Approximately 30,000 spinal injuries occur in the United States every year. Injuries to the spine and its contents affect predominately young, healthy individuals and are a major cause of disability, with significant socioeconomic consequences. The main cause for spinal injuries is blunt trauma, most commonly caused by motor vehicle accidents, followed by falls and sport injuries. Already, in the initial evaluation of patients who have blunt trauma, multislice CT with two-dimensional (and threedimensional) reformatting is the method of choice. The liberal use of MR imaging is recommended to assess for injuries to soft tissue, the spine and its contents, intervertebral discs, and ligaments.
Injuries to the spinal column and the spinal cord are a major cause of disability, affecting predominantly young, healthy individuals. Approximately 30,000 spinal injuries occur in the United States every year. Up to 60% of the injuries affect young, healthy males between 15 and 35 years of age. Therefore, the socioeconomic consequences are important, and the costs of lifetime care and rehabilitation are extremely high, often more than $1,000,000 per individual .
Most spinal trauma involves cervical spine injuries, with more than 10,000 cervical fractures and more than 4000 thoracolumbar fractures diagnosed per year. The main cause for spinal injuries is blunt trauma, most commonly caused by motor vehicle accidents (48%), followed by falls (21%) and sport injuries (14.6%). Assault and penetrating trauma account for approximately 10% to 20% of cases. Almost one half of spinal injuries result in neurologic deficits, which are often severe and sometimes fatal . Survival is inversely related to the patient’s age, and the mortality rate during initial hospitalization is reported to be almost 10% .
Injury to the spinal cord occurs in 10% to 14% of spinal fractures and dislocations . Injuries of the cervical spine are by far the most common cause of neurologic deficits, which occur in almost 40% of the cases . Most (85%) injuries to the spinal cord occur at the time of trauma, and 5% to 10% are present in the immediate postinjury period .
Imaging modalities
Plain film radiography
In cases where multislice CT (MSCT) is not available, plain film radiographs remain the initial imaging modality. To clear the cervical spine, a minimum of three sets of views must be obtained: a lateral, an anteroposterior, and an open-mouth, odontoid view. Often, additional views, such as oblique views or the swimmer’s view, are performed in an attempt to clear the cervicothoracic junction. Flexion and extension views are contraindicated in the acute setting. They usually do not add any additional information , and, in the acute setting, cases of unstable ligamentous injury may be masked by neck pain and muscle spasm, which limit the range of motion on extension-flexion views . The potential benefit of flexion and extension views is in the subacute setting 2 to 4 weeks after the trauma, to rule out delayed cervical instability .
The presence of neurologic deficits, back pain, and a Glasgow Coma Score of eight or less gives an overall sensitivity of almost 100% for the clinical evaluation of spinal trauma in the setting of blunt trauma . Overall, the sensitivity of plain films in diagnosing spinal injuries, especially injuries in the cervical spine, varies, ranging from 39% to 94%, with variable specificity . Several studies have proved that if only plain radiographs are used, 23% to 57% of all fractures of the cervical spine are missed . Delays in the diagnosis of clinically significant cervical spine injuries have been reported in approximately 5% to 23% of patients in various series, most of which used plain films as the initial screening modality.
CT
Today, MSCT (or single-slice helical CT) is the initial method of choice when evaluating the cervical spine for bone injuries after blunt trauma . CT not only detects fractures with higher sensitivity than plain films, but can detect soft tissue abnormalities, such as disc herniation and paravertebral soft tissue and intraspinal hematoma. MSCT allows whole-spine examination in a very short time, and fast reformatting of images in multiple planes allows for a better and more exact diagnosis of bone and soft tissue abnormalities. With the introduction of these new CT imaging techniques, most trauma centers have set up dedicated, acute, multitrauma protocols that include CT of the brain, cervical spine, thorax, and abdomen, with subsequent reformatting of images of the thoracic and lumbar spine. In addition, several institutions have completely replaced plain films with MSCT in blunt spinal trauma patients, especially for the cervical spine, including two- and three-dimensional reformatting. The use of axial CT only is obsolete because of its limitations in demonstrating subluxations, increased intervertebral distances, angulations, or horizontal fractures. One study demonstrated that axial CT only detected 54% of dislocations and subluxations in trauma patients .
Typically, (spiral) MSCT in high-resolution mode with 1.25- to 2-mm–thin slices in the C1-C2 region, 2- to 3-mm–thin slices in the rest of the cervical spine and 3- to 4-mm–thin slices in the thoracic and lumbar spine are chosen for axial presentation. Sagittal and coronal reformatted images of the entire spine are produced from contiguous, submillimeter (0.3–0.75 mm) axial images, or, on the older scanners, from thicker slices that have been reconstructed with overlapping (eg, at 1.5 mm). In addition to reconstructions with bone algorithm, reconstructing images with soft tissue algorithm has been proposed to facilitate the evaluation of, for example, intra-and extraspinal hemorrhage or disc herniation.
MR imaging
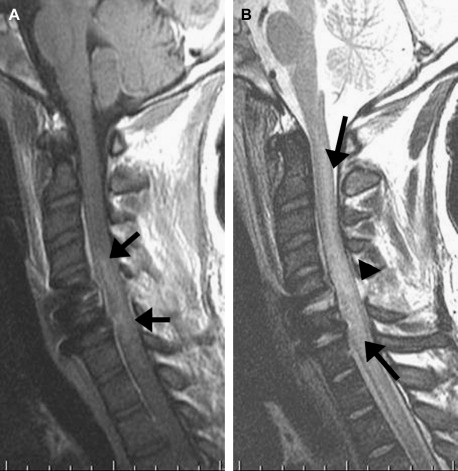
MR imaging is the imaging modality of choice for assessing soft tissue injuries, spinal cord injury, intervertebral discs and ligaments, and vascular injuries . MR imaging is the only method that can differentiate spinal cord hemorrhage from edema, which might be of prognostic significance and possibly may change the treatment ( Fig. 1 ). MR imaging is the examination of choice for excluding instability, proving or excluding cord or disc injury in patients who have focal neurologic signs, and for those who need preoperative spinal canal clearance before surgery. Compromise of the spinal canal and neural foramina, and cord compression in the presence or absence of an acute fracture, also can be evaluated sufficiently with MR imaging. MR imaging allows for better differentiation between acute and chronic compression fractures and bone marrow abnormalities. In addition, posttraumatic sequelae, such as syrinx formation, myelomalacia, and cord atrophy or tethering, typically are examined and evaluated with MR imaging. Performing MR imaging involves some safety issues, especially in assaulted patients who have penetrating injuries. The possibility for bullet or other metallic fragments close to the spinal canal to move and cause cord injury has to be considered . However, the results of some small series have shown no adverse effects in patients who have bullets within, or in close proximity to, the spinal canal . Because many patients who have suspected spinal injury are severely and critically ill, issues with halos or ventilators, the need for monitoring during scanning, and the presence of other extensive serious injuries to the brain, chest, or abdomen have to be considered; MR imaging–compatible devices have to be used when these patients are brought to the MR imaging unit. Today, these safety issues can be handled in most cases. However, most centers use MR imaging as an additional modality, and have a dedicated spine trauma MR imaging protocol, which includes several of the following sequences:
Sagittal T2 short-T1 inversion recovery (STIR), T2-weighted, and T1-weighted images, pre- and postcontrast
Axial T1-weighted images, pre- and postcontrast
Axial T2-weighted, fat-saturated images for ligamentous and soft tissue injuries
T2 ∗ gradient echo images to evaluate for small hemorrhage or blood products in the spinal cord
Criteria for imaging and choice of imaging modality
One of the critical decisions in the emergency clinical setting is determining which patients require imaging of the spine. Different studies have tried to separate low-risk from high-risk patients . The National Emergency X-Radiology Utilization Study (NEXUS) established five criteria to classify the patients having a low probability of injury . These criteria included no midline cervical tenderness, no focal neurologic deficit, normal alertness, no intoxication, and the absence of a painful distracting injury. The negative predictive value of this tool was 99.8% , but with a low specificity value of only 12%. Other retrospective studies have found the NEXUS low-risk criteria to be less sensitive (92.7%) but to have a higher specificity, 37.8% . Another, perhaps more sensitive or more accurate, method is the Canadian C-spine rule . The Canadian C-spine rule divides patients into high-risk versus low-risk patients, based on the presence of high-risk factors that mandates radiography, or the presence of any low-risk factor that allows the safe assessment of a range of motion. The high-risk factors are 65 or more years of age, dangerous mechanism, or paresthesias in extremities. The low-risk factors include simple rear-end motor vehicle collision, a sitting position in the emergency department, whether the patient has been ambulatory at any time since the trauma, the delayed onset of neck pain, or the absence of midline cervical spine tenderness. In addition, patients in a recent study were evaluated as to whether they were able to rotate their necks 45° to the left and right, by cross-validation, this rule had a 100% sensitivity and a 42.5% specificity for identifying clinically important cervical spine fractures .
The choice of modality depends on several factors, such as the availability of the different imaging modalities, the patient’s clinical and neurologic condition, the type of trauma (blunt, single, or multitrauma), other associated injuries to the brain, thorax, or abdomen, complaints of pain or limited neck or spine motion, the presence of permanent or transient neurologic deficits, and, finally, the reason for the examination (high clinical suspicion of spinal injury versus just a question of excluding injury for legal reasons in a patient with very low suspicion). A special group of patients is composed of those who need spinal cord and spinal canal clearance before surgery, in which case MR imaging is the method of choice.
Negative plain films do not exclude fractures in the craniocervical junction (ie, C1 or C2) or in the cervicothoracic junction, or soft tissue injury in the craniocervical junction, and, in these cases, the liberal use of CT or MR imaging is recommended. MR imaging is recommended also if the patient complains of pain in the setting of negative plain films. MR imaging should be performed also if the patient has symptoms that cannot be explained by the plain film or CT radiologic findings, to evaluate for intraspinal soft tissue injuries, traumatic disc herniations, or cord abnormalities.
Criteria for imaging and choice of imaging modality
One of the critical decisions in the emergency clinical setting is determining which patients require imaging of the spine. Different studies have tried to separate low-risk from high-risk patients . The National Emergency X-Radiology Utilization Study (NEXUS) established five criteria to classify the patients having a low probability of injury . These criteria included no midline cervical tenderness, no focal neurologic deficit, normal alertness, no intoxication, and the absence of a painful distracting injury. The negative predictive value of this tool was 99.8% , but with a low specificity value of only 12%. Other retrospective studies have found the NEXUS low-risk criteria to be less sensitive (92.7%) but to have a higher specificity, 37.8% . Another, perhaps more sensitive or more accurate, method is the Canadian C-spine rule . The Canadian C-spine rule divides patients into high-risk versus low-risk patients, based on the presence of high-risk factors that mandates radiography, or the presence of any low-risk factor that allows the safe assessment of a range of motion. The high-risk factors are 65 or more years of age, dangerous mechanism, or paresthesias in extremities. The low-risk factors include simple rear-end motor vehicle collision, a sitting position in the emergency department, whether the patient has been ambulatory at any time since the trauma, the delayed onset of neck pain, or the absence of midline cervical spine tenderness. In addition, patients in a recent study were evaluated as to whether they were able to rotate their necks 45° to the left and right, by cross-validation, this rule had a 100% sensitivity and a 42.5% specificity for identifying clinically important cervical spine fractures .
The choice of modality depends on several factors, such as the availability of the different imaging modalities, the patient’s clinical and neurologic condition, the type of trauma (blunt, single, or multitrauma), other associated injuries to the brain, thorax, or abdomen, complaints of pain or limited neck or spine motion, the presence of permanent or transient neurologic deficits, and, finally, the reason for the examination (high clinical suspicion of spinal injury versus just a question of excluding injury for legal reasons in a patient with very low suspicion). A special group of patients is composed of those who need spinal cord and spinal canal clearance before surgery, in which case MR imaging is the method of choice.
Negative plain films do not exclude fractures in the craniocervical junction (ie, C1 or C2) or in the cervicothoracic junction, or soft tissue injury in the craniocervical junction, and, in these cases, the liberal use of CT or MR imaging is recommended. MR imaging is recommended also if the patient complains of pain in the setting of negative plain films. MR imaging should be performed also if the patient has symptoms that cannot be explained by the plain film or CT radiologic findings, to evaluate for intraspinal soft tissue injuries, traumatic disc herniations, or cord abnormalities.
Types of injuries
The spine is divided into three osteoligamentous columns: anterior, middle, and posterior. The anterior column includes the anterior longitudinal ligament and the anterior two thirds of the vertebral body and disc, including annulus fibrosus. The components of the middle column are the posterior third of the vertebral body and disc, including annulus fibrosus, and the posterior longitudinal ligament. The posterior column is composed of the pedicles, articular processes, facet capsules, laminae, ligamenta flava, spinous processes, and interspinous ligaments. Depending on the mechanism of injury, several different types of traumatic injuries to the cervical, and the thoracic and lumbar spine, may occur, which may result in stable or unstable spine injuries. The two- or three-column concept was applied initially only to the lower thoracic and lumbar spine but can, with some modifications, be applied also to the cervical spine. Basically, the three-column concept states that fractures affecting more than two of the three columns, or only the middle column, are unstable, and the blunt trauma can be classified therefore by the anatomic location and the biomechanics of the injury.
Several studies have analyzed a more general pattern of spinal injury, and the correlation between type of trauma and type of fracture in the overall population, in the elderly, and in children . Burst fractures are the most common spine injuries after a fall, with 50% located in the thoracolumbar junction, followed by compression fractures . Cervical spine injuries are twice as common in patients older than 70, compared with the nongeriatric population, and odontoid fractures are the most frequent fracture, accounting for 20% of all fractures. In children younger than nine, the most commonly injured level is the higher cervical spine, whereas older children more commonly have injuries to the lower cervical spine .
Cervical spine injuries
Cervical spine injury can be divided simplistically into three major groups, based on the biomechanics behind the injury: hyperflexion injuries, hyperextension injuries, and vertical compression injuries.
Hyperflexion injuries include anterior subluxation, bilateral interfacetal dislocation, simple wedge fracture, clay-shoveller’s fracture (fracture of the spinous process), teardrop fracture, and odontoid (dens) fracture ( Figs. 2–4 ). The bilateral interfacet dislocation and the teardrop fracture are considered unstable. The odontoid fracture can be considered stable or unstable, depending on the fracture type. The remaining injuries are considered stable. The mechanism behind the flexion injury of the cervical and thoracolumbar spine results in forward rotation or translation of the vertebral body and, secondarily, compression in the anterior column with distraction in the posterior column. The injury is caused by forces that cause hyperflexion of the spine in the neutral position, or by a direct trauma to the flexed head and neck. This type of mechanism results in disruption of the posterior and interlaminar ligaments, the facet capsules, and the posterior part of the annulus fibrosus. Hyperflexion fractures often are associated with traumatic disc herniation.
Hyperextension injuries are less frequent than hyperflexion injuries, and usually are the result of an anterior impact to the face, forehead, or mandible, or sudden deceleration as the underlying mechanism. Hyperextension trauma results in the following types of injuries: dislocation, avulsion fracture or fracture of the posterior arch of C1, teardrop fracture of C2, laminar fracture, and the so-called Hangman’s fracture. Most of these injuries, with the exception of Hangman’s fracture, are considered stable. The Hangman’s fracture involves C2 and can be divided into three types, depending on the location of the fracture . Because at least two columns are disrupted in the Hangman’s fracture, this fracture is considered unstable. Hyperextension injuries often are associated with central cord syndrome, in the form of cord edema or diffuse prevertebral soft tissue swelling.
Finally, the Jefferson fracture involves the atlas and is considered unstable. The Jefferson fracture and the burst fracture are caused by vertical compression ( Fig. 5 ). Burst fractures are either stable or unstable, and may cause spinal cord injuries in up to 50% of cases because of encroachment on the spinal canal ( Fig. 6 ). Cusick and Yoganandan presented a more detailed classification of injury and the biomechanisms of injury. The diagnosis of whiplash injury or whiplash-associated disorder is determined by clinical history, the mechanism of injury, and the symptoms and neurologic findings at examination. Whiplash injury is increasingly common and frequently is caused by rear-end motor vehicle accidents, with hyperextension and hyperflexion of the neck. Symptoms include neck pain, neck stiffness, paresthesias, upper extremity pain, jaw pain, and headache. Most imaging techniques in patients who have suspected whiplash injury are inconclusive . The role of imaging in the work-up of patients who have whiplash injury remains controversial and possibly not cost-effective, at least in the acute stage . Most patients report recovery, with a resolution of symptoms. Some whiplash patients do develop chronic neck pain and in these patients who have persistent symptoms, imaging might play a role. A recent study found eight disc herniations in 24 patients who had symptoms for more than 6 weeks after trauma .