Figure 2-1. Normal postoperative finding. [A] Positioning of the probe. [B] Corresponding 12-5 MHz US image obtained after subacromial decompression demonstrates expected loss of the normal convex contour of the supraspinatus tendon (arrowheads) following removal of the subacromial-subdeltoid bursa.
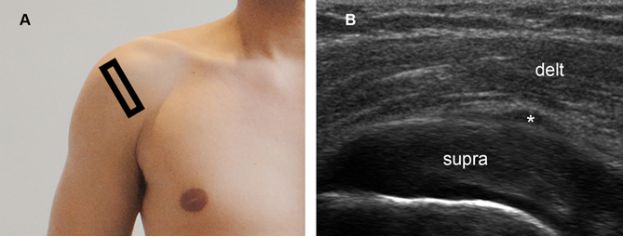
Figure 2-2. Normal postoperative finding. [A] Positioning of the probe. [B] Corresponding 12-5 MHz US image shows bursitis-like abnormality (asterisk) as a normal finding following removal of the subacromial-subdeltoid bursa. Supra= supraspinatus. Delt= deltoid.
Acromioplasty removes bony excrescences located on the undersurface of the acromion that cannot be confidently assessed by US because of shadowing. Distal clavicle resection is not routinely included but may occasionally be performed to treat refractory concomitant acromioclavicular joint disease. In these cases, adequate resection of the superior and posterior cortical margins is crucial to the long-term success and postoperative US depicts widening of the acromioclavicular joint space that should not be confused with pathology (figure 2-3).
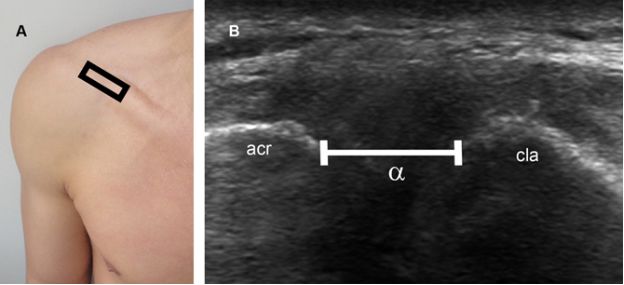
Figure 2-3. Normal postoperative finding following distal clavicle resection. [A] Positioning of the probe. [B] Corresponding 12-5 MHz postoperative image shows widening of the acromioclavicular joint space (α) secondary to surgical resection of the distal clavicle. With resection of the distal part of the clavicle, acromioclavicular distance typically increases 1-2 cm. Acr= acromion. Cla= clavicle.
Symptoms persisting after isolated subacromial decompression are commonly caused by abnormalities unrelated to the rotator cuff that still mimic subacromial impingement such as glenohumeral joint instability (see video 5-10) and acromioclavicular joint osteoarthritis (see figure 5-6). Refractory symptoms may also result from residual impingement and/or coexisting rotator cuff lesion.
2.2.2. Isolated Tendon Repair
Tendon repair is currently the standard surgical treatment for rotator cuff tears. Historically, most tendon repairs had been accompanied by subacromial decompression, but there has been an increasing frequency of isolated arthroscopic tendon repair in recent years based on growing evidence that successful treatment of a rotator cuff tear does not require routine surgical alteration of the acromion and/or coracoacromial arch.13,14 Proximal small full-thickness tears that leave a distal tendon stump attached to the greater tuberosity can be repaired using side-to-side or end-to-end tendon suturing technique. In either case, postoperative US may depict suture material as elongated hyperechoic structures within the tendon (figure 2-4). Distal tears that involve tendon insertion and large proximal tears require reattaching the proximal tendon to bone. Reattachment is performed using a screw inserted into the proximal humerus to function as an anchor. Prior to the insertion of this anchor a cortical trough is surgically created to promote bleeding and fibrovascular response with angiogenesis at the bone-tendon interface.15 The anchor is then placed just outside this trough and sutures that are attached to the anchor are passed through the rotator cuff where it is torn away from the bone resulting in the reattachment of the ruptured tendon to the humerus over the bleeding surface (figure 2-5). The following vascular response may be depicted as increased tendinous and peritendinous blood flow on Doppler evaluation during the first few months after surgery (figure 2-6).16,17 Adequate settings are essential to maximize low flow detection, and the color box must be sized to the area of interest to optimize system resources. A false-positive Doppler interrogation may result if motion artifacts or the background noise are confounded with blood flow. Spectral analysis should be used liberally to avoid these pitfalls, since only interrogation of true vessels generates a spectral Doppler tracing.18 However, even when performed with careful technique, the role of Doppler evaluation is unclear: one study shows that the intensity of vascular response does not correlate with recurrent tears,16 while another suggests that tendons with a defect at 3 months after surgery are relatively avascular.19 Less controversial, gray-scale evaluation typically depicts suture material in proximity to the greater tuberosity surface, connecting the anchor to the tendon (figure 2-7). Tears larger than 3 cm commonly require mobilization of the remaining tendon in the supraspinatus fossa before reattachment.
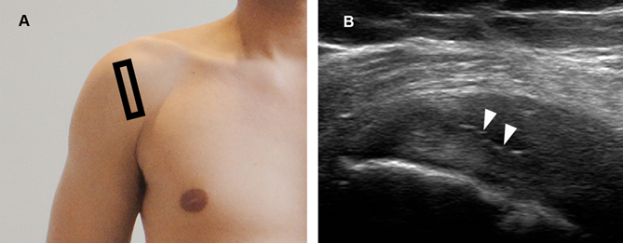
Figure 2-4. Normal postoperative finding. [A] Positioning of the probe. [B] Corresponding 12-5 MHz US image depicts suture material as hyperechoic elongated structures (arrowheads) within the supraspinatus tendon following repair.
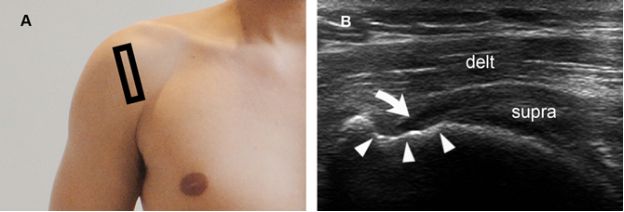
Figure 2-5. Normal postoperative finding. [A] Positioning of the probe. [B] Corresponding 12-5 MHz US image shows proximal supraspinatus tendon reattached to bone (curved arrow). The cortical depression at the insertion site is also a normal finding (arrowheads) and corresponds to the cortical trough that is surgically created to promote fibrovascular response at the bone-tendon interface. Supra= supraspinatus. Delt= deltoid.

Figure 2-6. Normal postoperative finding. [A] Positioning of the probe. [B] Corresponding 12-5 MHz power Doppler image shows normal increased blood flow in peritendinous (1) and suture anchor site (2) two months after tendon repair.
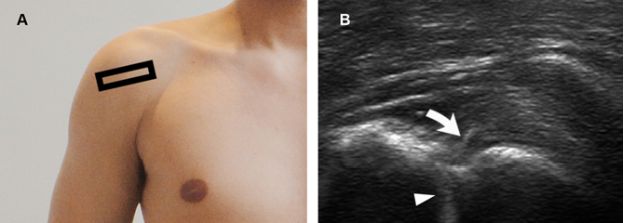
Figure 2-7. Normal postoperative finding. [A] Positioning of the probe. [B] Corresponding 12-5 MHz US image depicts suture material (curved arrow) connecting the anchor to the tendon following reattachment. Suture anchors are depicted as bright linear echoes with faint reverberation artifact (arrowhead).
The most common causes of clinical failure following repair are concomitant rotator cuff tendinopathy (see section 7.1 in chapter 1), adhesive capsulitis (see chapter 8), rotator cuff tear arthropathy (see figure 5-25), dislocated anchors (figure 2-8), fluid collections (figure 2-9), deltoid muscle atrophy, and recurrent tears.
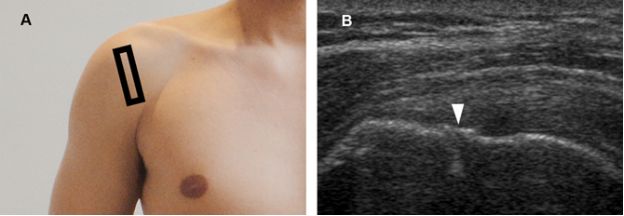
Figure 2-8. Dislocated anchor. [A] Positioning of the probe. [B] Corresponding 12-5 MHz US image shows a superficially dislocated anchor as a step up deformity of the bone contour (arrowhead). Note also a faint reverberation artifact originating from the suture anchor.

Figure 2-9. Postoperative fluid collection. [A] Positioning of the probe. [B] Corresponding 12-5 MHz US image shows a superficially dislocated anchor (arrowhead) and fluid collection (asterisk) following tendon repair.
Postoperative deltoid atrophy reflects the extent of surgical invasiveness and is significantly more common after open repair. It may be caused by loss of the origin of the muscle, more extensive muscle dissection, or injury to the axillary nerve.
Postoperative atrophy of the anterior fibers of the deltoid muscle may result in serious difficulty to perform daily living activities because no other muscles can effectively compensate for lost forward flexion of the shoulder (figure 2-10).
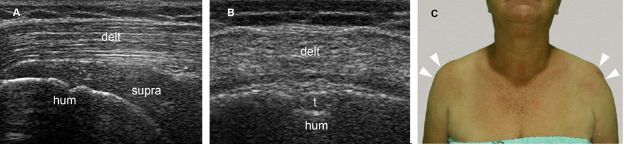
Figure 2-10. Deltoid muscle atrophy. [A] Coronal oblique 12-5 MHz US image shows reduced volume and increased echogenicity of the anterior fibers of the deltoid muscle secondary to atrophy (delt). [B] Axial 12-5 MHz US image obtained from a ventral approach also shows deltoid muscle atrophy. [C] Clinical inspection shows left deltoid atrophy (arrowheads) and a large cutaneous scar following open repair. Supra= supraspinatus tendon. Hum= humerus. T= long head of the biceps brachii tendon.
A key component to demonstrate small distal recurrent full-thickness tears is to perform graded compression with the probe in different shoulder positions. Another feature of retears is visible suture material without surrounding rotator cuff tendon. Most recurrent tears occur atraumatically in the first 3 months after surgery or 2 to 5 years postoperatively related to sports activities or direct trauma (figure 2-11).20 Recurrent full- thickness tears are also more likely to develop in the elderly21,22 or after repair of large defects (figure 2-12).23 They do not imply in inadequate surgical technique and may result from advancing preoperative rotator cuff disorder.
The postoperative diagnosis of partial-thickness recurrent tears is far more debated. Altered echogenicity and irregularities of the tendon contour do not have the same relevance as in preoperative setting because the sonographic appearance of pathological tendons does not return to normal after successful intervention. The purpose of surgery is to decrease or eliminate shoulder pain and to restore function and strength, not to bring tendon morphology back to prelesional status. Some pitfalls during the investigation of partial-thickness tears must also be considered. For example, reattachment to bone produces loss of the normal convex contour of the distal tendon and mimics a bursal surface tear (figure 2-13). Also, there is considerable variability in tendon thickness following repair, and thinning is a normal finding at serial postoperative evaluation as edema from manipulation gradually subsides. In summary, from a practical perspective, it is not prudent to consider the diagnosis of recurrent partial-thickness tear based on tendon irregularity, thinning, or altered echogenicity in the postoperative setting. In fact, the imaging diagnosis of recurrent partial-thickness tears is of little importance because this finding is usually clinically irrelevant and there is no correlation between tendon thickness and pain after surgery.24
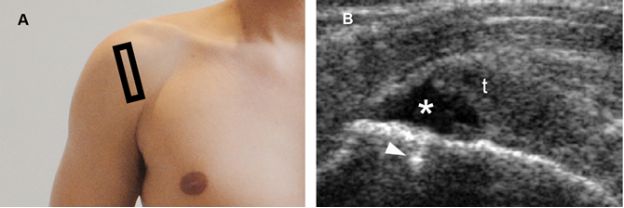
Figure 2-11. Recurrent full-thickness tear. [A] Positioning of the probe. [B] Corresponding 12-5 MHz US image shows a recurrent full-thickness tear of the supraspinatus tendon (asterisk) following reattachment. Note also absent suture material connecting the anchor (arrowhead) to the ruptured supraspinatus tendon (t).
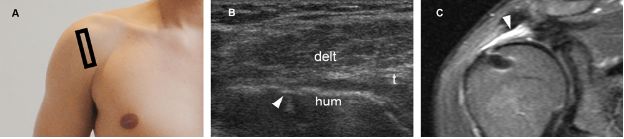
Figure 2-12. Recurrent full-thickness tear. [A] Positioning of the probe. [B] Corresponding 12-5 MHz US image shows abnormal close apposition of the deltoid (delt) and humeral head (hum) secondary to recurrent full-thickness tear of the supraspinatus tendon. Note also absent suture material connecting the anchor (arrowhead) to the ruptured supraspinatus tendon (t). [C] Corresponding coronal oblique STIR MRI confirms recurrent full-thickness tear (arrowhead).
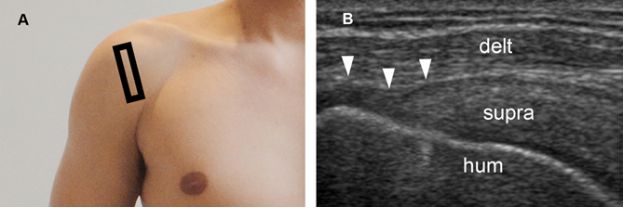
Figure 2-13. Normal postoperative finding. [A] Positioning of the probe. [B] Corresponding 12-5 MHz US image following supraspinatus tendon (supra) reinsertion shows deltoid muscle (delt) closely applied to the humeral head (hum) mimicking a bursal surface partial-thickness recurrent tear (arrowheads).
2.2.3. Combined Subacromial Decompression and Tendon Repair
Combined subacromial decompression and tendon repair is a common surgical treatment for subacromial impingement with an associated rotator cuff tear. Sonographic postoperative evaluation encompasses a combination of normal and abnormal findings of both subacromial decompression and tendon repair (see above). However, combined subacromial decompression may differ from isolated decompression because in the former the coracoacromial ligament is usually preserved in the absence of definite subacromial impingement in order to prevent postoperative superior migration of the humerus.
As in the case of isolated tendon repair, minor to moderate joint effusion is a normal finding and can be found after successful interventions (figure 2-14).
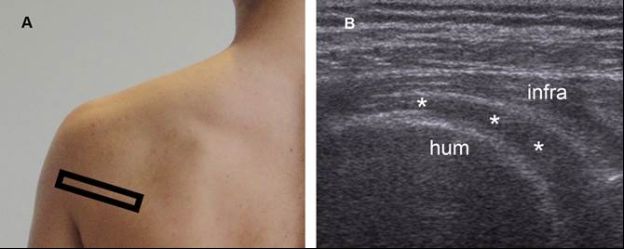
Figure 2-14. Normal postoperative finding. [A] Positioning of the probe. [B] Corresponding 12-5 MHz US image shows small to moderate joint effusion collected in the posterior glenohumeral recess (asterisks). Hum= humerus. Infra= infraspinatus.
2.2.4. Tendon Transfer
Tendon transfer is usually reserved for larger tears accompanied by severe muscle atrophy. During the procedure, a muscle-tendon unit is transferred from one location to another in order to substitute the lost motor function.
Several techniques are employed to mobilize and reconstruct tendon defects, including tendon transfer taken from the subscapularis, latissimus dorsi, pectoralis major, allografts, synthetic graft material, and xenografts.25-29 Sonographic findings depend on the surgical technique and results are generally better when the repair is performed with mobilization and transposition of existing cuff tissue rather than through implantation of allografts or synthetic material.30,31
2.3. Correlation of Postoperative Imaging Findings and Clinical Outcomes
Currently available evidence suggests that although persistent and recurrent tears may be associated with poorer functional outcomes and more severe fatty atrophy of the rotator cuff muscles,32-36 they are not necessarily synonymous with clinical failure.37,38 Such apparently contradictory statement can be at least partially explained by inconsistent definitions of what constitutes a clinical failure, because objective functional deficit assessed by physical examination may not match with subjective metrics perceived by the patient nor influence on daily living activities. At imaging, documenting a relationship between clinical outcomes and sonographic findings is challenging because US depicts anatomical damage, and several features other than anatomical damage may be involved in clinical failure such as mechanical factors and psychological profiles. Sonographers should be aware that some patients with refractory symptoms will have a normal imaging evaluation, and the opposite is also true: some asymptomatic patients satisfied with the result of the surgery will have abnormal findings at postoperative US. Imaging findings following surgery always require clinical correlation, and a postoperative recurrent tear by itself is not an absolute indication for surgical reintervention.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree