toddler. Her past medical history is significant for a learning disability and recent onset of puberty. On physical exam the patient is Tanner stage 2 in breast and pubic hair development. She has eight café au lait spots on her trunk, numerous neurofibromas over her body, and axillary freckling. She is diagnosed with neurofibromatosis 1 (NF1). Which of the following can be used regarding management of this condition?
A. Imaging of the brain, orbits, chest, spine
D. Surgical removal of dermal neurofibromas
11. The answer is F: All of the above. This patient exhibits three of the diagnostic criteria for NF1: 1) Six or more café au lait spots; 2) two or more neurofibromas; 3) freckling in axillary/inguinal region; 4) optic gliomas; 5) two or more iris hamaratomas (Lisch nodules); 6) bony lesions (sphenoid dysplasia/pseudoarthroses); 7) first-degree relative with NF1. Only two of these criteria are needed for diagnosis of NF1. Patients should be referred to NF specialists who can use imaging, usually in the setting of neurologic deficits, to assess for gliomas, sphenoid dysplasia, pseudoarthroses, and spinal lesions. An annual ophthalmological exam is needed to assess for optic pathway gliomas and, to a lesser extent, Lisch nodules. The spine should also be evaluated regularly for signs of scoliosis. Dermal neurofibromas can be surgically removed for cosmetic reasons or for malignant degeneration. Finally all NF patients should receive genetic counseling, as this is an autosomal dominant disorder with 50% chance of inheritance in their offspring (F).
This patient has multiple skin-colored, soft papules and pedunculated nodules on her abdomen. These neurofibromatous lesions are seen in association with neurofibromatosis (NF), an autosomal dominant disease characterized by changes in the skin, nervous system, endocrine glands, and bones. Central nervous system (CNS) involvement occurs in 10% of patients with NF and consists of benign lesions including acoustic neuromas, meningiomas, optic glioma, and in some cases astrocytomas. Thus neurologic signs and symptoms should be approached with a high index of suspicion. Pheochromocytomas occur in 1% of patients, causing severe hypertension. Note café au lait (CAL) macules on abdomen, also a skin finding associated with NF.
▪ NF2 features include seizures, skin nodules, and CAL spots
12. A 34-year-old woman presents with thin-walled, fluid-filled blisters over her trunk and extremities. The blisters easily rupture. Her temperature on arrival is 102° F, and her blood pressure is 85/50. You note peeling skin over her palms and soles. The woman was treated 3 weeks ago for a urinary tract infection. The woman takes oral contraceptive pills, but she takes no other medications. Her last menstrual period just ended, and she used a new superabsorbent brand of tampons. What is the cause of this syndrome?
A. Bacterial-released exotoxins
B. Bacterial-released endotoxins
E. Antibodies directed against desmoglein molecules
13. A 33-year-old woman presents to the emergency department (ED) with sudden onset fever, chills, vomiting, diarrhea, muscle aches, and a diffuse rash. You are incredibly busy and have not had a chance to see this patient when the nurse alerts you that she has developed severe hypotension and is beginning to decompensate. You start supportive therapy and begin to take a history. She cogently asks you if you think this has anything to do with the sponge that she uses for contraception. She had placed the sponge a week ago and recalls that she forgot to take it out. Which of the following is the most likely cause of her symptoms?
12. The answer is A: Bacterial-released exotoxins. This woman has toxic shock syndrome (TSS), likely due to her use of superabsorbent tampons. TSS is caused by bacterial exotoxins (A). Most typically the exotoxins are released by Staphylococcus aureus, but can also be due to group A streptococcus. These exotoxins cause detachment within the epidermal layer. Bacterial endotoxins (B) are most often associated with gram-negative bacteria, which do not play a role in TSS. Medications (C) and a reaction to a viral infection (D), such as HSV, are common causes of Stevens-Johnson syndrome (SJS), which classically involveds the mucous membranes and oral mucosa. Antibodies directed against desmoglein molecules (E) causes pemphigus vulgaris.
13. The answer is D: Bacterial exotoxins. This patient is likely suffering from TSS due to the use of an intravaginal contraceptive device (sponge, an older form of contraception). Menstruating women, women using intravaginal contraceptive devices, people who have undergone nasal surgery, and persons with postoperative staphylococcal wound infections are all at risk for TSS. TSS is caused by bacterial exotoxins (D). Fever, chills, vomiting, diarrhea, and rapid, severe hypotension are characteristic of the initial course of TSS. Desquamation, particularly on the palms and soles, can occur 1-2 weeks after onset of the illness. Bacterial endotoxins (A) are most often associated with gram-negative bacteria, which do not play a role in TSS. Viral syndromes (B) and allergic reactions (C) are common causes of SJS, which classically involves the mucous membranes and oral mucosa. TSS is not due to an autoimmune reaction (E).
Toxic Shock (Staph Scalded Skin)

Toxic shock syndrome (TSS) is a rare, life-threatening complication of bacterial infection that has been most often associated with the use of superabsorbent tampons. Often TSS results from toxins produced by S. aureus, but it may also be produced by toxins produced by group A streptococcus. S. aureus releases epidermolytic exotoxins A and B, which cause detachment within the epidermal layer. These exotoxins are proteases that cleave desmoglein 1, which normally holds the granulosum and spinosum layers together. TSS presents with thin-walled, fluid-filled blisters that easily rupture. Symptoms may also include fever, low blood pressure, vomiting, diarrhea, or a rash, which may lead to desquamation (especially of the palms and soles).
▪ Detachment within epidermal layer
▪ Treat with antibiotics and supportive care
▪ Thin-walled blisters and desquamation of skin (particularly hands and soles)
14. A 54-year-old man is in the clinic for an annual visit. During the physical examination, he inquires about multiple red entities present on his chest, upper arms, and back, as shown above. The lesions are cherry red and 1 mm in diameter. They have been there for a few years according to the patient. He has no other health complaints and no significant past medical history. What is the best next step in workup for this patient?
A. Investigation for a visceral adenocarcinoma
B. Biopsies of the lesions to rule out malignancy
D. Elective laser removal or electrocoagulation
14. The answer is D: Elective laser removal or electrocoagulation. This patient has a normal finding of cherry angiomas, which represent benign vascular lesions that are more common with increasing age. The histology of the lesions consists of dilated capillaries and an edematous stroma with homogenization of collagen. They are extremely common in the elderly and have no clinical significance (A, B). However, lesions that generate cosmetic concern may be treated with laser therapy or electrocoagulation (D). These findings do not warrant more invasive treatment (C, E).
Cherry hemangiomas (or cherry angiomas) are common, asymptomatic, domed vascular lesions that vary in color from bright red to violaceous or black. They are found typically on the trunk, appearing around age 30 and increasing in numbers with age. They have no clinical significance but may pose a cosmetic concern. If desired, they can be treated with laser removal or electrocoagulation.
▪ Numbers increase with age but have no clinical significance.
15. A 12-year-old immigrant boy from Brazil presents to the clinic with 5 days of cough, conjunctivitis, fever, and runny nose. His mother brought him in today, alarmed by a rash that began on his head and progressed over his face and neck down his arms to his hands. His medical chart is significant only for absent MMR and Tdap vaccinations. On physical exam a diffuse erythematous, maculopapular rash is noted on his face, neck, chest, and upper extremities. On the buccal mucosa of the inner cheeks, bluish-white spots are noted on erythematous bases bilaterally at the level of the first molars. Which is/are the best treatment option(s) at this time?
16. A 3-year-old girl who has no vaccination records presents to an emergency Saturday clinic with a fever, constant cough, runny nose, conjunctivitis, diarrhea, and vomiting for 3 days. On exam the patient is febrile and appears acutely sick with cervical and occipital lymphadenopathy. On oral exam bluish-white spots surrounded by red are noted on the buccal mucosa of the inner cheeks. A clinical diagnosis of measles is made. Supportive care is begun. The next day the patient develops a maculopapular rash on her forehead, which erupts down her face, neck, trunk, and reaches her palms and soles. In discussing the course of the disease you tell her mother that in terms of acute complications, otitis media (AOM) is the most likely, and pneumonia is the most serious. Which of the following is/are known complications of her disease?
A. Subacute sclerosing panencephalitis
15. The answer is C: Supportive care. This patient with measles virus has the characteristic exanthem (maculopapular rash starting on the forehead and progressing down the face, neck, trunk, and extremities) after 2-4 days of cough, coryza, and fever. Koplik spots (bluish-white spots on red) develop on the buccal mucosa prior to the onset of the rash and are pathognomonic for measles. Measles IgM antibody is confirmatory. The best treatment in the immunocompetent patient is supportive care: hydration, antipyretics, and maintenance of oxygenation (C). Vitamin A is useful if the patient has symptoms of deficiency, malabsorption, malnutrition, or immunosuppression. Ribavirin antiviral could be used with an immunocompromised patient. Antibiotics are not indicated.
16. The answer is D: All of the above. This patient has measles due to lack of proper vaccination. Koplik spots (bluish-white spots on red on the buccal mucosa) occurring 1-4 days before the exanthem are pathognomonic for measles. Acutely the leading cause of death is pneumonia. AOM is the most common complication. Diarrhea can lead to dehydration. Subacute sclerosing panencephalitis is a rare, chronic form of measles infection in the CNS, causing fatal neurodegeneration 7-13 years following initial infection (D). All of these complications can be avoided with proper MMR vaccination. Side effects of vaccination (fever, injection site rash, and rarely febrile seizure and thrombocytopenia) are minimal considering the risk of complications with measles infection.
Koplik spots emerge 1 to 2 days before the characteristic erythematous maculopapular rash. They first appear as 1- to 3-mm blue papules with gray-white centers on the buccal mucosa and are pathognomonic for measles infection.
▪ Pathognomonic for measles infection
▪ Appear as 1- to 3-mm blue papules with gray-white centers on the buccal mucosa
▪ Precede the appearance of the maculopapular rash by 1 to 2 days
17. A 43-year-old man presents with complaints of lesions around his eyes. He notes that the lesions have been present for a couple of years and have not changed in size, shape, or color. You note that the lesions are 1 mm, raised and non-fluid–filled. What primary skin lesion does this patient have?
18. A 10-year-old girl with no significant past medical history is brought to her pediatrician due to several itchy lesions on her abdomen and buttocks. She notes that they have been present for the past couple of months and seem to appear and resolve in different spots. She denies any recent travel or sick contacts but does note that she has a cat who sleeps with her at night. On physical exam, the lesions are 4 mm, raised, erythematous and non-fluid–filled. How would you characterize this patient’s primary skin lesion?
17. The answer is B: Papule. This patient has a papule (B) because it is raised, solid, and less than 5 mm. Macules (A) are flat lesions less than 10 mm in diameter. A patch (C) is a larger nonpalpable lesion greater than 10 mm. Plaques (D) are elevated plateau-like palpable lesions greater than 1 cm. Nodules (E) are morphologically similar to papules, but they are greater than 1 cm in both width and depth. They are most frequently centered in the dermis or subcutaneous fat.
18. The answer is E: Papule. This patient presents with several pruritic, erythematous papules (E) likely secondary to flea bites from her cat. A papule is a solid, elevated lesion less than 5 mm in which a significant portion projects above the plane of the surrounding skin. A macule (A) is any flat lesion of less than 10 mm in diameter that is even with the surface of surrounding skin and differs in color from the surrounding skin or mucous membrane. Patches (B) are larger, flat nonpalpable lesions measuring greater than 10 mm in size. Plaques (C) are elevated palpable lesions greater than 10 mm. A nodule (D) is a solid, round, or ellipsoidal palpable lesion with a diameter larger than 5 mm. Nodules are differentiated from papules and plaques by depth of involvement and/or substantive palpability.
A papule is a primary skin lesion defined by a palpable, solid, well-circumscribed elevation of skin measuring less than 5 mm in diameter.
▪ Palpable lesion less than 5 mm
▪ May be associated with secondary features such as crusts or scales
19. A 50-year-old man with a history of atopic dermatitis presents to the clinic with golden-crusted, erythematous, weeping lesions on his left arm. He is afebrile and otherwise healthy. Gram stain of the fluid reveals gram-positive cocci in chains, and culture of the weeping area grows group A streptococci after 24 hours. What is the next appropriate step in the clinical management of this patient?
A. IV penicillin and vancomycin
B. Warm compresses and IV penicillin
C. Second generation cephalosporin
D. Topical mupirocin ointment after removal of dirt, crusts, and debris with soap and water
E. Prophylactic ampicillin for all close contacts
20. A 17-year-old woman presents to the clinic with 3 days of a perioral, crusty, yellow rash. She says that crusting started at a crack at the corner of her mouth and gradually grew to her chin. On exam a honey-crusted rash is noted at the chin and corners of the mouth with some small unruptured vesicles on erythematous bases. A clinical diagnosis of impetigo is made. Which of the following is/are true regarding this condition?
A. Highly contagious, capable of self-inoculation
B. Can start at site of skin injury or on intact skin
C. Represents an infection with S. aureus and/or group A streptococcus
D. Treatment is topical mupirocin ointment
19. The answer is D: Topical mupirocin ointment after removal of dirt, crusts, and debris with soap and water. This patient has impetigo caused by group A streptococci based on clinical findings and confirmed with Gram stain and culture. Impetigo is a superficial skin infection that very rarely has systemic effects and can be effectively treated with either topical mupirocin ointment or oral penicillin (D). Removal of crusts and debris with soap and water is a helpful adjunct. Impetigo is a very contagious, autoinoculable infection. Clinical differentiation between streptococcal and staphylococcal lesions is difficult, and older erosions may contain both types of bacteria. IV antibiotics and prophylaxis of close contacts are not warranted.
20. The answer is E: All of the above. This patient has nonbullous impetigo, which is diagnosed clinically as small vesicles on a red base. As vesicles rupture, an adherent yellow-brown, honey-colored crust forms. Locally additional sites of clustered vesicles will appear as this dermal staphylococcal and/or group A streptococcal infection grows. Areas of skin around the mouth and nose are usual sites. Although not necessary, skin injury as well as preexisting lesions such as eczema or a cold sore can lead to impetigo with the introduction of infectious bacteria. Impetigo is highly contagious and most prominent in younger children. Treatment of this local superficial infection involves isolation and avoidance of physical contact and topical mupirocin ointment (E). Systemic antibiotics should be used only for extensive cases of impetigo.
Impetigo is caused by skin infection with either streptococci or staphylococci and appears as crusted superficial erosions that contain purulent material and rupture easily. The lesions may appear as macules, vesicles, bullae, pustules, and honey-colored gummy crusts. Impetigo is a highly contagious infection and inpiduals can often autoinoculate themselves. The face and other exposed areas are most commonly affected. Gram stain and culture confirm the diagnosis.
▪ Preexisting lesions like scabies, zoster, or eczema can predispose patients to the infection.
▪ Gram stain and culture confirm the diagnosis.
21. A 42-year-old African American man presents to the office for a routine checkup. On examination, he has darkened skin on the back of his neck (shown above), axilla, and elbows, which he states has been there for a few months. He is mildly overweight, but otherwise he has no significant past medical history and presents with no other medical complaints. What is the best next step in this patient’s ongoing therapy?
C. CA 125, CEA, and CA 19-9 tumor markers for underlying neoplasm
D. CAT scan of the abdomen and pelvis
E. Reassurance with no further workup
22. A 65-year-old African American man states that multiple areas of his skin have suddenly become darker. He also complains of intermittent epigastric pain and an inability to finish his meals over the last few weeks. He says he “feels full” with minimal food intake and notes that his clothes seem looser. His fasting glucose and hemoglobin A1c are normal. What is the next best step?
D. Recommend diet and exercise
E. Reassurance with no further workup
21. The answer is B: Fasting glucose level. This patient’s findings represent the classic presentation for acanthosis nigricans, which consists of hyperkeratosis and hyperpigmentation of the neck, axilla, groin, and other skin folds, especially on flexural surfaces. This condition is most commonly associated with type 2 diabetes mellitus and insulin resistance. Therefore the best initial course of action to take with this patient is to obtain a fasting glucose level (B). Although acanthosis nigricans has also been seen in patients with adenocarcinomas of the gastrointestinal (GI) and genitourinary tract (C, D), especially gastric carcinomas, this is not the most likely etiology of the condition. Typically cases associated with carcinomas have a rapid onset, and the patient in this case has an insidious onset of the disorder. A skin biopsy (A) will show typical dermatopathology findings of hyperkeratosis, epidermal papillomatosis, slight acanthosis, and possible increased melanin pigmentation, but it will not provide diagnostic value in revealing the underlying disorder. Choice E is incorrect because a diabetes workup is indicated in patients who present with this clinical finding.
22. The answer is B: Upper endoscopy. Acanthosis nigricans with rapid onset raises suspicion for malignancy, most commonly gastric carcinoma. Although malignancy is a rare cause of acanthosis nigricans, rapid onset of skin changes, coupled with the patient’s symptoms of abdominal pain, early satiety, and weight loss, warrant investigation for gastric cancer with upper endoscopy (B). Acanthosis nigricans lesions secondary to insulin resistance (the most common cause) and malignancy are indistinguishable, so skin biopsy (C) will not help to identify the underlying cause. A topical medication to improve the cosmetic appearance of the acanthosis nigricans (A) and initiation of a diet and exercise program (D) may be appropriate if serious causes of acanthosis nigricans are ruled out; however, the patient’s symptoms plus the rapid onset of the acanthosis nigricans makes these choices, as well as reassurance (E), inappropriate at this time.
Acanthosis nigricans is a cutaneous marker commonly associated with insulin resistance and less frequently with genetic disorders or malignancy. It is characterized by symmetric, hyperpigmented plaques that typically appear on skin folds, especially the flexural areas.
23. A 4-year-old girl presents with a red-purple, raised vascular plaque over her left fourth digit. The lesion appeared a couple weeks after she was born. It grew rapidly for a period of time, but has been stable for about a year. What is the next step in treatment?
A. Surgical excision and biopsy
24. A first-time mother brings her 1-month-old infant to her pediatrician concerned by a growing plaque on her left buttock. Her mom comments that there was a red mark present at birth but is concerned that this mark has not resolved and has in fact continued to grow and now demonstrates a raised, vascular appearance. Which of the following is the best advice for this concerned mother?
B. Reassurance that most of these lesions resolve spontaneously
C. Biopsy of the lesion to rule out a malignant vascular neoplasm
D. Reassurance that while this lesion will likely be permanent it is not malignant in nature
E. Advise the use of topical corticosteroids to speed resolution.
23. The answer is E: No treatment. This lesion is a strawberry hemangioma (also called an infantile hemangioma or a capillary hemangioma). The best treatment for these lesions is to let them resolve spontaneously (E). About 60% resolve by age 5, and 90% are gone by age 9. Treatment is only necessary if the lesion blocks vision, is in the way of the nostrils, or if ulceration occurs. If surgery is necessary, laser surgery (B) or cryosurgery (C) may be indicated. Surgical excision and biopsy (A) is not indicated in this case as the diagnosis can be made clinically. Systemic glucocorticoids (D) may be initiated if treatment is indicated, but spontaneous resolution generally gives the best results.
24. The answer is B: Reassurance that most of these lesions resolve spontaneously. This lesion is most likely a strawberry hemangioma and will resolve spontaneously (B). Biopsy (C) or treatment (D) is not necessary, and clinical diagnosis is usually sufficient. Topical corticosteroids have not been demonstrated to be beneficial (E), and referral to a dermatologist is not indicated at this time.
Strawberry hemangiomas (also called capillary hemangiomas or infantile hemangiomas) are superficial vascular tumors which appear as raised, red, lumpy areas of flesh anywhere on the body, although the majority occur on the head or neck. These hemangiomas are clonal proliferations of endothelial cells. They usually appear about 1-4 weeks after birth and may grow rapidly before stopping and then slowly fading. About 60% resolve by age 5, and about 90% are gone by age 9. Women are more often affected than males. The incidence is increased in preterm infants. No treatment is necessary unless the lesion blocks vision or is in the way of the nostrils.
▪ Rapid growth phase followed by spontaneous involution
▪ Increased incidence in women and in preterm infants
▪ Intervention necessary if ulceration occurs or if the lesion causes functional impairment
25. A 40-year-old man comes to the clinic complaining of pain at the base of his right great toe, which has been going on since he woke up. He has pain while ambulating and had trouble putting on his shoes. He has hypertension controlled on hydrochlorothiazide (HCTZ) and lisinopril and takes atorvastatin for hyperlipidemia. He drinks 1-2 beers each night after dinner. On examination he has a BMI of 30 and stable vital signs. He has swelling and erythema at the base of the right hallux, and he pulls his foot away briskly in pain when this area is palpated. Needle aspiration of the area is performed, and blood work is drawn for serum uric acid. What change(s) may be helpful in this patient to prevent future gouty attacks?
B. Cessation of alcohol consumption
C. Discontinuation of the diuretic
26. A 70-year-old African American woman presents to clinic with a painful bump on her finger. Her past medical history is significant for alcohol abuse. On exam there is an inflamed Heberden node on her right first distal interphalangeal (DIP) joint that is extremely tender to palpation. Labs reveal elevated erythrocyte sedimentation rate (ESR) and elevated uric acid levels. Aspirate from the nodule demonstrates negatively birefringent needle-shaped crystals and a white blood count (WBC) of 12,000 × 103/μL. A diagnosis of acute gouty attack is made. What is/are an appropriate treatment(s) of gout?
B. Cessation of alcohol consumption
C. Nonsteroidal antiinflammatory drug (NSAID)
25. The answer is E: All of the above. This patient is suffering from acute gouty arthritis. The most commonly affected location is the first metatarsophalangeal joint, and treatment of an acute attack is aimed at analgesia and antiinflammatory measures. Needle aspiration of synovial fluid from the affected joint will help to rule out other causes (e.g., septic arthritis) and show the characteristic monosodium urate crystals on compensated polarized light microscopy. The crystals are needle-shaped and appear yellow when parallel to the axis of rotation of the compensator and blue when perpendicular. While allopurinol therapy in the intercritical period between attacks may lessen morbidity from gout, issues like obesity, hyperlipidemia, diabetes, alcoholism, smoking, and hydration take priority. Lifestyle changes can have a positive effect on a patient’s prognosis after the first attack (E), because all these factors affect purine and/or uric acid metabolism in the body.
26. The answer is E: All of the above. This patient is suffering from an acute tophaceous gouty arthritis. First-line treatment includes NSAIDs (indomethacin, naproxen). Intraarticular steroid injections can offer more immediate relief and have no systemic side effects. Colchicine can decrease inflammation if used early in a gouty attack. Both allopurinol and cessation of alcohol are effective as long-term therapies in patients with hyperuricemia and recurrent gouty attacks (E).
Gout is characterized by a group of heterogeneous conditions that result in the deposition of monosodium urate crystals in the synovial fluid, usually with associated hyperuricemia. It is typically characterized by four stages: asymptomatic hyperuricemia, acute gouty arthritis, intercritical gout (between attacks), and chronic tophaceous gout. Leukocytosis and elevated ESR are often present during acute attacks. Treatment revolves around analgesia and reduction in inflammation in the acute setting with NSAIDs, colchicine, and corticosteroids. Chronic treatment includes xanthine oxidase inhibitors like allopurinol.
▪ Affected joints are erythematous and extremely tender to palpation.
27. A 45-year-old man presents with symmetric lesions over his knees. The lesions appear as a silvery scale on an erythematous base. The man reports that he is otherwise healthy. You note that slight scratching of the scaly lesions results in punctate bleeding points. What is the most likely cause of these lesions?
28. A 38-year-old man presents complaining of a rash on his leg and chronic pain in his fingers and lower back for the past 6 months. He has no significant medical history but does note that his father suffered from something similar. On physical exam you note lesions with a silvery scale on an erythematous base throughout the patient’s left leg and with passive motion of the DIP joints of his right hand as well as mild tenderness to palpation at the sacroiliac joint. You also identify that the patient has pitting on the nails of his fingers. What would be the next best step in diagnosing this patient’s disease?
A. Skin biopsy of lesions on leg
C. No further tests, the diagnosis can be made solely on clinical findings
D. Check for human leukocyte antigen B27 (HLA-B27)
E. Check uric acid level in urine
27. The answer is E: Psoriasis. Psoriatic lesions typically occur on extensor surfaces and often exhibit Koebner phenomenon and Auspitz sign (slight scratching of the scaly lesions results in punctate bleeding points). Although bony prominences may be damaged during trauma (A), a description of a silver scale on an erythematous base is a classic description of psoriasis. Lichen simplex chronicus (B) occurs due to habitually scratching an area of skin. The skin eventually thickens and darkens. These changes are called lichenification. Seborrheic dermatitis (C) causes red or golden scaly patches of skin around areas with oily skin, such as the ears, eyebrows, scalp, and nasolabial fold. Atopic dermatitis (D) typically affects flexor surfaces and can lead to lichenification.
28. The answer is C: No further tests, the diagnosis can be made solely on clinical findings. This patient has the signs and symptoms of psoriatic arthritis, an inflammatory arthritis that characteristically occurs in inpiduals with psoriasis. A diagnosis can be made based on clinical findings (C) of psoriasis and arthropathy along with nail changes ranging from pitting, horizontal ridging, onycholysis, yellowish discoloration, or dystrophic hyperkeratosis. A skin biopsy (A) may be helpful if one is unsure of the psoriasis on this patient’s leg. However, it would not help to characterize his arthropathy. An MRI of the lumbar spine (B) may show nonspecific changes that would not be useful for a diagnosis. Although HLA-B27 (D) is found in 50%-70% of patients with axial disease, it would not be useful to rule out psoriatic arthritis in this case. Uric acid (E) levels may be elevated in the presence of extensive psoriasis. However, this is a nonspecific finding and would not help diagnosis this patient’s disease.
Psoriasis is a common chronic skin disorder typically characterized by inflamed, edematous skin lesions covered with a silvery white scale. Plaque psoriasis is the most common type and is characterized by symmetric patches on the scalp, trunk, and limbs. The most common sites are the extensor surfaces of the limbs. Guttate psoriasis is characterized by small red dots and frequently appears after an upper respiratory infection. Nail psoriasis may cause pits in the nails, which may become yellow and thickened, eventually separating from the nail bed. Psoriatic arthritis affects approximately 10% of those with skin symptoms. The arthritis is usually in the hands, feet, and larger joints. It produces stiffness, pain, and progressive joint damage. Psoriatic lesions may demonstrate Auspitz sign (slight scratching of the scaly lesions revealing punctate bleeding points) or Koebner phenomenon (lesions occurring in areas of irritation/scratching, such as the pant line). The diagnosis is usually clinical. If there is a questionable diagnosis, a punch biopsy may be performed. Treatment options include PUVA, topical retinoids, and cytotoxic agents such as methotrexate and cyclosporine.
▪ Silver scales on an erythematous base
▪ Abnormal T lymphocyte function
29. A 65-year-old man presents with a thick dome-shaped lesion on his scalp. The lesion is blue-black, 7 mm in size, and he noted that the lesion sometimes bleeds when he irritates the area. What is the most likely diagnosis?
30. A 40-year-old man presents with a black, raised lesion on his upper back. The patient noticed that the lesion has almost doubled in size over the past 6 months. On physical exam the lesion is 1 cm, nontender, and asymmetric with irregular borders. What is the correct way to characterize this lesion?
B. Superficial spreading melanoma
29. The answer is D: Melanoma. This patient has findings of melanoma (D) as indicated by the size, color, border, and asymmetry. The lesion’s characteristics are concerning for a malignant process rather than a benign nevi (A). Basal cell carcinoma (B) is the most common skin cancer. They are often slowly growing, raised papular lesions that rarely metastasize. Basal cell carcinomas may be translucent or pearly with rolled borders or telangiectasia. Squamous cell carcinoma (C) is the second most common skin cancer and usually occurs in sun-exposed areas. It is characterized by red, scaly skin that may ulcerate. Actinic keratosis (E) is a rough, scaly, dark brown or pink patch that appears after years of sun exposure. A small number of actinic keratoses eventually develop into squamous cell carcinomas.
30. The answer is A: Nodular melanoma. This lesion is a nodular melanoma (A), the second most common melanoma subtype, accounting for 15%-30% of all melanomas. Nodular melanomas are remarkable for rapid evolution, often arising over several weeks to months, and typically appear as uniformly dark black-blue lesions with irregular borders and measuring over 6 mm in size. Superficial spreading melanomas (B) are the most common subtype and account for around 70% of all cutaneous melanomas. Classically, these subtypes appear with asymmetry, irregular scalloped borders, and often various shades of color. They do not project prominently from the skin and are often nonpalpable. Lentigo maligna (C) displays asymmetry, poorly defined irregular borders, and is generally a flat, slowly enlarging, brown, freckle-like macule. Acral lentiginous melanoma (D) only constitutes 2%-8% of all melanomas in Caucasians but up to 60%-72% in African Americans. The most common sites are the sole, palm, and subungual locations, and lesions can appear brown, black, tan, or red. Actinic keratosis (E) occurs in fair-skinned older inpiduals with extensive sun exposure. These lesions are typically 2-6 mm in size and appear as erythematous, flat, rough, or scaly papules.
Melanoma is a malignant tumor of melanocytes found predominantly in the skin. It is less common than many other types of skin cancer, but accounts for 75% of skin cancer–related deaths. There are four main types of melanomas. Superficial spreading melanomas are the most common and are usually flat and irregular in shape and color. Nodular melanomas usually start as a raised area. Lentigo maligna melanomas usually occur in the elderly on sun-damaged areas such as the face, neck, and arms. Acral lentiginous melanomas usually occur on the palms, soles, or under the nails and are more common in African Americans.
▪ Border of lesion is irregular
▪ Color: melanomas usually have multiple colors
▪ Diameter: moles greater than 6 mm are more likely to be melanomas
▪ Enlarging: enlarging or evolving
31. A 43-year-old man presents with a well-demarcated, rough, slightly raised lesion on his finger. The lesion has been present for about 3 months. What is the cause of this lesion?
32. A 24-year-old man comes to your office complaining of an uncomfortable bump on his index finger (shown above). This lesion has been present for the past 2 years despite many attempts at home removal. The lesion is rough, slightly raised, and has a cauliflower-like appearance upon closer inspection. Which of the following is the most appropriate treatment for this patient’s condition?
C. Soak lesion in hot water for 10-30 minutes
D. Carbon dioxide laser therapy
31. The answer is A: Virus. This man has a lesion consistent with a verrucae, or wart. Warts are caused by the human papillomavirus (HPV) (A). They are classified based on their shape and the area of the body affected. There are several strains of HPV. Verrucae are not a fungal (B) or bacterial (C) infection. They are not caused by cellular overgrowth (D) or necrosis (E). Common warts often disappear on their own in a few months but may last years and may also recur. Treatment options include cryotherapy or salicylic acid.
32. The answer is A: Cryotherapy. The lesion on this patient’s finger is most likely a verrucae or wart due to a viral infection with human papillomavirus. The most appropriate treatment listed is cryotherapy (A). Surgical excision is rarely necessary (B). Soaking the lesion in hot water for 10-30 minutes daily for 6 weeks may aid in resolution, but a one-time soak (C) is unlikely to be beneficial. Carbon dioxide laser therapy (D) and photodynamic therapy (E) should be reserved for lesions that fail initial cryotherapy or salicylic acid treatment.
Verrucae, also called warts, are well-demarcated, rough, hard nodules or plaques with an irregular surface caused by the HPV. They typically disappear after a few months but can last years and can recur. Warts are classified based on their shape and the area of the body affected. Common warts are raised and rough and are most common on the hands. Other types of warts include flat warts, filiform warts, plantar warts, genital warts, or periungual warts. Cryotherapy or salicylic acid can also be used to remove the lesion.
▪ Treated with cryotherapy or salicylic acid
33. A 27-year-old man presents to the clinic complaining of a severely pruritic rash that recently erupted on his skin. He has never experienced a similar rash and appears anxious for symptomatic relief. He denies any GI complaints and has no significant past medical history. Physical examination reveals erythematous patches and plaques with crusts and erosions in a symmetric pattern on his elbows, knees, dorsa of the hands, upper back, and gluteal crease. A biopsy of one of the lesions shows subepidermal vesicles at the tips of dermal papillae with intravesicular neutrophil collections. Immunofluorescent staining of a biopsy from normal-appearing skin reveals granular IgA deposits. Which of the following statements regarding this patient’s diagnosis is/are true?
A. The rash will respond rapidly to dapsone.
B. This patient is at increased risk for developing GI lymphoma.
C. Strict adherence to a gluten-free diet helps to decrease exacerbations and resolve the rash.
34. A 32-year-old woman presents to your office with a 1-year history of a pruritic rash on her back and extensor surfaces of both arms and legs. Her past medical history is significant for iron-deficiency anemia and chronic steatorrhea causing a 30-pound weight loss over the past year. Physical exam is significant for pale conjunctivae and small groups of vesicles with crusting on erythematous plaques present symmetrically on her back, buttocks, and extensor surfaces. A biopsy from healthy skin around the lesions shows IgA deposits at the dermal-epidermal junction, confirming a diagnosis of dermatitis herpetiformis (DH). Blood tests are positive for antiendomysial and antitissue transglutaminase antibodies, and biopsy of the small bowel shows atrophic villi and intraepithelial lymphocytosis, confirming associated celiac disease. In the treatment of this patient, which of the following has been shown to decrease the symptoms of both autoimmune disorders long term?
33. The answer is D: All of the above. This patient is experiencing DH, which presents as an intensely pruritic, chronic papulovesicular eruption symmetrically on the extensor surfaces. While these patients have a gluten-sensitive enteropathy, fewer than 10% are symptomatic. This enteropathy, however, places them at higher risk for developing GI lymphoma. The rash responds rapidly to sulfa drugs, especially dapsone, and to a gluten-free diet, which must be maintained to prevent cutaneous disease. Thus all answer options are true (D). A biopsy from normal appearing skin that shows granular IgA deposits is diagnostic. Dapsone use may be limited by dose-related hemolytic anemia and idiopathic neuropathy.
34. The answer is C: Gluten-free diet. This patient exhibits symptoms of malabsorption (iron-deficiency anemia, steatorrhea, and weight loss). Because DH is unique to gluten-sensitive enteropathy, celiac disease is the most likely and proven cause of this malabsorption. In treating this patient, she should be tested and treated for deficiencies of fat-soluble vitamins (A, D, E, K), calcium, folate, iron, and vitamin B12. She should also be evaluated for osteoporosis. Dapsone and other sulfa drugs (sulphapyridine) are used for immediate relief and control of DH. Additional therapies for DH include tetracycline and prednisone. However, initiation and maintenance of a gluten-free diet is the long-term therapy for both DH and celiac disease (C). In celiac disease, symptom relief may take days to weeks, and histologic recovery may take months to years on a gluten-free diet. After 6 months of strict gluten- and gliadin-free diet, sulfa drugs may be dose-decreased or discontinued in treatment of DH.
Dermatitis herpetiformis (DH) is a chronic, severely pruritic, papulovesicular eruption that usually follows a symmetric distribution over the extensor surfaces. Histologically, it consists of dermal papillary collections of neutrophils, termed microabscesses. Almost all patients with DH have an associated gluten-sensitive enteropathy. It may present at any age and persists indefinitely, with varying severity if the underlying gluten sensitivity is not treated.
▪ Histologically characterized by papillary neutrophil collections
▪ Granular IgA deposits in paralesional or normal-appearing skin are diagnostic.
▪ Rash responds rapidly to dapsone and adherence to a gluten-free diet.
35. An 82-year-old man is brought from a nursing home to your office by his daughter, who is visiting from out of town and became concerned about bleeding from a lump on her father’s nose. The patient’s memory is poor, and he cannot give a complete history, saying only, “I guess I just never noticed it.” He has no complaints, and his past medical history is significant only for Alzheimer’s dementia. Physical examination reveals a pearly papule on the nose that has a waxy appearance, central crater with scab, and visible telangiectasia. Multiple actinic keratoses are seen on the face and hands. What is the next appropriate step in this patient’s management?
B. Referral for immediate irradiation
C. Whole body PET scan for staging purposes
D. Three cycles of curettage and electrodesiccation
E. Topical chemotherapy to shrink the lesion before surgical removal
36. A 75-year-old retired fisherman comes in for a routine physical. He points out a spot on his chest that has been present for more than a year. He says it occasionally bleeds and is about the same size as when he first noticed it. The lesion has an ulcerated base covered with a crust. Biopsy reveals atypical basal cells with palisading nuclei. Which of the following is the most likely diagnosis?
35. The answer is A: Shave or punch biopsy. This patient has basal cell carcinoma. The nodular type, has a characteristic translucent, waxy, or pearly appearance. A shave or punch biopsy is required to confirm the diagnosis (A). The lesion can then be treated with excision, curettage, electrodesiccation, or Mohs micrographic surgery. Curettage and electrodesiccation may be curative but leave a broad scar; therefore, these methods should not be used for basal cell carcinoma on the head and neck (D). Mohs micrographic surgery is tissue sparing and has the highest cure rate among treatment options. Irradiation may be considered for older patients (> 65 years), but recurrent lesions are aggressive and difficult to treat. Because up to half of patients will develop a second lesion, they should be monitored closely for new or recurrent lesions. Basal cell carcinoma rarely metastatasizes so treatment is local excision. Therefore PET scan for staging purposes, irradiation, and/or chemotherapy, are not part of the workup and treatment (B, C, E).
36. The answer is C: Basal cell carcinoma. The patient has an ulcerating basal cell carcinoma (C). It is common with this type of basal cell carcinoma for the ulcer to be covered with a crust. As with the nodular type, ulcerating basal cell carcinoma lesions are typically translucent and pearly, with peripheral telangiectasia. Basal cell carcinoma is slow growing, with virtually no metastatic potential. Atypical basal cells with palisading nuclei are found on biopsy. Squamous cell carcinoma (A) can also ulcerate and crust, but biopsy shows atypical keratinocytes and malignant epidermal cells penetrating the basement membrane. Melanoma (B) can also ulcerate, but the lesion in this case is slow growing and shows characteristics of basal cell carcinoma on biopsy. Seborrheic keratosis (D) presents as waxy brown papules and plaques, which have a “stuck-on” appearance. Actinic keratoses (E) are light, scaly, erythematous lesions. They are a precursor to squamous cell carcinoma.
Basal cell carcinoma is the most common skin cancer. It has a characteristic translucent, waxy, or pearly appearance. As the lesion enlarges, it often develops an umbilicated or ulcerated center and peripheral telangiectasia.
▪ Major risk factor: chronic sunlight exposure
▪ Tumor is slow growing and locally invasive, aggressive, and destructive
▪ Metastasis is extremely rare.
▪ Diagnose clinically; confirm with biopsy
▪ Treat with excision, curettage, electrodesiccation, or Mohs micrographic surgery
37. A 17-year-old man presents with lesions over his thighs, buttocks, and arms. The lesions appear to have a small raised central white area with an erythematous base and contain necrotic inflammatory cells. How would you describe this patient’s lesions?
38. A 4-year-old girl presents to her primary care physician with several itchy lesions over her torso, face, and buttocks. These lesions began 2 days ago. Her mother notes that she is enrolled in daycare where several other children also experienced similar lesions. On physical exam the lesions are 3-5 mm in size and appear as circumscribed, raised lesions with a central whitish, pus-filled area. How would you classify this patient’s lesion type?
37. The answer is A: Pustule. This patient has pustules (A) due to folliculitis. Pustules are small raised lesions filled with cloudy, purulent material (necrotic inflammatory cells). Vesicles (B) are circumscribed fluid-containing epidermal elevations measuring less than 1 cm, commonly referred to as blisters. Bullae (C) are large vesicles and are greater than 1 cm. Nodules (D) are greater than 1 cm and are centered in the dermis or subcutaneous fat. Cysts (E) are cavities with a closed sac that contain a liquid, semisolid, or solid material.
38. The answer is B: Pustule. This patient has pustules (B) likely secondary to a varicella infection. Pustules are small raised lesions filled with cloudy, purulent material (necrotic inflammatory cells). Papules (A) are solid, elevated lesions measuring less than 0.5 cm in which a significant portion projects above the plane of the surrounding skin. Nodules (C) are greater than 1 cm and are centered in the dermis or subcutaneous fat. Macules (D) are flat lesions of less than 10 mm in diameter that are even with the surface of surrounding skin and differ in color from the surrounding skin or mucous membrane. Bullae (E) are large vesicles greater than 1 cm.
A pustule is a small elevation of the skin containing cloudy or purulent material usually consisting of necrotic inflammatory cells or exudate.
▪ Contains pus (necrotic inflammatory cells)
▪ May or may not be related to hair follicles
39. A 29-year-old African American woman complains about a growth on the posterior aspect of her earlobe during an office visit. It appeared where she received a second ear piercing during her pregnancy last year and continued to grow even after she removed the earring. She is requesting that it be removed. What are her treatment options?
D. Wide-margin excision with a skin flap
E. Biopsy to confirm diagnosis
40. A 25-year-old African American patient presents to the clinic with multiple growths that appeared on her skin after local injures: pimples, scratches, cuts, and tattoos. She admits that her mother and sister have similar growths. She is anxious to have them removed. On exam there are multiple raised nodules with rounded, well-defined borders on her right shoulder and chest. Upon palpation they are slightly tender and have a rubber-like texture. Which of the following is/are true regarding her diagnosis?
A. Excision has a high risk of keloid recurrence.
B. Hispanic and African American populations have a higher rate of keloid occurrence.
C. Injections of corticosteroids and cryosurgery can diminish keloids.
D. The key to prevention is avoidance of any disruption of the skin.
39. The answer is A: Cryosurgery. This patient has keloid formation at the site of her ear piercing. It is not uncommon for keloids to develop during pregnancy. Keloids are more common in dark-skinned races and represent excessive and dysregulated collagen deposition at the site of injury. Simple surgical treatment is often very difficult because keloids tend to recur and may get worse. Injections of glucocorticoids have shown some promise in shrinking lesions and relieving symptoms. Cryosurgery with repeated freezing over the course of a month has produced flattening of many lesions, but it is not always successful (A). Biopsy should not be performed, because it can exacerbate the keloid formation.
40. The answer is E: All of the above. Keloids are benign overgrowths of connective tissue arising from sites of dermal injury. They grow well beyond the dermal borders of injury, as opposed to a hypertrophic scar which remains within the borders of normal skin, and can be expected to grow over time. Because they are generated from trauma to the skin, keloid excision can lead to recurrence. Although periodic injections of triamcinolone and cryotherapy have both been used to diminish keloid size, ridding a patient of keloids is inherently difficult. Prevention is the key and educating patients about avoiding cosmetic or elective procedures such as piercings, tattoos, and plastic surgery is important. Darkly-pigmented populations have a higher incidence of keloids. Keloid proneness can also have a recessive or dominant pattern of familial inheritance (E).
A keloid results from the uncontrolled synthesis and excessive deposition of collagen at sites of previous dermal injury and wound repair. They can occur after local skin trauma or inflammatory skin reactions. A keloid extends beyond the border of the original wound and resembles a well-circumscribed pink to purple nodule or pseudotumor. It does not regress spontaneously.
▪ Dysregulated collagen deposition at site of dermal injury
▪ Tend to recur after excision; difficult to treat
▪ Predilection for areas of increased tension
▪ More common in Asians and dark-skinned peoples
41. A 12-week-old infant is brought to the pediatrician with multiple yellow, greasy, flaky lesions over his scalp, especially along his hairline. His mother has tried several home remedies, but nothing has seemed to help. What therapy would you recommend?
42. A 43-year-old woman with a history of AIDS presents with dandruff and erythema and scaling of her eyebrows and nasolabial folds. You suspect seborrheic dermatitis. Which of the following treatments should be avoided in treating the facial scaling?
E. High-potency topical corticosteroids
41. The answer is A: Selenium sulfide shampoo. This infant has classic findings of seborrheic dermatitis, thought to be caused by overgrowth of the yeast, Malassezia furfur. Seborrheic dermatitis on the scalp responds to shampoos, such as selenium sulfide (A). Topical antifungals, such as ketoconazole (D), can be tried when the lesions are in other sebum-rich areas, but shampoos are used when lesions are present on the scalp. Topical nystatin (C) is often used to treat candida infections. Oral fluconazole (B) and other oral medications can be tried for refractive disease, but would not be the first-line choice, especially in a 12-week-old infant. Moisturizing lotion (E) will not provide any relief, because the affected areas are not caused by breaks in the skin due to dryness.
42. The answer is E: High-potency topical corticosteroids. Antidandruff shampoo (A), salicylic acid (B), ketoconazole (C) and hydrocortisone cream (D) are all appropriate options for treating seborrheic dermatitis. The use of higher potency topical corticosteroids (E) should be avoided on the face, as they can lead to steroid rosacea or perioral dermatitis.
Seborrheic dermatitis, sometimes referred to as cradle cap when it occurs during infancy, is a skin disorder that can affect the scalp, face, or trunk. Skin appears greasy, yellow-red, flaky, and scaly. Seborrheic dermatitis particularly affects the sebum gland–rich areas of skin. The yeast, Malassezia furfur, is involved. Temporary hair loss may be a side effect to the inflammatory process. Topical treatments such as shampoos and creams are used in treatment.
▪ Greasy, yellow-red, flaky, scaly
▪ Affects sebum-rich areas of skin
▪ Antifungals, such as ketoconazole, may be helpful in treatment.
▪ Outbreaks are usually worse in the winter and can be worsened by stress or fatigue.
43. A 34-year-old man comes to the clinic to follow up on his antiretroviral therapy (ART). Six months ago, his CD4+ count was > 500/μL and viral load was < 10,000 copies of human immunodeficiency virus (HIV) RNA/mL. He has no complaints, but a new white, corrugated plaque is noted on the lateral aspect of his tongue on physical examination. It does not scrape off with a tongue blade. What is the next best step in this patient’s treatment?
A. Punch biopsy and referral to otolaryngology or oral surgery for possible resection
B. Repeat CD4+ count, viral load, and perform drug-resistance testing
C. Oral fluconazole for 10-14 days
44. A 35-year-old African American man comes to clinic for his yearly physical. The patient has no complaints. He reports having had a flulike illness a few months ago. He was coughing with high fevers and chills in bed for more than 2 weeks. His social history is significant for multiple male and female sexual partners with intermittent condom use. On physical exam there is anterior and posterior cervical lymphadenopathy, as well as a 1-cm white, adherent, corrugated, nontender patch on the left anterolateral lingual margin. A clinical diagnosis of oral hairy leukoplakia (OHL) is made. The patient is positive for HIV on initial ELISA test and confirmed with a Western blot. Which of the following is/are true regarding OHL?
A. It represents a local Epstein-Barr virus (EBV) infection
B. Seen only in immunocompromised states
C. Treatment is directed at underlying condition
43. The answer is B: Repeat CD4+ count, viral load, and perform drug-resistance testing. This patient has OHL, which is a benign lesion of the oral mucosa representing EBV infection. It most often appears as an asymptomatic, corrugated white plaque on the inferolateral aspects of the tongue and does not scrape off. While the lesion itself does not need treatment, it may herald the failure of ART or the development of drug resistance. Candida coinfection can be present, but it will scrape off, as opposed to OHL. The appearance of OHL carries poor prognosis in HIV disease and demands retesting of CD4+ counts, viral load, and investigation into resistance (B).
44. The answer is E: All of the above. OHL remains an important clinical sign of underlying immunosuppression (HIV, organ transplant, extended steroid use, chemotherapy). As in this case, OHL can be the herald of HIV infection. This clinical picture prompted HIV testing. Even though patients with OHL and HIV are at higher risk of developing malignancies (lymphoma), OHL is itself a benign lesion that is rarely symptomatic. It appears on the lateral borders of the tongue as a fixed, white or gray, corrugated patch that may not be removed by scraping. EBV replicates freely within the lesion, where candida infection may coexist. The lesion will resolve with highly active antiretroviral therapy (HAART) and subsequent restoration of immunocompetence (E).
Oral hairy leukoplakia (OHL) is a benign hyperplasia of the oral mucosa that most frequently appears on the lateral or inferior aspect of the tongue. It represents EBV infection and presents as asymptomatic, corrugated white plaques with accentuation of the vertical folds. It is seen primarily in the HIV population.
▪ EBV infection in the HIV population; candida coinfection may be present
▪ Not a premalignant condition, but associated with poorer prognosis in HIV disease
45. A 67-year-old Caucasian man comes to the office for the first time. He recently moved to the area and works part time on a fishing boat. He previously worked as a landscaper and trash collector. He has no complaints, although his past medical history is significant for a skin biopsy on his shoulder “for a dark mole” 10 years ago. As he speaks, his hands are visible (shown above). Similar lesions are present on his cheeks and temples. The lesions are rough and scaly and range from 1-5 mm in diameter. What is the next best step for the lesions on his hand?
A. Reassurance with no further workup
D. Recommend UVA/UVB sunscreen with no further workup
46. A 62-year-old farmer is concerned about a rough patch on his lip. It has been there for more than a year and has not changed during this time. It is not painful. He has had similar lesions on his hands and the top of his head, some of which have been “frozen” by his dermatologist. On examination, the lesion appears well-demarcated and has an ulcerated base. What is the next best step in management?
A. Reassurance with no further workup
D. Recommend UVA/UVB sunscreen with no further workup
45. The answer is C: Cryosurgery. The patient’s history of sun exposure, combined with the appearance and description (rough and scaly) of the lesions, makes actinic keratosis the likely diagnosis. Since actinic keratosis can progress to squamous cell carcinoma, the lesions should be treated. Cryosurgery works in most cases (C). Actinic keratosis can usually be diagnosed clinically; however, highly hyperkeratotic lesions, as well as those that are painful, bleeding, ulcerated, or rapidly growing, should be biopsied to rule out malignancy (B). Sunscreen is an important preventive measure (D), but treatment is warranted at this time. Wide local excision is the treatment if squamous cell carcinoma is diagnosed (E).
46. The answer is B: Biopsy. The lesion most likely represents actinic keratosis. It is a well-demarcated, stable lesion in an exposed area on a light-skinned man who has worked extensively outdoors. However, actinic keratosis can progress to squamous cell carcinoma, and ulceration is a concerning feature. Thus biopsy is warranted (B). His history is suggestive of cryosurgery (C) for other lesions, and this may be an appropriate treatment in this case if the biopsy is negative. Sunscreen (D) should be recommended as a preventive measure but does not resolve the question of how to manage the current lesion. Because this is likely actinic keratosis, wide local excision (E) is not appropriate at this time.
Actinic keratosis consists of rough, adherent, scaly lesions that are often erythematous and painful when scratched. They result from proliferation of abnormal epidermal keratinocytes in response to prolonged UV radiation exposure.
▪ Precursor of squamous cell carcinoma
47. A 63-year-old African American woman presents with a large violaceous plaque over the bridge of her nose, her cheeks, and her upper lip. She also complains of cough and dyspnea. A chest x-ray reveals bilateral hilar adenopathy. Which of the following findings would you expect?
A. Biopsy of the skin lesion showing noncaseating granuloma
B. Biopsy of the lung showing caseating granuloma
C. Low serum angiotensin-converting enzyme (ACE) level
D. Pulmonary function test (PFT) showing obstructive pattern
E. Positive rapid plasma reagin (RPR)
48. A 34-year-old African American man presents with worsening shortness of breath, chest pain, and cough of 3 months’ duration. He also complains of fatigue and general malaise, describing a 10-pound weight loss over the last 3 months. This is the first time he has experienced symptoms like this, and he denies any history of travel or incarceration. He works as a librarian and denies alcohol, drug, or tobacco use. Physical exam reveals patchy crackles. Chest x-ray shows mediastinal adenopathy, and biopsy of one of the lesions reveals noncaseating granulomas. His HIV test is negative. Which of the following is the most appropriate initial treatment for this patient?
47. The answer is A: Biopsy of the skin lesion showing noncaseating granuloma. The violaceous plaque over this woman’s face is lupus pernio, which is a cutaneous manifestation of sarcoidosis. This woman also has bilateral hilar adenopathy, a classic finding in sarcoidosis, which indicates lung involvement. A biopsy of the lung or skin lesion would show noncaseating granulomas (A). Caseating granulomas on lung biopsy (B) are suggestive of tuberculosis (TB). Up to 75% of untreated sarcoid patients will have an elevated ACE level, thus a low serum ACE level (C) would not aid in making a diagnosis. When lung involvement is present in sarcoidosis, a restrictive pattern is seen on PFTs rather than an obstructive pattern (D). RPR (E) is a screening test for syphilis.
48. The answer is D: Glucocorticoids. This patient is suffering from sarcoidosis, a multisystem disease that most frequently involves the lungs. Other manifestations include erythema nodosum, acute polyarthritis, and anterior uveitis. Mediastinal and paratracheal adenopathy are highly suggestive of sarcoidosis. Additional classic findings on chest X-ray include reticulonodular infiltrates and biopsy will demonstrate noncaseating granulomas. Asymptomatic sarcoidosis is often followed closely without treatment due to the high rate of spontaneous remission, but patients with symptomatic disease receive systemic glucocorticoids (D) as initial treatment for sarcoidosis. INH and rifampin (A) are part of the typical four drug regimen used to treat active TB. While TB could explain many of this patient’s symptoms, biopsy would show caseating granulomas. Cyclophosphamide (C) is a chemotherapeutic agent that is often used to treat systemic lupus erythematosus with renal involvement and is not an appropriate initial treatment for sarcoidosis. Infliximab is a tumor necrosis–alpha inhibitor (TNF-alpha inhibitor) approved for the use in ankylosing spondylitis, inflammatory bowel disease, and rheumatoid arthritis. Neither infliximab nor chemotherapy (B) would be an appropriate treatment for this patient.
Sarcoidosis (Noncaseating Granulomas)
Sarcoidosis is a systemic granulomatous inflammatory disease of unknown etiology. The disease is characterized by noncaseating granulomas. Granulomas are most often noted in the lungs or lymph nodes, but almost any organ can be affected. The highest incidence is in Northern American blacks and Northern European whites. Among blacks, women are more frequently affected than men. Disease onset is usually in the 30s or 40s. Lupus pernio is a severe cutaneous manifestation of sarcoidosis. Violaceous plaques can occur on the nose, cheeks, ears, lips, and fingers. Diagnosis of sarcoidosis requires three components: clinical and radiographic manifestations, exclusion of other diseases with similar presentations, and the presence of noncaseating granulomas. Chest x-ray, pulmonary function tests, ECG, slit-lamp eye exam, liver function tests, and serum calcium test should be included in the initial evaluation of a patient with suspected sarcoidosis. Glucocorticoids are the initial treatment.
▪ Bilateral hilar adenopathy may be seen on imaging.
▪ Elevated serum ACE level in 75% of untreated patients
▪ Histopathologic detection of noncaseating granuloma is helpful to make diagnosis.
▪ Common presenting symptoms include cough, dyspnea, chest pain, eye lesions, and/or skin lesions.
49. A 23-year-old man presents with pruritic lesions on his right arm which appeared about 24 hours ago over his upper arm. The lesions appear as central rounded localized areas of edema with peripheral erythema. How would you define the central area of edema?
50. A 45-year-old woman comes to your office complaining of a raised, red, itchy lesion with a central area of edema and peripheral erythema that appeared a few hours after being bitten by a mosquito. She has a formal event tomorrow and is concerned about how long this unsightly mark will remain on her arm. What is the best advice for this patient?
A. This lesion will likely fade in 7 days.
B. This lesion will likely progress to a disseminated rash in 3-7 days.
C. This lesion will likely go away in 24-48 hours.
D. Corticosteroids are necessary for the treatment of this lesion.
E. Biopsy is warranted for definitive diagnosis.
49. The answer is B: Wheal. This patient has urticaria (hives), which typically last 24-48 hours. The lesions are pruritic and classically demonstrate a central wheal (B). The wheal is the area of localized edema. Surrounding the wheal, a flat area of erythema is often present, referred to as the flare (A). Although the lesion is similar to a vesicle (C), a small, fluid-filled, elevated lesion, the evanescent nature of the lesion and the associated pruritic description indicate urticaria. A bulla (D) is a large vesicle. A cyst (E) is an epithelial-lined sac containing fluid or semisolid material.
50. The answer is C: This lesion will likely go away in 24-48 hours. This patient is experiencing an allergic reaction from the insect bite known as a wheal and flare reaction that will likely resolve in 24-48 hours without any treatment (C). Corticosteroids are not necessary for the treatment of this lesion (D). Clinical diagnosis suffices in this case, and biopsy is not warranted unless the lesion persists (E).
A wheal is a primary skin lesion and is defined as a rounded or flat-topped, pale-red papule or plaque that is typically evanescent, disappearing within 24-48 hours. A wheal appears as an area of localized edema that follows vascular leakage. A wheal and flare skin reaction is often associated with an allergic reaction. The wheal is the central raised area, which is surrounded by a flat erythematous flare.
51. A 56-year-old woman comes to the office for a postoperative visit 1 week after open-fixation of an ankle fracture and complains of pain and swelling in her foot (pictured above). She states that she first noticed a patch of redness and some pain near the surgical incision last night but woke up to find it had spread to encompass her entire foot. She reports that she “just doesn’t feel well,” and reports chills overnight. On physical exam, her temperature is 101 ° F (38.3 ° C), blood pressure 118/78, and heart rate 86 beats per minute (bpm). The right foot is edematous, erythematous, warm, and tender to the touch with no crepitus or fluctuance present. The incision site is intact, and no purulent material is noted. Which of the following infectious organisms should be suspected in this patient?
A. Group A β-hemolytic streptococci
D. Escherichia coli and other gram-negative species
52. A 77-year-old Caucasian woman was recently bitten on the hand by her housecat. The cat has been vaccinated against rabies and never leaves the house. The woman has a history of hypertension and hyperlipidemia but is otherwise healthy. Her hand is erythematous and edematous. Strength in her fingers and wrist is 5/5. An x-ray showed no tooth fragments or bony injury. Cultures are pending. She is given tetanus toxoid in the ED. Which of the following is the best treatment?
51. The answer is E: All except B. This patient has cellulitis that she developed after a surgical procedure. The defect in the skin barrier and any metal hardware installed during the procedure are risks for developing this type of infection. She has the classic findings of edema, erythema, warmth, and pain. The lack of crepitus and fluctuance is reassuring that this infection is not necrotizing fasciitis or an abscess. Common pathogens for cellulitis include group A β-hemolytic streptococci and S. aureus species; however, this patient is also at risk for E. coli and gram-negative infection because the wound is below the waist. Thus initial antibiotic coverage should have activity against these pathogens and can be adjusted later if the pathogen(s) can be identified (E).
52. The answer is A: Amoxicillin-clavulanate. The patient has cellulitis from a cat bite and is likely infected with Pasteurella multocida. The best antibiotic choice is oral amoxicillin/clavulanic acid for 7-10 days (A). Alternatives include oral doxycycline or clindamycin plus a fluoroquinolone. Clindamycin alone and cephalosporins do not provide coverage against P. multicida (B, C, D). Cat bites often penetrate to tendons and bones. The wound should be examined for depth of injury and possible joint penetration. Nerve and tendon function and integrity of nearby vessels should be determined, and an x-ray should be obtained to exclude retained tooth fragments, fracture, and/or crush injury, which may occur in the setting of an animal bite.
Cellulitis is an acute inflammatory reaction representing a spreading infection of the dermis and subcutaneous tissue. The most common pathogens include group A β-hemolytic streptococci and S. aureus. It typically presents as a small patch of swelling, erythema, and pain before spreading diffusely. As the infection spreads, the patient may experience fever, chills, and malaise, and is at risk for developing septicemia.
▪ Edematous, expanding, erythematous, warm plaque with ill-defined borders
53. A 35-year-old man notices a slow growing mass on his arm. The mass is mildly tender, and he is concerned because the mass is large and noticeable to others. Physical examination reveals a rubbery, soft, fluctuant mass with lobulation and free mobility of the overlying skin. What is the most likely diagnosis?
54. A 50-year-old man presents to his primary care physician with a large mass on his upper back. The mass is painless and, aside from being uncomfortable due to its size, has not otherwise affected the patient. He is, however, concerned that he might have cancer because the mass has been slowly growing over the past 5 years. On physical exam the mass is superficial, nontender, homogeneous, and rubbery. Although the physician feels the mass is highly likely to be benign, a biopsy is conducted to better characterize the tissue and assure the patient. What is the most likely histological finding?
A. A mixture of mature adipocytes and a chondroid matrix containing lipoblasts.
C. Large numbers of brown fat cells mixed with mature white fat.
E. A proliferation of adipose and fibrous tissue within the epineurium infiltrating along and between nerve bundles.
53. The answer is C: Lipoma. Superficial subcutaneous lipomas are common, benign neoplasms of the skin. They rarely cause symptoms, but patients often bring them to the attention of their providers either because they are either worried about the possibility of cancer or because of the cosmetic deformity caused by larger lesions. Clinical history is used to distinguish lipoma from more serious conditions such as lymphoma (A) based on the fact that lipomas are soft, asymptomatic, and usually do not enlarge quickly. Malignant transformation of a lipoma into a liposarcoma (B) is rare. Liposarcomas typically appear in the deep fat tissue of the thigh or abdomen in people between the ages of 50 and 70. If a suspected lipoma causes symptoms, is rapidly enlarging, or is firm rather than soft, a biopsy is indicated. Glomus tumors (D) are small benign tumors that arise from the glomus body. Cutaneous leiomyomas (E) are benign soft tissue neoplasms that arise from the smooth muscle and may involve vascular smooth muscle, the dartos muscles of the genitalia, the nipples, or the areolas.
54. The answer is D: Lobules of mature white adipose tissue pided by fibrous septa containing thin-walled, capillary-sized vessels. This patient is presenting with a lipoma (D), the most common soft-tissue neoplasm. These tumors occur predominantly in inpiduals between 40 and 60 years old, but may affect patients in a wide age range. Lipomas are entirely benign mesenchymal neoplasms. The most common presentation is as a painless subcutaneous mass typically occurring on the trunk, neck, or extremities. Less commonly, lipomas may be found deep in the subcutaneous tissue or intramuscularly and may be painful to patients. Histologically these tumors are circumscribed, encapsulated by a thin, fibrous capsule, and composed of mature white adipocytes lacking evidence of nuclear atypia. Because lipomas are entirely benign, they may be left alone without concern for malignant potential unless they cause discomfort to a patient. In the instance of very large tumors or intramuscular lipomas, surgical excision is the treatment of choice. (A) Chondroid lipomas are rare benign tumors occurring most commonly in adult women and tend to be smaller than 5 cm. They are characterized histologically by an admixture of a mature adipocytic component and a chondroid matrix containing lipoblasts. (B) Pleomorphic liposarcomas are aggressive sarcomas found on the extremities of adults and are associated with high rates of metastasis and mortality. These deep-seated tumors tend to grow rapidly and are less frequently found in subcutaneous tissue. Histologically they are characterized by features of a high-grade pleomorphic sarcoma containing spindle cells and multinucleated giant cells with admixed lipoblasts. (C) Hibernomas are rare benign neoplasms containing brown fat. They most commonly affect young adults and are most frequently found in the thigh region. (E) Lipomatosis of nerve is a rare tumor that affects infants and children and presents as a growing mass, most commonly on the hand. Histologically, lesions are characterized by a proliferation of adipose and fibrous tissue within the epineurium, infiltrating along and in between nerve bundles.
A lipoma is a benign tumor of mature fat cells enclosed by a thin, fibrous capsule. They are most often found superficially in the subcutaneous tissue but can more rarely involve fascia or deeper muscular planes.
▪ Familial multiple lipomatosis is a genetic condition resulting in multiple lipomas.
▪ Diagnostic workup: CT or ultrasound (not MRI), excision, biopsy
55. A previously healthy 64-year-old man presents with localized pain, erythema, and swelling surrounding a small wound on his right hand. These symptoms rapidly progressed to involve his entire right arm, and his pain became severe. He also developed fever and diarrhea. Initial laboratory evaluation reveals an elevated WBC and an elevated creatine phosphokinase. In addition to empiric antibiotics, what would be the next step in treatment?
A. Reexamine patient in 24 hours
C. Send patient for immediate MRI
D. Culture wound on patient’s right hand
E. Surgical exploration and debridement
56. A 61-year-old man with a past medical history of type 2 diabetes mellitus, IV drug use, and chronic skin infections presents to the ED with a 3-day history of subjective fever and confusion along with swelling, redness, and blisters on his right arm. The patient admits that he had been “skin-popping” IV heroin in his right arm in the week prior to the onset of his symptoms. Physical exam reveals erythema, brawny edema, and severe pain with very minimal passive movement of the right extremity. There are several large bullae seen on his right forearm, along with crepitus in the overlying skin. What is most important first step in the management of this patient’s condition?
A. MRI of the right upper extremity
C. Transfusion of two units of packed red blood cells
D. Lance of the bullae and culture fluid
55. The answer is E: Surgical exploration and debridement. This patient is presenting with findings that are concerning for necrotizing fasciitis. This is a surgical emergency and requires exploration and debridement (E). Surgical exploration is the only way to confirm the diagnosis, and prompt surgical exploration facilitates early debridement. Broad-spectrum IV antibiotics should be administered. Reexamining the patient in 24 hours (A) is not appropriate, given the likelihood of rapid progression. Although necrotizing fasciitis must be distinguished from other processes, such as gas gangrene, pyomyositis, and myositis, the history and clinical features usually allow this distinction. Laboratory findings are not specific. Imaging may be useful in some instances. CT is most commonly used to visualize air along the fascial planes. MRI and ultrasound (B, C) may not delineate air along the fascial planes. MRI often cannot distinguish necrotizing fasciitis from cellulitis or inflammation. Gram stain and culture of the lesion (D) may be positive for organisms, but this is not as reliable as obtaining deep samples during surgical exploration. If the diagnosis of necrotizing fasciitis is suspected, awaiting the results of blood or skin cultures is not recommended.
56. The answer is B: Surgical consult. This patient presents with the classic symptoms of a necrotizing soft tissue infection, which include tissue pain out of proportion to physical examination findings, erythema, brawny edema, and crepitus. Bullae develop later in the course of the infection. This patient has several risk factors for a necrotizing soft tissue infection, including diabetes mellitus, advanced age, chronic skin infections, and IV drug abuse. Several other risk factors are alcoholism, peripheral vascular disease, heart disease, renal failure, HIV, cancer, NSAID use, decubitus ulcers, and immune system impairment. Necrotizing fasciitis is a clinical diagnosis based on physical exam findings and patient history. This patient’s past medical history, especially his IV drug use, make the diagnosis highly likely. Necrotizing soft tissue infections are a surgical emergency, and early surgical consultation (B) is the most important first step in the management of all suspected cases of necrotizing fasciitis, and the gold standard for diagnosis and therapy remains operative exploration and surgical debridement. MRI (A) is highly sensitive in identifying fascial thickening and deep tissue collections but delays definitive surgical treatment. Blood transfusion (C) may be indicated later to correct anemia from hemolysis but is not the first step in management. Although cultures of blood and bullae fluid (D) may be helpful later in the treatment when antibiotic coverage is narrowed, it is more important to get the patient into the operating room for exploration and debridement. Hyperbaric oxygen therapy (E) is a controversial therapy that would be the decision of the surgical consult and would not be part of the initial treatment of a patient in the ED.
Necrotizing fasciitis is an infection of the deep layers of skin and subcutaneous tissue that easily spreads across the fascial planes. Necrotizing fasciitis may present initially with localized pain, erythema, and swelling. However, rapid progression may follow, resulting in bullae formation and systemic symptoms. If untreated, the bacteria can travel rapidly along the fascia of the muscle and spread throughout the body, leading to sepsis and death. There are two types of necrotizing fasciitis. Type 1 is a mixed organismal infection that occurs postsurgically, often in patients with diabetes or peripheral vascular disease. Type 2 is a monomicrobial infection caused principally by group A streptococcus (Streptococcus pyogenes).
57. A 36-year-old man comes to the clinic complaining of weakness. He states he has recently noticed a lack of energy and frequently experiences backaches and headaches. He is also concerned about recent changes in his appearance. Examination reveals plethoric moon facies, supraclavicular fat pads, and a protuberant abdomen. He does not smoke or drink alcohol and takes no medications. Past medical history is significant only for cellulitis 2 months prior. Which sequence of tests would confirm the diagnosis?
A. Serum adrenocorticotropic hormone (ACTH) level and MRI of the head
B. Dexamethasone suppression test, urine free cortisol, and serum ACTH
C. CT scan of the chest and abdomen
D. Midnight serum cortisol, morning serum cortisol, and random serum cortisol tests
E. No further testing necessary
58. A 22-year-old woman comes to the clinic because she is concerned about changes in her appearance, as well as decreased libido and irregular menses, which she reports have been worsening over the past several years. She feels that her face has gotten larger, and she no longer feels attractive. She also reports that her skin has become dark spotted, and she has noticed purple lines on her abdomen. In the last few months, she has given up on physical activity because she feels weak. Examination reveals plethoric moon facies, supraclavicular fat pads, and central obesity. Her blood pressure is 150/90. She does not smoke or drink alcohol. She takes no medications. Past medical history is significant only for recurrent infections in recent years. Which of the following describe changes seen in the most likely diagnosis of this patient?
A. Increase in serum ACTH level produced by the anterior pituitary
B. Increase in cortisol level and decrease of ACTH level
C. Increase in ACTH level produced ectopically
D. Decrease in cortisol level due to adrenal insufficiency
E. Electrolyte disturbances, normal ACTH levels
57. The answer is B: Dexamethasone suppression test, urine free cortisol, and serum ACTH. This patient displays the physical and symptomatic manifestations of hypercortisolism in Cushing syndrome, and his condition warrants a workup (E). The correct sequence of confirmatory laboratory testing is a dexamethasone suppression test, urine free cortisol, and serum ACTH (B). Dexamethasone suppression testing is performed by giving 1 mg of dexamethasone orally at 11 PM and assessing serum cortisol at 8 AM the following morning. An abnormal test result warrants confirmation of excess cortisol by 24-hour urine free cortisol testing, midnight cortisol levels, or a late-night salivary cortisol assay (D). Once hypercortisolism is established, serum ACTH levels should be assessed. A level of ACTH below 20 pg/mL indicates a probable adrenal tumor, whereas higher levels are the result of a pituitary tumor (termed Cushing disease) or ectopic ACTH production. Imaging techniques for localization of the lesion are indicated once the initial workup has been completed (A, C).
58. The answer is A: Increase in serum ACTH level produced by the anterior pituitary. The patient suffers from Cushing syndrome (A), due to increased production of ACTH. She has typical signs of this disorder, including round plethoric facies, purple skin striae, and central obesity. She also has symptoms of weakness, menstrual irregularities, and sexual dysfunction. Cortisol increases secondary to an increase in ACTH, rather than a decrease (B). The patient is not a smoker, so the increased in ACTH is not likely due to ectopic production from a malignant tumor, such as small cell carcinoma of the lung (C). Addison disease causes an increase in ACTH (because of lack of negative feedback). Typically it presents as an increase in skin pigmentation but is not associated with the other symptoms seen in this case (D). Conn syndrome results in electrolyte disturbances and muscle weakness, but the other symptoms in this case are not explained by this disease (E).
Cushing syndrome refers to the state of excess corticosteroids and the resultant physical manifestations. The most frequent cause is iatrogenic. Cushing syndrome is less frequently due to endogenous excess corticosteroid production by the adrenal cortex. Cushing disease accounts for nearly 40% of cases and describes the scenario where the manifestations of excess corticosteroids result from the hypersecretion of ACTH by a benign pituitary adenoma, most frequently located in the anterior pituitary. Occasionally, hypercortisolism may represent a paraneoplastic condition where nonpituitary neoplasms like small cell lung cancer produce and secrete ACTH. Excess corticosteroid production independent of ACTH is due to autonomous secretion of cortisol by the adrenals, usually from a unilateral adrenal tumor.
▪ Women: oligomenorrhea or amenorrhea; males: impotence
▪ Psychologic changes: decreased concentration, mood liability, frank psychosis
▪ Hyperglycemia, glycosuria, leukocytosis, lymphocytopenia, hypokalemia
▪ Elevated serum cortisol and urine free cortisol; lack of normal suppression by dexamethasone
59. A 41-year-old male patient has been on long-term high-dose steroids for Crohn disease. He is concerned because he has noticed an increasing number of well-defined, symmetric, elevated, reddish-purple lesions in his axilla. He also has several older lesions which have faded to a pale color. Which of the following options may help to improve the appearance of these lesions?
C. Stop high-dose steroid treatment
60. A 28-year-old woman with a history of severe asthma presents to your office complaining of recent weight gain. She is frustrated after trying many diets and comes to you for advice. Upon further questioning, the patient also describes stretch marks on her abdomen and fatty growth on her neck and shoulders. You notice that her arms and legs are still quite thin and her face appears moonlike. She seems to be concealing her armpits which you notice to be quite sweaty. Which of the following is the best step in diagnosing her condition?
C. Fasting plasma glucose level
E. Dexamethasone suppression test
59. The answer is E: All of the above. All of the above treatments (E) are known to help improve the progression of striae (stretch marks). Although the lesions are not reversible, there are treatments that can help to fade the lesions. Topical tretinoin (A), glycolic acid creams (B), and stopping steroid treatment (C) will help to fade striae. In addition, laser surgery (D) has been shown in some cases to improve the appearance of stretch marks.
60. The answer is E. The most common cause of Cushing syndrome is the exogenous administration of corticosteroids by a health care provider, in this case to treat this patient’s severe asthma. The patient’s symptoms, central obesity, striae, and hyperhidrosis, in the setting of likely steroid use, suggest exogenous Cushing syndrome. When Cushing syndrome is suspected, either a dexamethasone suppression test or a 24-hour urine cortisol measurement is indicated as the next step in diagnosis. If this test is positive, an MRI of the pituitary gland or CT of the adrenal gland may be performed to detect the presence of any adrenal or pituitary adenomas or incidentalomas (B, D). While this patient likely has impaired glucose tolerance due to Cushing syndrome, a glucose tolerance test (A) or fasting plasma glucose level (C) is not necessary at this time.
Striae, or stretch marks, are well-defined, symmetric, trophic lesions. They are caused by a tearing of the dermis and are a form of scarring that produces an off-color hue. They first appear as elevated reddish or purple lines in areas of rapid growth; however, they eventually flatten and fade to a pale color. Striae are often the result of rapid skin stretching. They may be associated with times of rapid growth such as puberty, weight gain, and pregnancy. In addition, striae formation is influenced by hormonal changes. Glucocorticoid hormones cause striae formation by preventing fibroblasts from forming collagen and elastin fibers necessary to keep rapidly growing skin taut. Thus striae may occur in patients with Cushing syndrome or in patients chronically treated with high-dose steroids. They can occur anywhere on the body but are most likely to appear in areas of larger fat stores (abdomen, breasts, upper arms, back, thighs, hips, buttocks). Striae are more common in women. Early-stage striae have shown improvement with the use of topical tretinoin and glycolic acid creams. Laser therapy has been shown in some cases to improve the appearance of striae as well.
▪ Appear in areas with larger fat stores
▪ Associated with times of rapid growth
▪ Influenced by hormonal changes
61. A 27-year-old woman presents to the clinic complaining of pain in her lower legs for the past 2 days. Over this time she has been feeling ill and also complains of bilateral ankle pain. On physical exam, her temperature is 100.4° F (38 ° C), and her blood pressure is 142/92. Erythematous lesions that are nodular and tender to palpation are seen on her lower legs (shown above). ESR and c-reactive protein are elevated. A chest radiograph reveals bilateral adenopathy, and sarcoidosis is suspected. The patient is scheduled for tissue biopsies. What is the best management of her lower limb findings at this time?
B. Oral prednisone with a taper
C. NSAIDs and symptomatic treatment
D. Bilateral ankle aspiration and radiographs
E. Biopsy of the edge of a nodule
62. A 23-year-old women presents to the clinic with pleuritic chest pain, bronchial cough, fatigue, and a fever for 2 weeks. She says that she went hiking and camping in southern Arizona 1 month ago. She thought she had picked up a bad cold. Her fever resolved 3 days ago; however, her fatigue, cough, and chest pain continue. She was prompted to come in yesterday when she noticed painful red nodules on her lower legs and aching knee pain. Physical exam is significant for right-sided crackles and 2- to 3-cm hard, red, tender nodules on the extensor surfaces of the lower legs. A chest x-ray shows a right middle lobe infiltrate and right hilar adenopathy. Sputum cultures are sent. Tissue samples obtained via bronchoscopy reveal spherules filled with endospores. What is the best management at this time?
C. NSAIDs and symptomatic treatment
61. The answer is C: NSAIDs and symptomatic treatment. This patient has erythema nodosum and suspected sarcoidosis. Erythema nodosum is an immunologic skin reaction showing granulomatous inflammation that has a variety of causes, including drugs, infection, inflammatory or granulomatous disease, and malignancy. Treatment is symptomatic, antiinflammatory (C), and directed at the underlying cause if known. Patients often have associated fever, malaise, and arthralgia, particularly of the ankle joints. Glucocorticoids should be used only if the etiology is known. Women are affected 10 times more frequently than men. Lesions will typically disappear after 6 weeks but may recur.
62. The answer is E: C and D only. This patient has confirmed coccidioidomycosis pneumonia with erythema nodosum. Close to 70% of all cases of erythema nodosum have an identified cause (infection, drugs, systemic illness, pregnancy). Common causes include streptococcal infection, sarcoidosis, lymphoma, and inflammatory bowel disease. NSAIDs are helpful in treating the inflammation of erythema nodosum. However, once an underlying cause for erythema nodosum has been identified, treatment of that cause, in this case fluconazole for fungal pneumonia, is indicated (E).
Erythema nodosum is an acute inflammatory, immunologic reaction to the subcutaneous fat characterized by the appearance of painful nodules in the lower legs. It represents a reaction pattern to a variety of etiologic agents, including drugs, infections, and other inflammatory or immunologic diseases. Lesions tend to be bright red, nodular, and tender to palpation, and are often accompanied by fever and malaise.
▪ Multiple and perse etiologies: drugs, infections, inflammatory or granulomatous disease
▪ Women are affected more than men (10:1 ratio).
63. A 25-year-old man with a history of mitral valve prolapse (MVP) presents with 1 day of sharp, tearing chest pain at the center of his chest that now radiates toward his neck. Physical exam reveals low blood pressure, moderate sternal depression, and a tall, thin man with long arms. What is likely to be abnormal in this patient?
64. A 16-year-old man presents to his primary care physician with a complaint of “near-sightedness.” He reports that he has recently had difficulty reading signs and discerning faces at a distance. The patient is a very tall, thin man with long arms and fingers. Physical exam reveals moderate sternal depression and striae distensae on the shoulder and axillary area. On visual acuity exam the patient is found to have 20/100 OD and 20/80 OS vision. What additional screening test will not be necessary in this patient?
E. Annual musculoskeletal evaluation for kyphoscoliosis
63. The answer is B: Fibrillin 1. This patient is having an aortic dissection and has classic findings of Marfan syndrome, including MVP, long arms, and pectus excavatum. Marfan syndrome is caused by a defect in fibrillin 1 (B). Collagen defects (A) are associated with Ehlers-Danlos syndrome, in which patients exhibit skin hyperextensibility and joint hypermobility. Low LDL and high HDL cholesterol (C and D) would put a patient at risk for an acute coronary syndrome. Urine homocystine abnormalities (E) can be seen in homocystinuria, a recessively inherited metabolic disorder that can lead to ectopia lentis, mental retardation, bone overgrowth, and a high predisposition to thromboembolism and coronary artery disease in the absence of aortic root dilation.
64. The answer is D: Annual chest x-ray. This patient exhibits many of the classic features of Marfan syndrome, including myopia, long limbs, arachnodactyly, striae distensae, and pectus excavatum. Marfan syndrome is a generalized disorder of connective tissue caused by a defect in fibrillin 1 that has primary manifestations in the skeletal, ocular, and cardiovascular systems. As a result, Marfan patients commonly suffer from disorders in these systems and must be closely screened. Annual ophthalmic exams (A), including slit-lamp examination, are necessary to screen for ectopia lentis, an upward displacement of the lens affecting up to 70% of patients with Marfan syndrome, which may lead to dislocation and acute glaucoma. Urine homocystine levels (B) should be checked in all patients suspected of having Marfan syndrome to rule out homocystinuria, a recessively inherited metabolic disorder that can lead to similar clinical manifestations as Marfan syndrome, including ectopia lentis. Annual echocardiograms (C) are indicated in all patients with Marfan syndrome to screen for MVP and dilation of the proximal aorta, which can lead to aortic dissection. Annual musculoskeletal evaluation for kyphoscoliosis (E) is particularly important in younger patients who are still growing, as severe kyphoscoliosis is frequently seen in Marfan syndrome. An annual chest x-ray (D) is not a recommended screening test for patients with Marfan syndrome.

Marfan syndrome is an autosomal dominant disorder of connective tissue protein, fibrillin 1. Abnormal connective tissue development may result in cardiovascular, musculoskeletal, skin, lung, and CNS abnormalities. Musculoskeletal features include: long limbs, arachnodactyly, pectus excavatum or carinatum, scoliosis, high arched palate, high pedal arches, and joint hypermobility. Cardiovascular features include MVP, aortic root dilation, aortic dissection, and rupture. Ocular features include superior lens dislocation and retinal detachment. A diagnosis of Marfan syndrome should also be considered in patients with recurrent spontaneous pneumothoraces secondary to rupture of blebs.
▪ Affects about 1 in 5000 people in the United States
▪ Treat with β-blockers to decrease myocardial contractility and slow rate of aortic dissection
▪ Routine echocardiogram monitoring to evaluate aortic root diameter
65. A 25-year-old Caucasian mother brings her 4-week-old girl to the office. She expresses concern that her daughter appears different than she and the father. The baby’s skin is “snow white,” as are her eyebrows and scalp hair. She appears well and exhibits normal development. Her pale blue irides are translucent, and the corneal light reflex is asymmetric. Nystagmus is present. Which advice should be given to the mother regarding her daughter’s condition?
A. She is likely to have lower-than-average intelligence and behavioral problems.
B. Obtain a peripheral blood smear.
E. She should have emergent genetic testing.
66. A 10-month-old Caucasian boy has recurrent skin and lung infections. His skin and hair are white, and his face has a pink hue. His mother says he’s the first “albino” in the family. A recent workup revealed neutropenia and neutrophils with large grayish-blue granules. Which of the following is the most appropriate treatment?
65. The answer is D: She should be under the care of an ophthalmologist and dermatologist in addition to her primary care physician. The infant has oculocutaneous albinism (OCA), evident by her white skin and hair, as well as iris translucency, nystagmus, and other ocular abnormalities. People with OCA have an increased risk of skin cancer, most commonly squamous cell carcinoma, and vision problems. Therefore they should be followed by a dermatologist and ophthalmologist (D). OCA results from a defect in melanin synthesis, causing obvious skin and hair manifestations, as well as less obvious but pathognomonic translucent irides and nystagmus. Iris translucency is best seen in a dark room with a flashlight shined at the sclera. Preventive measures to decrease sun exposure should be initiated at birth (C). OCA is not associated with cognitive or behavioral problems (A). Albinism may result from a number of genetic mutations, which can be identified with genetic testing; however, this is unlikely to affect management (E). In addition, there are special types of albinism associated with hematologic abnormalities, such as Hermansky-Pudlak syndrome and Chédiak-Higashi syndrome, but the patient in this case does not appear to have one of these syndromes (B).
66. The answer is C: Bone marrow transplant. Chédiak-Higashi syndrome is a rare autosomal recessive disorder that presents with oculocutaneous albinism and neutropenia. Giant grayish-blue granules are seen in neutrophils. The preferred treatment is bone marrow transplant (C). Patients with Chédiak-Higashi have recurrent pyogenic infections. Common organisms include S. aureus, S. pyogenes, and Pseudomonas. Patients with Chédiak-Higashi syndrome may have mild bleeding, but regular transfusions are not indicated (A). IV immunoglobulin is appropriate for some antibody-related immunodeficiencies (D). There is no role for splenectomy in the management of Chédiak-Higashi syndrome (B). Chédiak-Higashi syndrome is a serious condition that warrants aggressive management as it often results in death before the age of 7 if untreated (E).
Albinism is most commonly due to autosomal recessive mutations in melanin synthesis. It is present at birth and typically affects the eyes and skin (OCA). In OCA, there is a normal number of melanocytes, but a key enzyme in melanin synthesis, tyrosinase, is inactive.
67. A 16-year-old man presents with complaints of a rash. During the physical examination, you note multiple tiny, symmetric papules and plaques, most prominent over the trunk. A single larger lesion is present over the patient’s side. This lesion is salmon colored with a central scale located within the oval plaque. What is the best treatment for this rash?
A. No treatment is needed. It should resolve in 6-8 weeks.
B. Topical antifungal treatment
E. Topical hydrocortisone cream
68. A 23-year-old woman with no past medical history presents complaining of a 1-week history of an itchy rash on her back and abdomen. She notes that the rash initially began as a single larger patch on her abdomen one week ago. She has not recently started any new medications or changed her detergents or soaps. On physical exam the patient has several erythematous, fine, scaling plaques and patches ranging from 1-3 cm with fine collarette scales at the periphery of each lesion. What is the most likely diagnosis of this patient’s rash?
67. The answer is A: No treatment is needed. It should resolve in 6-8 weeks. This patient has classic findings of pityriasis rosea, including a herald patch and a rash most prominent over the trunk. Because this is thought to be due to a reaction to human herpesvirus (HHV) infection, the viral exanthem should resolve spontaneously in 6-8 weeks (A). Herald patches may be confused with ringworm; however, the scale of a herald patch is classically located inside the patch. In ringworm, which is caused by tinea, the scale is located outside the patch. Ringworm is due to a fungal infection and is most often treated with topical antifungals (B). In some cases, such as tinea capitis, an oral antifungal treatment (C) may be needed. Topical nystatin (D) is often used to treat candida infections. Topical hydrocortisone cream (E) is not needed to treat this viral exanthem.
68. The answer is D: Pityriasis rosea. This patient presents with the characteristic symptoms of pityriasis rosea (D), including an initial herald patch (a 2- to 5-cm, salmon-red patch that is the presenting symptom in 80% of patients) with a scale located inside the patch. This is in contrast to tinea corporis (E) that presents with scaling lesions with scales located outside the patch. Secondary syphilis presents as a papulosquamous truncal eruption that involves the palms and soles, which is not seen in this patient. Guttate psoriasis (B) is characterized by eruption of small (0.5-1.5 cm) papules over the upper trunk and proximal extremities. These lesions are much smaller than those in pityriasis and do not present with a herald patch. EM (C) presents as target lesions that may coalesce and develop erosions over the body in response to herpes simplex virus (HSV) and certain drugs.
Pityriasis rosea is an acute viral exanthem and manifests with a characteristic skin rash. The rash begins with a herald patch, a single scaly salmon-colored 2- to 5-cm oval lesion. After 1-2 weeks, a secondary eruption of smaller fine scaling papules and plaques with collarettes evolves. The secondary exanthem is distributed symmetrically in a Christmas tree–like pattern most prominent over the trunk, neck, and adjacent extremities. The long axis of these oval lesions tends to be oriented with the cleavage lines of the skin. Of note, the initial herald patch may be confused with tinea. Pityriasis rosea’s scale is located within the oval plaque, whereas tinea’s scale is located at the border of the oval plaque. Pityriasis rosea is typically self-limiting and resolves within 6-8 weeks. Treatment is usually not needed, but topical zinc oxide, calamine lotion, or moderate potency corticosteroids can be used for pruritis.
▪ Scale located within oval plaque
▪ Thought to be a reaction to HHV 7
69. A 19-year-old man presents with edematous, pruritic papules on his abdomen and chest. The lesions appeared shortly after eating a shellfish meal at a restaurant. He also complains of difficulty breathing and swallowing and has wheezing on examination. What is the most appropriate treatment for this patient?
D. Intramuscular (IM) epinephrine
70. A 23-year-old woman comes to the urgent care center complaining of a rash around her neck. For Valentine’s Day, her fiancé gave her a beautiful gold necklace. Since wearing this necklace, she has developed a skin rash notable for pale-red, raised, itchy papules and vesicles around her neck. You suspect that she has developed contact dermatitis from her necklace. Which of the following is the most likely mechanism of her rash development?
A. Type 4 delayed cell-mediated hypersensitivity
C. Cytotoxic, antibody-dependent response
D. Type 1 hypersensitivity reaction
E. Release of histamine from eosinophils
69. The answer is D: IM epinephrine. This patient is having a severe allergic reaction to shellfish. He has urticaria as well as signs of angioedema and airway constriction. Thus this patient should be given IM epinephrine (D). Benadryl (A) is an H1 blocker and ranitidine (E) is an H2 blocker. Although they are both antihistamines, epinephrine should be used as first line treatment if there are signs of airway compromise. Systemic glucocorticoids (C) can be used to alleviate urticaria, but would not be first line in this situation. Topical glucocorticoids (B) may help to alleviate the itching associated with urticaria and may help the lesions resolve, but this patient is showing concerning signs of systemic inflammation. This patient should be instructed to avoid shellfish and should carry an EpiPen in the future.
70. The answer is A: Type 4 delayed cell-mediated hypersensitivity. This woman is experiencing an allergic contact dermatitis, a type 4 hypersensitivity reaction (A). Her collar-like rash is confined to the area of allergen exposure, in this case nickel sulfate. Immune complex disease (B) is a type 3 hypersensitivity reaction, characteristic of an arthus reaction or serum sickness. Cytotoxic, antibody-dependent reactions (C) are type 2 hypersensitivity reactions. Examples include autoimmune hemolytic anemia and erythroblastosis fetalis. Type 1 hypersensitivity reaction (D) is characteristic of anaphylaxis and asthma. Histamine is not released from eosinophils (E).
Urticaria, commonly called hives, are due to either an allergic and nonallergic stimuli that causes the release of inflammatory mediators, including histamine and mast cells. Urticaria can result from contact dermatitis, food, drugs, recent upper respiratory infections, and environmental factors. Key features include evanescent wheals (raised areas surrounded by a red base) or hives. Itching is usually intense. Most incidences are acute and self-limited. Lesions typically last less than 24 hours. Chronic urticaria is defined as recurrent episodes lasting longer than 6 weeks. Urticaria may be associated with angioedema, flushing, burning, wheezing, and abdominal pain. Antihistamines and prednisone are the mainstays of treatment. If angioedema and wheezing are prominent, IM epinephrine may also be used.
▪ Most common causes: food, drugs, contact dermatitis
71. A 41-year-old woman presents with painful ulcerations of her distal fingers. On physical examination she also has nail fold capillary changes and tight thickened skin over her hands, causing loss of mobility of her fingers. Which of the following would help to confirm the diagnosis?
B. Anti–double-stranded DNA (anti-dsDNA) antibodies
C. Anti-Smith (anti-Sm) antibodies
D. Antineutrophil cytoplasmic antibody (ANCA) levels
72. A 52-year-old man presents with a change in his facial appearance. He has noticed tightening of the skin around his mouth and eyebrows. In addition, his fingers have developed a sausage-like appearance. Two years ago he had been diagnosed with Raynaud phenomenon (RP). He recalls his mother suffering from a condition severely affecting the mobility of her fingers. Which of the following is the most accurate regarding this patient’s likely diagnosis?
A. Women are four times as likely as men to develop the disease.
B. Positive anti-dsDNA and anti-Sm antibodies confirm the condition.
C. The condition can be cured with agents used to increase blood flow to the affected areas.
D. RP is a result of chronic disease progression.
E. This familial condition can be mapped to the short arm of chromosome 3.
71. The answer is D: ANCA levels. This patient has digital ulceration due to vasculitis caused by RP. In this case, the RP is likely secondary to scleroderma given the physical exam findings of nail fold capillary changes and sclerodactyly. ANA (antinuclear antibodies), anti-Scl, and anticentromere antibodies (A) are helpful in diagnosing scleroderma. Anticentromere antibody is specific for CREST, a limited form of scleroderma. Anti-dsDNA antibodies (B) and anti-Sm (C) antibodies are positive in lupus. Lupus patients may also experience RP, but the physical exam findings in this patient are consistent with scleroderma, not lupus. ANCA levels (D) can be positive in certain conditions causing vasculitis. Cytoplasmic antineutrophil cytoplasmic antibody (C-ANCA) is positive in conditions such as Wegener syndrome. Perinuclear antineutrophil cytoplasmic antibodies (P-ANCA) may be positive in Churg-Strauss syndrome, primary sclerosing cholangitis, and polyarteritis nodosa. A biopsy (E) of the ulceration will show necrosis but would not be helpful in determining a cause.
72. The answer is A: Women are four times as likely as men to develop the disease. This patient has scleroderma. Scleroderma is four times as likely in women compared to men (A). RP is an early manifestation of disease, and many patients will present with Raynaud (D). Positive anti-dsDNA and anti-Sm antibodies suggest lupus (B). Scleroderma is a chronic autoimmune condition without a cure. Treatment is aimed at alleviating symptoms (C). The cause of scleroderma is unknown, and while symptoms seem to run in families, a specific gene has not yet been identified.
Scleroderma is a chronic autoimmune disease characterized by fibrosis, vascular alterations, and autoantibodies. Limited scleroderma mainly affects the hands, arms, and face. Facial involvement may include a smooth, unwrinkled brow, tight area around the nose, and a shrunken, expressionless mouth. Involved skin feels smooth and indurated and as if it is bound to underlying structures. Areas of hyperpigmentation or hypopigmentation may be present. CREST syndrome is an example of limited scleroderma, which results in Calcinosis, Raynaud phenomenon, Esophageal dysfunction, Sclerodactyly (fibrosed skin causes immobile digits), and Telangiectasias. Pulmonary arterial hypertension is the most serious complication of this form of scleroderma. Limited scleroderma can also cause vascular changes in the extremities, such as the hands, which may lead to local ulcerations and digit ischemia. Diffuse scleroderma is rapidly progressing and affects large areas of skin and at least one internal organ—frequently the kidneys, esophagus, heart, and lungs. Fibrosis and tightening of the skin may result in flexion contractures.
▪ Anticentromere is 80% sensitive for CREST syndrome.
▪ Treatment: immunosuppressive agents, such as methotrexate
▪ Hand findings in scleroderma: Raynaud, sclerodactyly, nail fold capillary changes
▪ RP is seen in approximately 90% of patients.
▪ Women are affected three to four times more frequently than men.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree