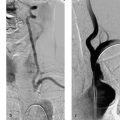
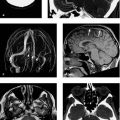
13 Subclavian Steal Syndrome The phenomenon of retrograde blood flow in the vertebral artery relating to an occlusion of the subclavian artery was first described by Contorni in 1960 (Contorni 1960). The term ”subclavian steal” was introduced by Fisher (1961), in an editorial comment on the publication by Reivich et al. (1961). Reivich was the first to describe the neurologic symptoms associated with the subclavian steal phenomenon. The subclavian steal syndrome is a relatively common vascular disorder, with prevalence data in the literature ranging from 0.6 to 6.4%. A 2010 study published by Labropoulus et al. stated a prevalence of 5.4%. Duplex scans of the carotid arteries were performed in 7881 patients over a 6-year period (Labropoulus et al. 2010). It was found that a blood pressure differential of > 20 mmHg between the right and left arms had a high correlation with subclavian steal syndrome. The authors found that subclavian steal was detectable in 77% of patients (n = 254) with a pressure differential of 20–30 mmHg (4.2% of all patients), in 90% of patients (n = 90) with a differential of 31–40 mmHg, and in 100% of patients (n = 85) with a differential of > 41 mmHg. Note Interestingly, it is relatively rare for a detected subclavian steal syndrome to produce clinical symptoms. It is not surprising to find that as the blood pressure differential rises, symptoms become more prevalent. Labropoulus et al. (2010) found that only 1.38% of patients with a pressure differential of 20–30 mmHg had a symptomatic subclavian steal syndrome, whereas 38.5% of patients with a pressure differential > 50 mmHg were symptomatic. The classic manifestations of subclavian steal syndrome are symptoms of vertebrobasilar ischemia such as dizziness and ataxia. Not infrequently, hemispheric symptoms are also found in patients with the syndrome. Atherosclerosis is the most frequent cause of subclavian artery occlusion or stenosis and has an incidence of ~17%. Because atherosclerosis tends to be generalized, associated vascular diseases in the anterior circulation are common and are generally responsible for symptoms. In patients with subclavian steal syndrome and additional vascular diseases in the anterior circulation, Hennerici et al. (1988) found that the 36% incidence of neurologic symptoms fell to 5% following the treatment of anterior circulation disease. Though over two decades old, these figures reflect current epidemiologic data, and clinical symptoms should be very carefully evaluated with regard to their origin before a patient is selected for treatment. Note The severity of symptoms should also be considered as a factor in patient selection. This is emphasized by the study of Labropoulos et al. (2010), who treated only 1.4% of their patients, corresponding to 18.4% of all symptomatic patients. Besides subclavian steal syndrome, an occlusion or high-grade stenosis of the subclavian artery can also lead to angina pectoris with rest and exercise ischemia of the arm or thromboembolism to the arm. Angina pectoris symptoms occur in patients with an internal mammary artery bypass (coronary subclavian steal syndrome). Flow reversal in the bypass graft may occur in the setting of subclavian stenosis or occlusion. Rarely, finger ischemia has also been described as a result of decreased blood flow during exercise (e.g., hand-over-head activities) or thromboemboli from the stenosis. Moreover, arm ischemia may result from a combination of subclavian stenosis and arteriovenous shunts created for hemodialysis, or it may develop in patients with an axillofemoral bypass. There is even a published report of a 74-year-old man with a subclavian stenosis that diverted blood from the anterior spinal artery; this patient presented clinically with bilateral arm weakness (Rughani et al. 2008). Published reports consistently indicate a left-sided predominance. In the epidemiologic study by Labropoulus et al. (2010), the left subclavian artery was affected in 82% of cases; 46% of patients were men 42–86 years old, with an average age of 61 years. Subclavian steal syndrome is not uncommon and is increasingly detected even in asymptomatic patients owing to the widespread use of imaging studies such as duplex sonography, CTA, and MR angiography (MRA). This makes it all the more important to take a discriminating approach to patient selection and not base treatment decisions solely on morphologic findings. The classic clinical manifestations of subclavian steal syndrome include drop attacks, vertigo, and ataxia. Other possible signs are arm ischemia at rest and during exercise or rare symptoms such as angina pectoris in patients who have had bypass surgery (see above). Operative treatment may consist of an axilloaxillary or carotid-axillary bypass or transposing the subclavian artery to the common carotid artery. Perioperative mortality is low, at 0–0.8%, and stroke rates range from 0.5 to 5%. The patency rates published in the 1990s literature are 92–95% at 5 years and 83–85% at 8–10 years. Despite excellent surgical results, the treatment of subclavian steal syndrome during the past decade has been trending toward percutaneous endovascular techniques. Sixt et al. (2009) reported technical success rates of 100% for stenoses and 86% for occlusions. Endovascular treatment is associated with a high procedural success rate, low periprocedural mortality, and good short- and long-term patency rates of 70–90%. Two patients in the 2009 study had periprocedural complications with a pseudoaneurysm at the access site, which was successfully treated by ultrasound-guided compression. Ischemic problems did not occur. The cornerstone for successful endovascular therapy is a complete angiographic survey of the supraaortic vessels to define the true extent of the subclavian steal and the potentially complex collateral pathways. Frequent collateral routes are the occipital artery anastomosis between the external carotid artery and vertebral artery, thyroid artery anastomoses, and intersegmental anastomoses that form rope-ladder connections between the two vertebral arteries. Once the hemodynamics are known, the treatment procedure can be planned and the procedural risk can be assessed. Endovascular treatment may consist of percutaneous balloon angioplasty alone or balloon angioplasty plus stenting. The stent may be of the self-expanding or balloon-expandable type. Caution Self-expanding stents may be disadvantageous for a short circumferential stenosis because the deployed stent may slip to a position that is proximal or distal to the stenosis.
Introduction
Etiology and Clinical Presentation
Indications
Treatment
Operative Treatment
Endovascular Treatment
Imaging Studies
Technique
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree