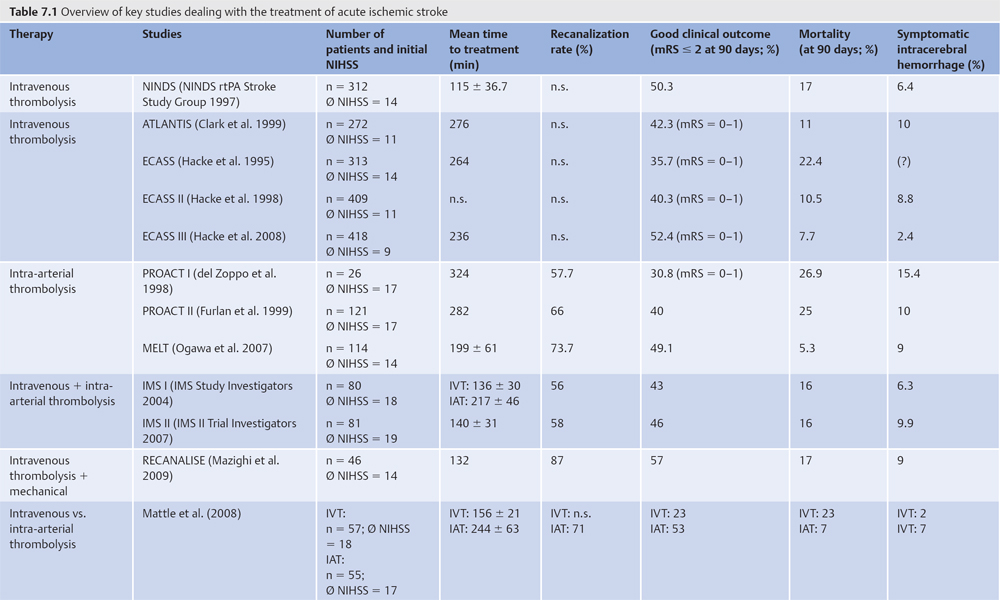
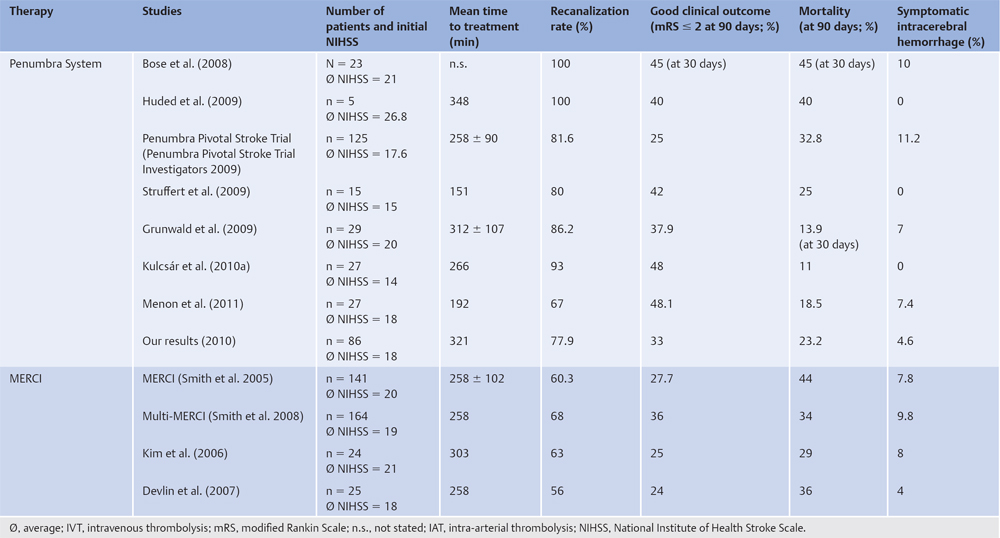
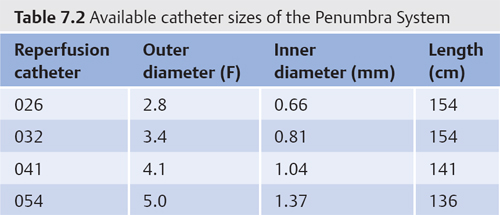
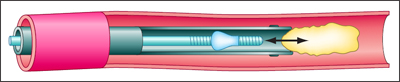
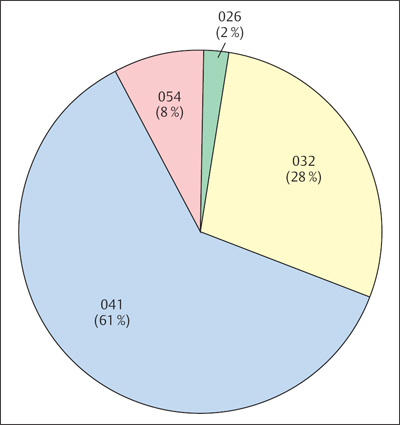
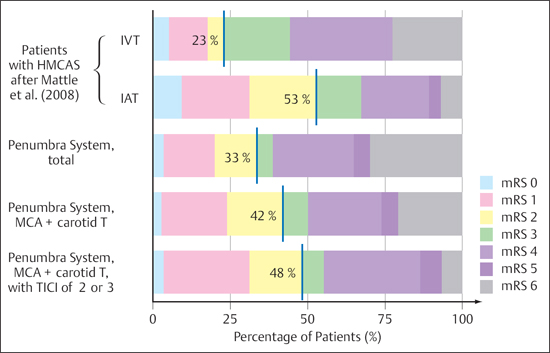
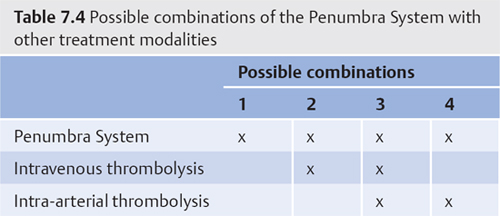
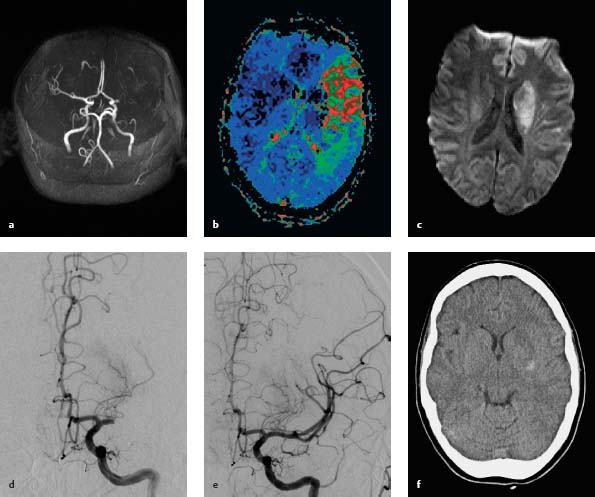
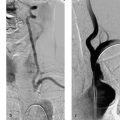
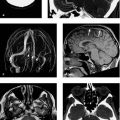
7 Mechanical Recanalization Materials The standard treatment for acute ischemic stroke is systemic (intravenous) pharmacologic thrombolysis. This therapy is widely practiced and is rapidly available following the exclusion of intracranial hemorrhage. Large, randomized, placebo-controlled double-blind studies on intravenous thrombolysis (ECASS, NINDS, ATLANTIS; Table 7.1) have shown, however, that no more than 1 in 8 patients (13%) will benefit from this therapy compared with placebo and will be able to live a (largely) independent life with no disability in daily activities (mRS ≤ 2) (National Institute of Neurological Disorders and Stroke tPA Stroke Study Group 1995). Only patients treated within the first 3 h of stroke onset were enrolled in the NINDS study. The ECASS III study showed that stroke patients can benefit from intravenous thrombolysis even beyond a time window of 4.5 h after symptom onset (Hacke et al. 2008). Longer periods of time to (intravenous) treatment are associated with higher mortality and decreased benefit from intravenous thrombolysis (Lees et al. 2010). In a meta-analysis of 53 studies on the importance of vascular recanalization in acute ischemic stroke, Rha and Saver (2007) found that recanalization had a high correlation with good functional outcomes and reduced mortality. Intra-arterial recanalization techniques were associated with significantly higher success rates than intravenous thrombolysis. The length of a vascular occlusion is a limiting factor in the efficacy of systemic intravenous thrombolysis. While intravenous thrombolysis can produce recanalization in 63% of cases where thrombus length was < 4 mm, the recanalization rate fell to 1% when thrombus length was > 8 mm (Riedel and Jansen 2009). Note In these cases, and/or cases treated outside the time window, mechanical recanalization is a potentially important option that can be used alone or in conjunction with systemic thrombolysis to achieve complete recanalization. Mechanical recanalization may employ any of three main principles: thrombus aspiration, thrombus extraction, or thrombus fragmentation. Mechanical recanalization systems currently on the market can be subdivided into three groups based on their relationship to the intravascular thrombus: • Proximal systems: These devices engage and remove the clot from the proximal side (e.g., Penumbra System, Snare, Alligator, AngioJet, EPAR). • Distal systems: These devices are deployed past the thrombus—that is, they must first be advanced through the thrombus and positioned behind it (e.g., MERCI, Catch, Phenox pCR/CRC, Lazarus, Neuronet, Snare). • On-the-spot systems: These devices are deployed within the thrombus (e.g., EKOS, stents, stent-like retrievers such as Solitaire, Bonnet, Trevo, Mindframe, ReVive, and the Penumbra System). The first aspiration thrombectomies were successfully performed with simple catheters which were particularly useful in the vertebrobasilar system. The AngioJet device (Minneapolis, MN) was developed for cardiologic and peripheral vascular recanalizations. To date, most published reports on the device have dealt with cerebrovascular applications for venous sinus thrombosis. A directional fluid jet in the catheter creates a suction effect that draws pieces of the thrombus into side holes where they are fragmented and evacuated through the catheter. The Penumbra System is widely used for mechanical recanalization in acute ischemic stroke. Classified as a proximal or on-the-spot system, it employs a combined principle of thrombus aspiration and extraction. However, based on the practice at our hospital and surveys of neurointerventionalist colleagues, we find that, at least in Germany, the system is used almost exclusively in the aspiration mode and is very rarely used for clot extraction. The Penumbra System was developed by Penumbra, Inc. (Alameda, CA, USA) and received FDA approval in late 2007. Besides the MERCI Retriever from Concentric Medical, Inc. (Mountain View, CA, USA), the Penumbra System is currently the only device approved by the United States Food and Drug Administration (FDA) for the mechanical recanalization of patients with acute is-chemic stroke in cases where intravenous thrombolysis is contraindicated or unsuccessful. Fig. 7.1 Components of the Penumbra System (with kind permission of Penumbra Europe GmbH, Berlin, Germany). The Penumbra System consists of five main components (Fig. 7.1): • Reperfusion catheter • Separator • Aspiration pump • Aspiration tubing • Canister Since the Penumbra System was introduced, seven studies and single-center study results have been published on this new treatment option; a randomized control study has not yet been conducted (see Table 7.1). Practical Tip Before mechanical recanalization starts, it must be confirmed that the patient has suffered a (symptomatic) ischemic stroke in the intracranial vascular system. Intracranial hemorrhage must be excluded. Patient selection requires an imaging study that can demonstrate the vascular occlusion and assess the size of the definitive infarction. The Penumbra System is designed for the revascularization of large intracranial vessels—the internal carotid artery (ICA), the M1 and M2 segments of the middle cerebral artery (MCA), the basilar artery, and the vertebral arteries. The manufacturer states that the device should be used within the first 8 h from stroke onset, although there are no hard data to support this recommendation. There are patients who will no longer benefit from recanalization within a considerably shorter time frame because the entire territory supplied by the occluded vessel is already infarcted. Conversely, imaging criteria may identify patients who will still benefit from (mechanical) recanalization even after a longer interval from symptom onset. This particularly applies to vertebrobasilar strokes. Percutaneous arterial access is established at a peripheral site, usually the right common femoral artery, using aseptic technique, and a sheath is introduced. Next, a guide catheter or long sheath, flushed continuously with heparinized saline solution, is introduced over a guidewire. This is followed by selective catheterization and angiographic visualization of the intracranial vessels to determine the location and extent of the thrombotic occlusion and assess collateral circulation. When perfusion status has been assessed and the decision to proceed with mechanical recanalization has been made, the reperfusion catheter is advanced to the primary occlusion site with the help of a micro-guidewire. The selected size of the reperfusion catheter depends on the site of the occlusion, the vessel diameter at that site, and the tortuosity of the approach. Penumbra reperfusion catheters and separators are available in four different sizes for vessels ranging from < 2 to > 4 mm in diameter (Table 7.2). The reperfusion catheter is navigated to the site of the vascular occlusion, and the separator is advanced through the reperfusion catheter. Its function is to facilitate aspiration of the thrombus and prevent clogging of the aspiration catheter. The aspiration pump, which is connected to the reperfusion catheter by tubing, generates a continuous suction of -20 inches of mercury (= –677.2 mbar). Mechanical recanalization is achieved by repeatedly advancing and retracting the separator through the reperfusion catheter and thrombus while the fragments are aspirated through the catheter (Fig. 7.2). The 041 reperfusion catheter is the size most often used at our hospital in Göttingen, Germany. To date we have used it in 61% of interventions. The 041 catheter can reach occlusions as far as the M1 segment of the MCA and in the vertebrobasilar system, depending on individual circumstances. The 032 and 026 catheter sizes are better for accessing more distal thrombi or secondary emboli (Fig. 7.3). An average of 1.47 Penumbra Systems are used per intervention at our center. Exchanges may be necessitated by a distal taper of the vessel diameter or the fragility of the separator tip, which should be replaced after several reperfusion maneuvers. Various grading scales can be used to document vascular status before and after mechanical recanalization. The TICI score (Thrombolysis in Cerebral Infarction; Table 7.3) is widely employed (Higashida et al. 2003). Other scoring systems are the TIMI (Thrombolysis in Myocardial Infarction; see the section on Concepts, and Table 8.1, p. 111) and the Qureshi Grading System. Fig. 7.2 Functional principle of the Penumbra System (with kind permission of Penumbra Europe GmbH, Berlin, Germany). Fig. 7.3 Frequency of use of different reperfusion catheter sizes in the Penumbra System. The 041 reperfusion catheter, with an outer diameter of 4 1F and a luminal diameter of 1. 04 mm, is most commonly used. Note On the whole, it has been our experience that few complications arise during mechanical recanalization. The most frequent complication in our patients was intracerebral vasospasm, which occurred in 8.1% of interventions but was easily managed with drug therapy. Symptomatic intracranial hemorrhage occurred in 4.6% of our patients. Incidences of 0–11.2% have been reported in previous publications on the Penumbra System (see Table 7.1). Thus, the rates of symptomatic intracranial hemorrhage at our center are no higher than the rates reported in large studies of intravenous thrombolysis (e.g., ECASS III). We experienced a 4.6% rate of periprocedural iatrogenic dissections of the ICA. In all of these cases, significant disruption of blood flow was prevented by careful stenting of the dissection. We have had two cases of separator breakage (2.3%) at our center. Because the break occurred at a proximal site, retrieval was easily accomplished in both cases. In another published case (Kulcsár et al. 2010) the distal tip of the separator broke off and was lost in the thrombus of the M2 segment. Menon et al. (2011) observed distal emboli in 48.1% of their patients treated with the Penumbra System. Other publications did not make significant mention of this phenomenon. Table 7.3 TICI perfusion categories (after Higashida et al. 2003) TICI grade Perfusion Description 0 No perfusion No antegrade flow beyond the point of occlusion 1 Penetration with minimal perfusion The contrast material passes beyond the area of obstruction but fails to opacify the entire cerebral bed distal to the obstruction for the duration of the angiographic run 2 Partial perfusion The contrast material passes beyond the obstruction and opacifies the arterial bed distal to the obstruction. However, the rate of entry of contrast into the vessel distal to the obstruction and/or its rate of clearance from the distal bed are perceptibly slower than its entry into and/or clearance from comparable areas not perfused by the previously occluded vessel, e.g., the opposite cerebral artery or the arterial bed proximal to the obstruction 2a Only partial filling (<2/3) of the entire vascular territory is visualized 2b Complete filling of all of the expected vascular territory is visualized, but the filling is slower than normal 3 Complete perfusion Antegrade flow into the bed distal to the obstruction occurs as promptly as into the obstruction and clearance of contrast material from the involved bed is as rapid as from an uninvolved bed of the same vessel or the opposite cerebral artery Other complications have been reported in a few sporadic cases: • Inguinal hematoma • Reocclusion of the target vessel • Vascular perforation • Vascular dissection • Infarction in a new vascular territory Among the patients treated at our center, 79% of the vascular occlusions were located in the anterior circulation and 21% were in the vertebrobasilar system. Partial or complete recanalization, corresponding to a TICI score of 2 or 3, was achieved in 77.9% of the interventions with the Penumbra System. The following treatment modalities were used: • Mechanical only: 18.2% • Intravenous thrombolysis + mechanical: 11.4% • Intra-arterial thrombolysis + mechanical: 34.1% • Intravenous thrombolysis + intra-arterial thrombolysis + mechanical: 36.4% In the studies published thus far, the Penumbra System, usually combined with chemical thrombolysis, has achieved high recanalization rates with a weighted average of 82.25% (67–100%; see Table 7.1). To date, these high recanalization rates have been matched only by stent-like recanalization systems such as Solitaire or Trevo used in small experimental series. In an initial trial of the MERCI Retriever, also approved for mechanical thrombectomy, recanalization was achieved in 48% of patients in whom the device was deployed (Smith et al. 2005). The subsequent Multi MERCI trial (Smith et al. 2008) achieved a recanalization rate of 69.5%. In both trials, thrombolytic agents were used as an adjunct to recanalization with the MERCI device. Thus, the rates for recanalizing cerebral vessels with aspiration systems are considerably higher than the rates reported in a meta-analysis by Rha and Saver (2007) for spontaneous (24.1%), intravenous (46.2%), and intra-arterial fibrinolysis (63.2% of patients treated). At our center, we documented a good clinical outcome after rehabilitation (mRS ≤ 2) in 33% of the patients treated with the Penumbra System. While 39% of the successfully recanalized patients achieved an mRS ≤ 2, only 19% of patients did so in the cohort without successful recanalization. Previously published clinical data on the Penumbra System also indicate a weighted average of 33.55% (25–48.1%) for a good clinical outcome 90 days after the stroke event. An average of 31.1% (24–36%) of patients treated with the MERCI Retriever had a good clinical outcome at 90 days. A more striking difference was found in the weighted mortality rates at 90 days: 27.49% (11 -40%) for the Penumbra System vs. 37.78% (29–44%) for the MERCI Retriever. In a direct comparison of intravenous and intra-arterial thrombolysis in comparable patients with a HMCAS on cranial CT, Mattle et al. (2008) documented a significantly better outcome in patients treated with intra-arterial thrombolysis. When we compare these findings with the results in our own patients with carotid-T and MCA occlusions that would be expected to have a HMCAS on cranial CT, we find a similarly good clinical outcome in patients who were successfully recanalized (TICI score of 2–3; Fig. 7.4). Fig. 7.4 Comparison of clinical outcomes of treatment with intravenous and intra-arterial fibrinolysis (after Mattle et al. 2008) or after mechanical recanalization with the Penumbra System in patients with a HMCAS. An mRS of 2 or less at 90 days after the stroke event is interpreted as a good outcome. HMCAS, hyperdense middle cerebral artery sign; IAT, intra-arterial thrombolysis; IVT, intravenous thrombolysis; TICI, thrombolysis in Cerebral Infarction Score (after Higashida et al. 2003). In principle, it should be possible to combine aspiration therapy with other recanalization techniques. Table 7.4 shows the possible combinations that may be used in clinical practice. A combination of pharmacologic and mechanical thrombolysis in the patients at our center yielded a higher recanalization rate (average of 75.0%; n =58) than with use of the aspiration system alone (average of 72.2%; n =18). Practical Tip We achieved particularly good recanalization results by combining copious intravenous bridging thrombolysis (> 20 mg rtPA) with subsequent use of the Penumbra System. One possible explanation is that preliminary rtPA therapy ”softened” the thrombus and made it easier to aspirate. The addition of intra-arterial thrombolysis should further reduce the thrombus burden at the primary occlusion site, further improve perfusion beyond the revascularized occlusion, and dissolve any distal emboli that may be present. A 25-year-old woman was transferred from another hospital with a suspected left hemispheric stroke marked by a progressive decline in vigilance, decreased movement on the right side of the body, and positive pyramidal tract signs on the right side (NIHSS = 14, mRS = 5). Multimodal MRI revealed an occlusion of the left MCA (Fig. 7.5a) with a significant perfusion delay in the affected territory; the diffusion abnormality was still relatively small (Fig. 7.5b, c). After the exclusion of intracranial hemorrhage, the patient was selected for mechanical thrombolysis. Angiography commenced at 4.5 h after symptom onset using a 6F Envoy catheter to define the intracranial vessels. Angiograms confirmed a complete occlusion of the M1 segment of the MCA with a TICI score of 0 (Fig. 7.5d). The Penumbra 041 reperfusion catheter was positioned proximal to the thrombus, and the clot aspirated swiftly and without difficulty over a period of 24 min. Control angiograms showed complete recanalization of the MCA trunk (Fig. 7.5e). Then 20 mg of rtPA was slowly infused into the MCA through the indwelling guide catheter. Cranial CT on the day after mechanical thrombectomy showed a circumscribed infarction of the left basal ganglia with minimal associated hemorrhage ( Fig. 7.5f). The infarcted area did not extend beyond the diffusion abnormality detected before the intervention. Eighteen days later, after a period of early inpatient rehabilitation, the patient was discharged from acute hospital care to a rehabilitation facility with her clinical neurologic status significantly improved (NIHSS = 5, mRS = 2). Mild coordination problems and word-finding difficulties were still present at discharge but were successfully addressed in the 22-day rehabilitation program. The patient returned home without significant disability and is able to live an independent life (NIHSS = 0, mRS = 1). Fig. 7.5a–f Case report of an aspiration thrombectomy with the Penumbra System. a Initial MRA shows a complete occlusion of the left MCA. b TTP map shows a large perfusion delay in the MCA territory. c DWI (b = 1000) displays the hyperintense core of the infarction The core appears small relative to the MCA territory and the area of the perfusion deficit. d DSA confirms a complete occlusion of the M1 segment of the MCA. e Status following successful recanalization of the M1 segment. f Next-day cranial CT shows a left basal ganglia infarction with small associated hemorrhage. The infarcted area does not extend beyond the diffusion abnormality seen on preinterventional images. Mechanical recanalization is already widely practiced at larger hospitals with expertise in interventional neuroradiology. The application of mechanical recanalization techniques requires a trained and experienced team of neuroradiologists who can administer the treatment safely and effectively. Nevertheless, there is still a lack of large, randomized, placebo-controlled studies on mechanical recanalization that would enable a direct comparison of functional outcomes with intravenous thrombolysis. The Penumbra System has shown an effective recanalization success rate in clinical practice in patients with long-segment intracranial vascular occlusions, even when used beyond 4.5 h from symptom onset. Very distal occlusions are difficult to reach with the Penumbra System and therefore limit the applications of the device. Vascular kinking is another potential difficulty. Aspiration thrombectomy is a safe procedure associated with few complications. The maximum incidence of symptomatic intracranial hemorrhage is ~10%. On the other hand, Rha and Saver (2007) found that there was no significant difference in the incidence of symptomatic hemorrhages between successfully recanalized patients and nonrecanalized patients. Since intra-arterial therapies are performed under angiographic control, the times to treatment are longer than with intravenous thrombolysis. But this delay can be effectively offset by bridging therapy, which may consist of a single bolus injection of the fibrinolytic agent (1/10 the standard dose) or the infusion of a complete dose prior to the intervention. Early intravenous thrombolysis after the exclusion of contraindications appears to be an effective strategy based on available data and can reduce the impact of the time delay for intra-arterial therapy. Initial bridging therapy followed by mechanical thrombectomy combines the two advantages of each modality: rapid availability and high recanalization rates. In a study of stroke patients with HMCAS, Mattle et al. (2008) found that the group of patients treated by intra-arterial fibrinolysis had a significantly better outcome at 90 days than the group treated intravenously, despite the average time to treatment being 88 min longer. Study data indicate that not all patients undergoing successful mechanical recanalization benefit from the procedure (Hussein et al. 2010). It is important, however, to distinguish between successful recanalization at the site of the arterial occlusion and successful reperfusion of the brain tissue supplied by the occluded vessel (Rha and Saver 2007). Reperfusion is probably the critical factor in terms of patient benefit. Furthermore, improved patient selection is probably one of the most important issues to achieve a higher proportion of patients with a favorable clinical outcome. Note This underscores the importance of the prompt identification and selection of patients who may potentially benefit from endovascular recanalization.
Aspiration Thrombectomy
Introduction
Penumbra System
Indications and Contraindications
Technique
Complications
Recanalization Rate and Neurologic Outcome
Combination Therapies
Case Report
Summary
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree