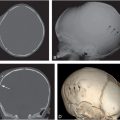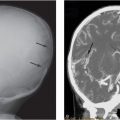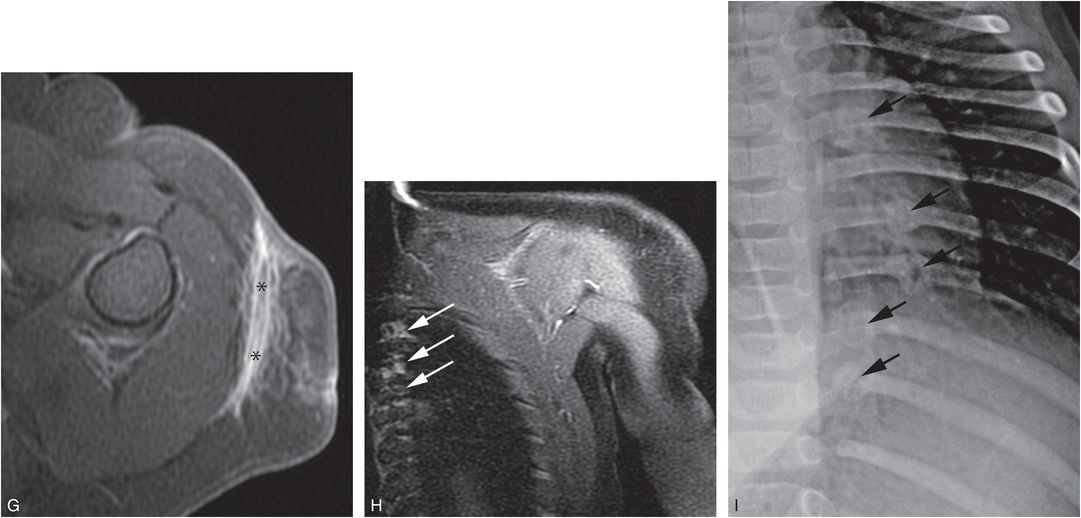
Figure 4.1 Inflicted soft tissue injury simulating neoplasm. A five-month-old infant referred to oncology for a left shoulder mass of several weeks duration. A punch biopsy done elsewhere showed no malignant cells. A, AP radiograph of the shoulder demonstrates an ill-defined deep subcutaneous soft tissue mass (*). B, A coronal sonographic image shows a heterogeneously echogenic subcutaneous mass (*) lateral to the deltoid muscle (D). C, Coronal T1W MRI demonstrates an irregularly marginated mass (*) in the deep subcutaneous fat. D, E, Coronal STIR and axial T2 fat saturated images show corresponding hyperintensity (*). F, Axial T1 FS image shows intermediate signal intensity (*). G, Axial T1 FS post-gadolinium image shows enhancement of the lesion (*) extending to the dermis anteriorly. H, Coronal T1 FS image through the posterior rib cage demonstrates abnormal enhancement at the costovertebral articulations (arrows). I. View of the left ribs from the subsequent SS confirms healing rib fractures (arrows). Other osseous injuries were also noted; see same patient in Fig. 3.95.
The proximal humerus
Normal anatomy
During early infancy, the proximal humeral epiphysis is entirely cartilaginous. The humeral head ossification center is usually present by 4 months of age, and the greater tuberosity appears between 6 and 18 months (34). The two ossification centers and surrounding cartilage move as a unit when physeal injury occurs in young children. Because 80% of humeral growth occurs proximally, injuries affecting the growth mechanism in this region can produce deformity and/or shortening of the extremity, a serious complication that will be subsequently discussed (34).
The junction of the metaphysis with the cartilage of the greater tuberosity is plateau shaped. The lateral cortex often appears to extend beyond the metaphyseal margin, producing a spur-like projection (Fig. 4.2A) (see Chapter 12).
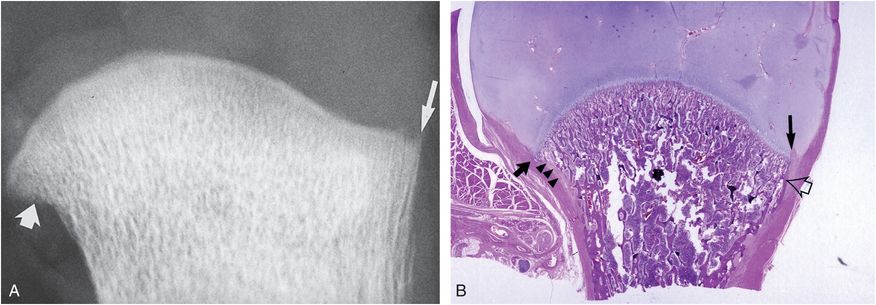
Figure 4.2 Normal humeral anatomy. A, AP specimen radiograph of the humerus of a two-month-old boy shows the physeal margin of metaphysis to be convex medially where it abuts the humeral head, and plateau shaped laterally where it abuts the greater tuberosity. Note the spur of bone extending beyond the metaphyseal margin adjacent to the physeal cartilage (long arrow). Note also the indistinctness of the cortex medially (short arrow). B, A corresponding histologic section shows a prominent lateral SPBC extending beyond the metaphysis and abutting the physeal cartilage, explaining the spur configuration seen radiographically (long black arrow). Medially, a concave margin of humeral neck and a relatively short SPBC produce beak configuration (short black arrow). Note the solid cortex laterally (open arrow) and fenestrated appearance medially (arrowheads). (From Kleinman PK, Marks SC Jr. A regional approach to classic metaphyseal lesions in abused infants: the proximal humerus. AJR. 1996;167:1399–403.)
Histologically, this projection corresponds to the prominent subperiosteal bone collar (SPBC) that extends beyond the chondro-osseous junction (COJ) (Fig. 4.2B). This appearance can be confused with a fracture (35, 36). Medially, the physeal margin of the metaphysis abutting the humeral head has a moderately concave margin that may form a beak-like projection. Histologically, the beak conforms to the junction of the short SPBC and the adjacent medial metaphyseal cortex (Fig. 4.2B) (35, 37–40). In the rapidly growing infant, this medial metaphyseal cortex is fenestrated or absent because of osteoclastic bone resorption and remodeling that exposes the underlying trabeculae of the primary spongiosa (36, 41).
The CML
The CML of the proximal humerus is less common than that involving the lower extremity. Only 1 of 17 metaphyseal “chip” fractures involved the humerus in 28 infants and young toddlers studied by Worlock and associates (14). Loder and Bookout found 19 corner fractures in abused children, only 3 of which involved the proximal humerus (13). Of 124 CMLs found on high-detail SSs in 50 infants, Barber and others found 10 involving the proximal humerus, compared to 35, 29, and 23 affecting the distal femurs, proximal and distal tibias, respectively (21). In the author and colleagues’ postmortem study of 31 abused infants, we found 7 proximal humeral CMLs compared with 15, 17, and 16 lesions of the distal femurs, proximal tibias, and distal tibias (42). However, metaphyseal injuries of the humeri may be more likely to be found incidentally on chest radiography performed for nontraumatic indications. Thus, as with rib fractures, a proximal humeral CML may be the first indication of abuse to be recognized radiographically.
The radiologic features of recent proximal humeral CMLs are often subtle or absent. Histologically, a sharply defined plane of trabecular microfractures extends through the primary spongiosa with hemorrhage and little, if any, evidence of repair (Fig. 4.3; also see Fig. 2.14) (43). When acute/subacute proximal humeral CMLs are inconspicuous on SS, specimen radiography or micro-computed tomography (micro-CT) may demonstrate distinctive findings. More extensive recent injuries will show greater conspicuity with frank osseous disruption and further separation along the fracture plane (see Fig. 2.15) (36, 42).
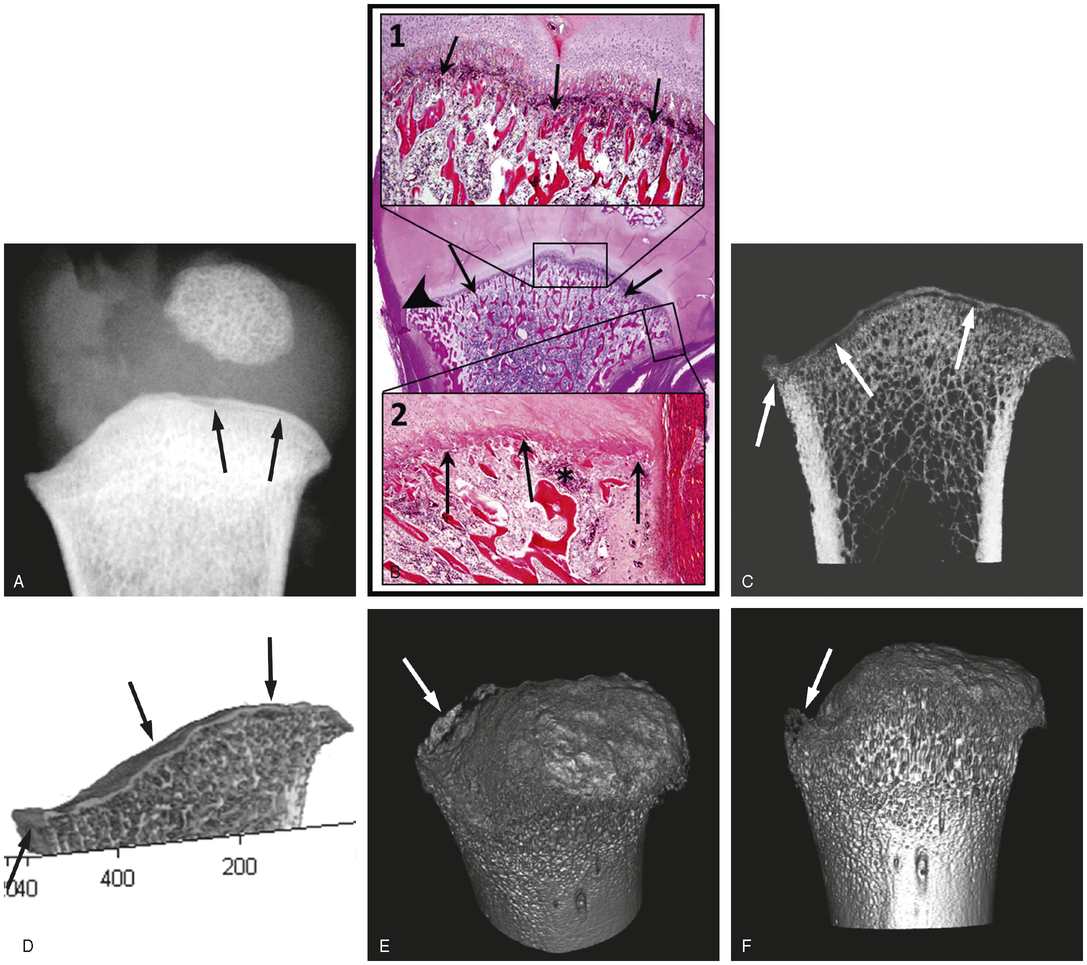
Figure 4.3 CML: subtle imaging alterations in the proximal right humerus of a nine-month-old infant. (See same patient in Figs. 2.6, 2.15.) A, Specimen radiograph shows a lucent line paralleling the metaphysis to advantage (arrows). B, Very low power photomicrograph (center image) demonstrates a fracture line through the medial aspect of the metaphysis extending to the periphery (arrows). Low power (insert 1 at 4.4×) delineates this fracture line (arrows). Medium power (insert 2 at 6.1×) shows that the fracture line (arrows) is less evident than centrally, and a small focus of hemorrhage is present (*). Note that the SPBC is less conspicuous medially than laterally (arrowhead in large image). C, Maximum intensity projection (MIP) image shows both the corner fracture laterally and the fracture line along the region of the COJ (arrows). D, Cross-sectional surface rendering shows the fracture extending in a planar fashion through the region of the COJ towards the periphery where it undercuts a larger fragment that is encompassed by the SPBC (left arrow). The separated disk-like fragment is comprised predominantly of the rZPC (arrows). E, Volumetric rendering shows a bucket handle fracture when the metaphysis is tipped at an obliquity (arrow). F, Volumetric rendering demonstrates the same lesion as a corner fracture pattern when viewed tangentially (arrow). (With permission fromTsai A, McDonald AG, Rosenberg AE, Gupta R, Kleinman PK. High-resolution CT with histopathologic correlates of the classic metaphyseal lesion of infant abuse. Pediatr Radiol. 2014;44(2):124–40.)
With further healing, the radiographic features are better visualized, particularly on specimen radiographs obtained at the time of autopsy. Radiographic indications of fracture tend to be first evident laterally (Fig. 4.4A). A discrete radiolucency disrupts the lateral humeral cortex extending proximally toward the COJ, undercutting a discrete lateral fragment of bone that corresponds to the corner fracture pattern described by Caffey (44). Histologically, this focal lesion shows a plane of trabecular disruption laterally, undercutting the SPBC (Fig. 4.4B) (37, 38, 40, 43, 45–49). As the plane of osseous injury approaches the COJ, an extension of hypertrophic chondrocytes into the metaphysis is often noted (45, 49). These observed findings are commonly focal, and the most important feature of this localized injury is the disruption of the lateral metaphyseal margin.
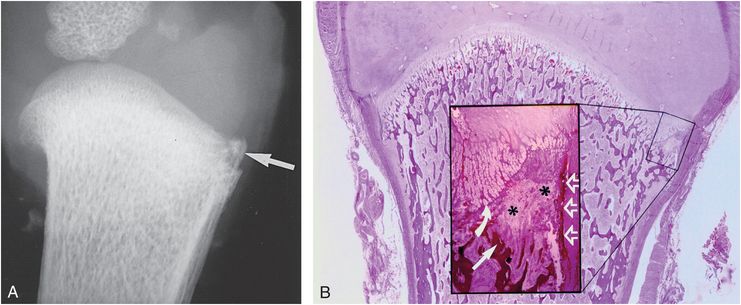
Figure 4.4 Healing focal CML. A, AP specimen radiograph of the proximal left humerus in a 3½-month-old abused infant reveals a corner fracture pattern (arrow). The fracture line disrupts the lateral cortex and extends proximally toward the physis. B, Corresponding photomicrograph shows a healing fracture laterally. The insert shows that the fracture disrupts the primary spongiosa (straight arrow) and undercuts the SPBC (open arrows). Note the thickening and extension of the zone of hypertrophic chondrocytes into the metaphysis (curved arrow), indicating healing. Active bone resorption results in depletion of bony trabeculae at the site of injury (asterisks). (From Kleinman PK, Marks SC Jr. A regional approach to classic metaphyseal lesions in abused infants: the proximal humerus. AJR. 1996;167:1399–403.)
Extensive injuries may demonstrate the lateral fracture line, but they also manifest an osseous injury extending across a substantial cross-sectional area of the metaphysis (Figs. 4.5–4.7). The degree of medial extension of the injury radiographically ranges from a barely perceptible radiolucency (Fig. 4.5A) to grossly abnormal bony architecture (Fig. 4.7A). The more extensive injuries show varying degrees of subphyseal radiolucency and irregular mineralization. Focal, flame-shaped mineralized extensions into the radiolucent physis are a particularly notable finding (Fig. 4.7A). SPNBF is uncommon and generally modest (Fig. 4.7A).
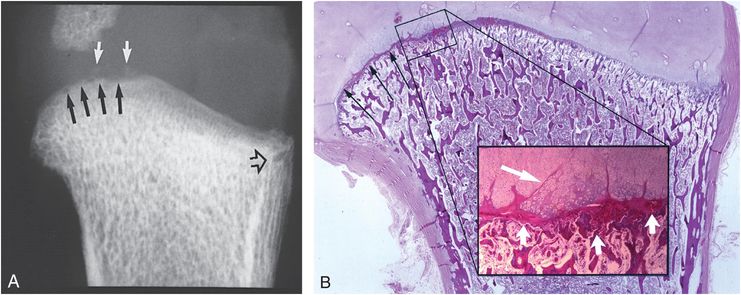
Figure 4.5 Healing of diffuse CML. A, AP specimen radiograph of the proximal left humerus in a five-month-old abused infant reveals a corner fracture pattern laterally (open black arrow). Note the irregularity and loss of normal metaphyseal convexity medially (black arrows). Note also the faint mineralization within the physeal radiolucency (white arrows). B, Corresponding photomicrograph shows a planar fracture extending across the metaphyseal primary spongiosa, meandering into the physeal cartilage medially (long black arrows). The insert shows a plane of disruption extending across the primary spongiosa near the COJ (short white arrows). Multiple fissures extend into the hypertrophic zone (long white arrow). The volume of the hypertrophic zone is increased, which results in irregularity and loss of the convex metaphyseal margin seen in A.
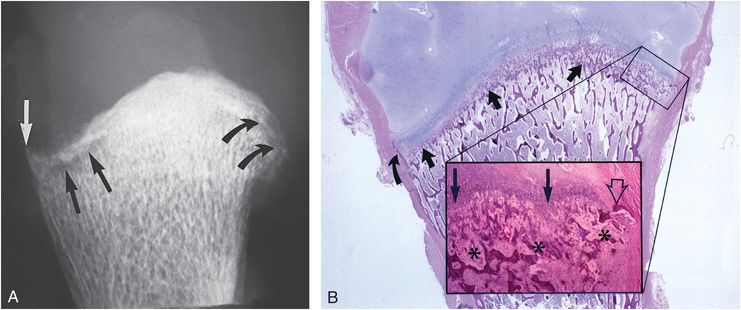
Figure 4.6 Healing diffuse CML. A, AP specimen radiograph of the right humerus in a 3½-month-old abused infant reveals a lucent metaphyseal fracture line (straight black arrows) that undercuts the SPBC, resulting in a conspicuous peripheral fragment laterally (white arrow). Medially, note both the metaphyseal irregularity and the faint fracture line extending through the metaphyseal trabeculae (curved arrows). B, Corresponding photomicrograph shows the plane of injury extending across the primary spongiosa (thick black arrows). The fracture undercuts the SPBC laterally (curved black arrow). The insert shows extensive trabecular disruption (asterisks) and undercutting of the medial SPBC (open arrow). Note the extension of hypertrophic chondrocytes into the disrupted primary spongiosa (long black arrows). (From Kleinman PK, Marks SC Jr. A regional approach to classic metaphyseal lesions in abused infants: the proximal humerus. AJR. 1996;167:1399–403.)
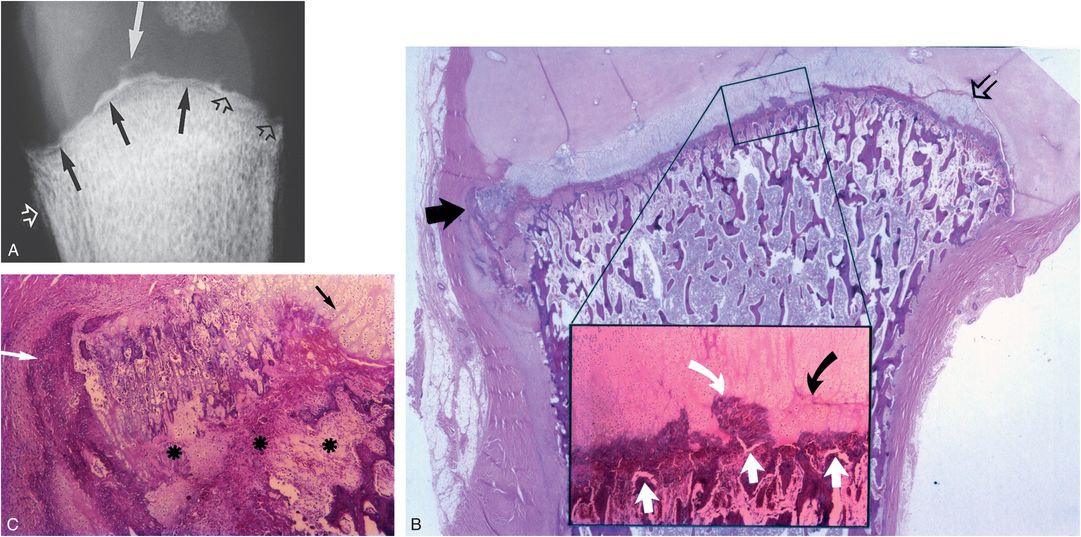
Figure 4.7 Healing CML. A, AP specimen radiograph of the right proximal humerus in a five-month-old abused infant shows a radiolucent fracture line extending across the metaphyseal margin (solid black arrows). Note the irregularity of the metaphyseal margin with focal radiolucent extensions into the metaphysis (open black arrows), and peninsulas of mineralized densities (solid white arrow) within the physis. SPNBF (open white arrow) is present laterally. B, Corresponding photomicrograph shows a planar injury traversing the metaphyseal primary spongiosa. Laterally, the fracture undercuts the SPBC (solid black arrow). Medially, the fracture meanders into the physeal cartilage (open black arrow). The insert shows the fracture extending across the primary spongiosa (white arrows). A peninsula of bone/calcified cartilage (curved white arrow) is surrounded by hypertrophic chondrocytes. The cleavage plane is evident through the thickened hypertrophic chondrocyte zone (curved black arrow), a finding that suggests a second more recent injury. C, Photomicrograph of the region indicated by the solid black arrow in B shows widespread depletion of trabeculae, granulation tissue, and osteoclastic activity (*). The fracture undercuts the SPBC (white arrow). Hypertrophic chondrocytes extend into the fracture site (black arrow).
Histologically, the laterally situated findings are similar to those noted in the focal lesion where the fracture line undercuts SPBC (Figs. 4.5B, 4.6B, 4.7B,C). However, the plane of injury extends to varying degrees along the primary spongiosa, with trabecular disruption and osseous repair. Diffuse thickening of the zone of hypertrophic chondrocytes is usually seen in the region of osseous injury. Focally, areas of primary spongiosa may be surrounded by the thickened hypertrophic chondrocytes of the physis, findings that appear to correspond radiographically to the flame-shaped mineralized densities (Fig. 4.7C). Vertical fissures extending from the fracture line into the physeal cartilage are other interesting histologic findings (Fig. 4.5B).
The major proximal humeral CML patterns are depicted diagrammatically in Figure 4.8. The bucket handle pattern, commonly encountered in the lower extremity, is only occasionally noted in the proximal humerus (50). The factors responsible for the corner fracture and bucket handle patterns in the proximal humerus are well shown using three-dimensional (3D) micro-CT (Fig. 4.3C–F).
Figure 4.8 Proximal humeral CML. Right, focal lesion; left, extensive lesion. The fracture extends through the primary spongiosa. In the periphery, the fracture line (arrows) undercuts the SPBC. When the lesion is focal, it results in a corner fracture appearance laterally (right). When it is more extensive, diffuse metaphyseal lucency and irregularity result (left).
Although the proximal humeral CML is a primarily osseous lesion, passage of the fracture line into the hypertrophic cartilage zone is commonly noted histologically (Figs. 4.5–4.7) (42). This finding contrasts with the relatively uncommon intrusion of the fracture line into the physis noted in most other metaphyses. The proximal humerus is a well-described site for epiphyseal separations of the Salter–Harris (SH) type (see below) (51). And as will be discussed, these relatively rare injuries form a continuum with the common CML fracture patterns.
In contrast to other sites, such as the distal tibia, where metaphyseal injuries have a fairly predictable radiographic appearance, the injuries of the proximal humerus are varied. As noted, radiographic studies may be normal initially, despite significant pathologic changes. A follow-up SS in two weeks will demonstrate definite abnormalities (Fig. 4.9) (46).
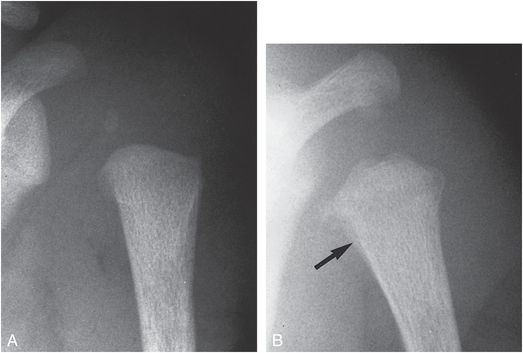
Figure 4.9 Proximal humeral CML, showing the value of follow-up study. A, AP view of the proximal humerus in a two-week-old abused infant is normal. B, Follow-up radiograph taken two weeks later shows metaphyseal irregularity and radiolucency, with SPNBF medially (arrow).
Commonly, the proximal humeral CML is manifested initially as an area of subphyseal radiolucency, a nonspecific finding that can be noted in other disorders (see Chapters 7 and 12). However, when this radiolucency is a unilateral finding or when it is associated with a distinctive CML in the opposite extremity, the pattern likely indicates a fracture (Fig. 4.10). With healing, the radiolucency migrates from the physis as new trabecular bone is laid down at the COJ. With repetitive injury, dense sclerosis can be seen about the fracture margins (Fig. 4.11). The fracture may be associated with other injuries around the shoulder girdle, including the acromion (Fig. 4.11), clavicle, and upper ribs (see Chapter 5).
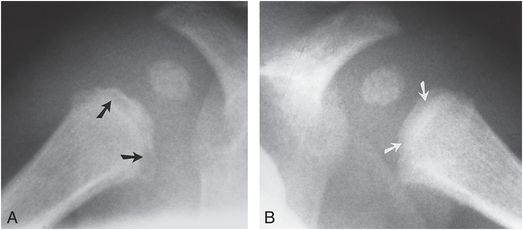
Figure 4.10 Bilateral proximal humeral CMLs. Right (A) and left (B) proximal humeral metaphyseal lucencies are seen in this abused infant (arrows). Sclerosis and irregularity, indicating chronicity, are more pronounced on the right.
Figure 4.11 Proximal humeral CML, advanced healing. AP view of the right shoulder in a three-month-old abused infant demonstrates a transmetaphyseal radiolucency of the proximal humerus (large arrows). Dense sclerosis indicates healing and probable repetitive injury. Note also an accompanying acromial fracture (small arrows). (Courtesy of Michael Thomason MD.)
Physeal injuries and epiphyseal separations
Although the humerus is commonly fractured with abuse, separation of the proximal humeral epiphysis is relatively rare (21, 50, 52). Although Pandya et al. found that the humeral fractures in 10 of 36 children were proximal in location, they did not specifically mention proximal epiphyseal separations or SH-type injuries (27). Large studies including substantial numbers of humeral fractures, and smaller series focusing on humeral fractures, do not describe proximal humeral epiphyseal separations (18, 23, 24).
The morphologic characteristics of an inflicted epiphyseal separation are identical to those resulting from obstetric injury (see Chapter 11). Numerous examples of birth-related epiphyseal separations of the proximal humerus have been described, and an examination of the mechanics and anatomic alterations in these cases sheds light on the injury associated with abuse (30, 31, 53). The birth injury occurs as the upper extremity is twisted and pulled with an armling presentation and extraction. A breech presentation, with excessive manipulation of the arms during delivery, may also result in epiphyseal separations. These tractional, torsional, and other complex stresses occurring during delivery are likely similar to the forces applied during manual assaults on infants and toddlers.
Radiographically, early diagnosis of a proximal humeral epiphyseal separation can pose a significant challenge if the epiphysis is unossified, or if there is no displacement of an ossified epiphysis. Furthermore, since the unique anatomy of the shoulder joint permits a wide range of motions of the humeral head with respect to the glenoid, the radiographic patterns of humeral epiphyseal separations are dependent on the position in which the shoulder is held, as well as the direction of displacement. In most cases, the metaphysis is displaced laterally with respect to the epiphysis, but this may be inapparent on a single projection. A clue to the injury may be a subtle metaphyseal fragment suggesting a SH type II fracture pattern (Fig. 4.12). With severe displacement, the metaphysis will lie lateral and cephalad with respect to the glenoid (Fig. 4.13).
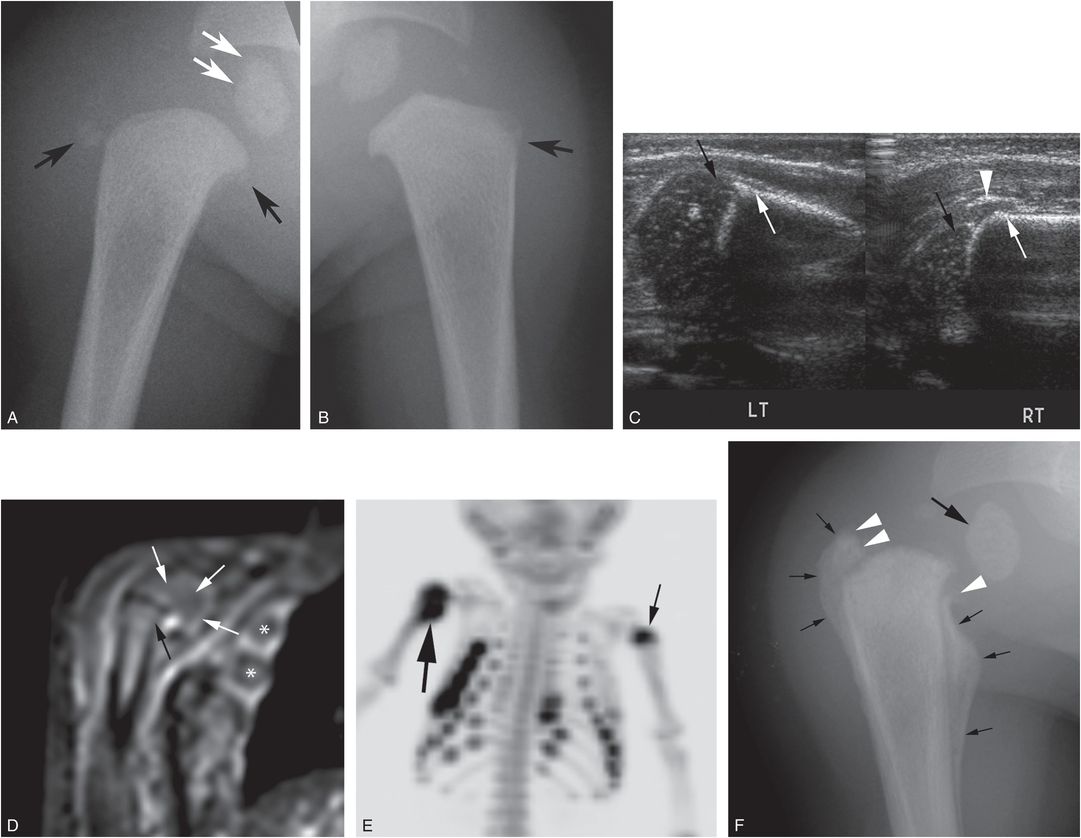
Figure 4.12 Proximal humeral epiphyseal separation. A four-month-old boy with multiple bruises. (See same patient in Fig. 3.105.) A, AP radiograph of the right shoulder shows small mineralized densities arising from the proximal humeral metaphysis (black arrows). The metaphysis is displaced slightly laterally with respect to the humeral head ossification center (white arrows), consistent with an epiphyseal separation. Compare with the appearance on the left (B). C, Coronal sonograms of the right (RT) proximal humerus with comparison of left (LT) demonstrates a lateral shift of the right proximal humeral metaphysis (white arrows) with respect to epiphysis (black arrows). An echogenic band extends from the periosteum correlating with the mineralized density in A (arrowhead). This is due to early SPNBF and/or a bony metaphyseal fragment. D, Coronal STIR sequence from the WB-MRI shows similar metaphyseal displacement (black arrow) with respect to the epiphysis (white arrows). Also note signal fluid around several ribs (*). E, Anterior MIP 18F-NaF PET study shows intense abnormal uptake in the right proximal humerus (thick arrow) consistent with a physeal injury. Additionally, there is mildly increased tracer uptake in the left proximal humeral metaphysis (thin arrow), correlating with a subtle CML (arrow in B), not initially noted. There are multiple rib fractures, correlating with the MRI findings. F, Three-week follow-up radiograph of the right shoulder shows further displacement of the metaphysis with respect to the epiphysis (thick arrow) and marked callus formation (thin arrows) indicating an epiphyseal separation. Note discontinuity of the SPNBF with the epiphysis (arrowheads) indicating disruption of the periosteum. (A, B, E, and F published with permission from Drubach LA, Sapp MV, Laffin S, Kleinman PK. Fluorine-18 NaF PET imaging of child abuse. Pediatr Radiol. 2008;38(7):776–9.)
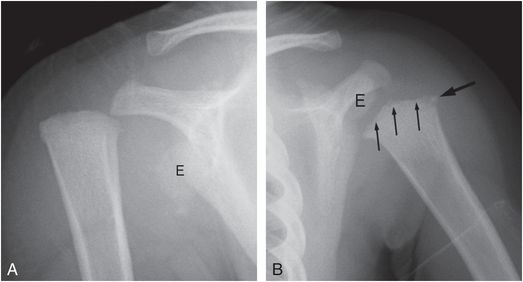
Figure 4.13 Proximal humeral epiphyseal separation with severe displacement. An 18-month-old child with right shoulder injury and reported fall from a standing position onto an outstretched arm. A, AP view of the right shoulder demonstrates lateral and superior displacement of the proximal humeral metaphysis with respect to the scapula. The ossified proximal humeral epiphysis (E) remains associated with the glenoid, although somewhat inferior in position. B, AP view of the left shoulder shows a proximal humeral CML with a lateral corner fracture pattern (thick arrow) and subphyseal metaphyseal irregularity (thin arrows). In contrast to the right, the relationship of the epiphysis (E) to the metaphysis is normal. (Case courtesy of Carole Jenny MD.)
If the epiphysis is unossified, or if the ossified epiphysis is obscured by overlying structure, the appearance may suggest a shoulder dislocation. Pure glenohumeral dislocations are rare in infants and early childhood, and this pattern should be assumed to be a physeal injury with epiphyseal separation. In very rare instances, the metaphysis may be shifted medially with respect to the epiphysis (Fig. 4.14) (54). The humeral head may appear to be perched over the apex of the metaphyseal margin (Fig. 4.14A). A posteroanterior (PA) chest radiograph taken with the arms elevated in the routine fashion may cause superimposition of the displaced proximal humeral ossification center over the metaphysis and result in apparent absence of the proximal humeral epiphysis (Fig. 4.14B).
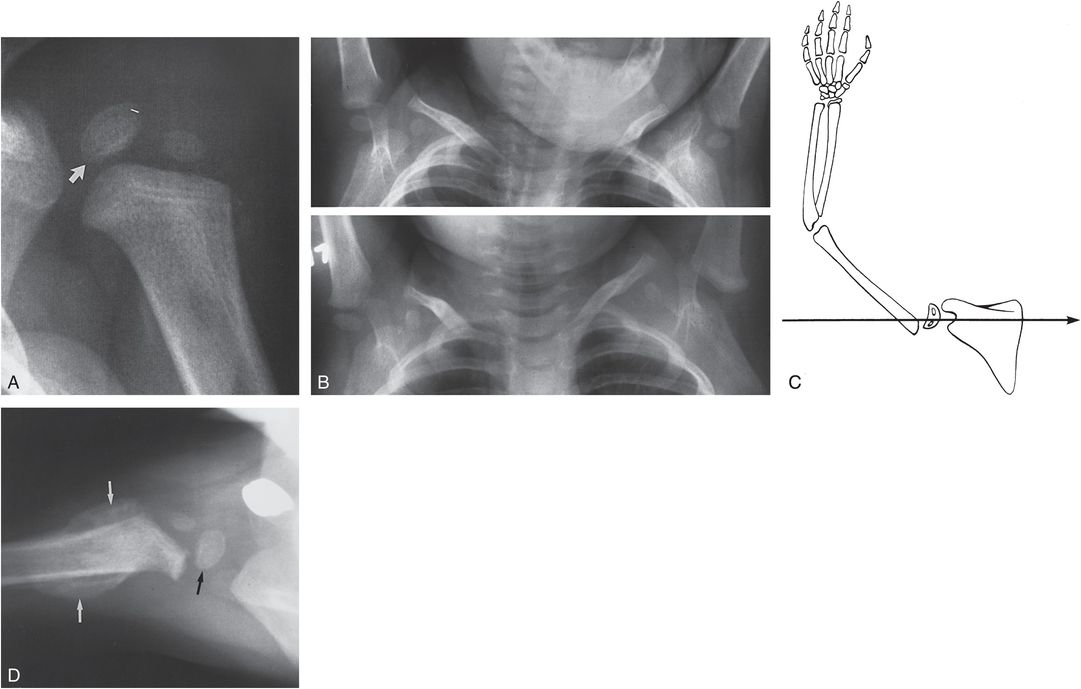
Figure 4.14 Displaced SH type I fracture of the proximal humerus in an 18-month-old child. The mother indicated that she had pulled the child’s left forearm, producing sudden forward flexion at the shoulder. A, An external rotation view of the shoulder demonstrates lateral displacement of the ossification centers of the humeral head (arrow) and greater tuberosity. B, Lower frame, The upper portion of a chest film obtained at admission demonstrates apparent absence of the left proximal humeral epiphysis. Upper frame, A chest film obtained six months earlier shows a normal proximal humeral ossification center. C, This injury occurs by sudden forward flexion of the shoulder, resulting in anterior slippage of the epiphysis. The projection of the beam with a standard chest film (arrow) causes superimposition of the humeral head over the metaphysis, resulting in “absence” of the ossification centers. D, A follow-up film two weeks after admission in the axillary projection demonstrates epiphyseal displacement (black arrow) and SPNBF (white arrows). (From Kleinman PK, Akins CM. The “vanishing” epiphysis: sign of Salter type I fracture of the proximal humerus in infancy. Br J Radiol. 1982;55:865–7.)
The early literature promoted arthrographic assessment, but sonography has simplified the prompt diagnosis of proximal humeral epiphyseal separation (Fig. 4.12C) (31, 52). Considerable sonographic experience has been accumulated with obstetrically induced proximal humeral epiphyseal separations (see Chapter 11). Since the structures of interest lie within a few millimeters of the skin, the precise relationships of the epiphysis to the metaphysis can be defined and compared to the opposite side. Early periosteal stripping and SPNBF are easily identified. Magnetic resonance imaging (MRI) is usually unnecessary, but may be performed when the shoulder is swollen and infection is suspected. The injury may also be encountered and elucidated when whole-body MRI (WB-MRI) is done for global skeletal assessment of suspected abuse (Fig. 4.12D).
Diagnosis is generally apparent when healing is present and the character of the SPNBF delineates the extent of epiphyseal displacement (Fig. 4.12F). If the periosteum remains firmly anchored to the physeal region, the new bone formation will converge on the metaphyseal margin (Fig. 4.14). If it has been torn from its attachment, the SPNBF will tend to end abruptly in the nearby soft tissue (Figs. 4.15, 4.16; also see Fig. 4.12).
Figure 4.15 Proximal humeral epiphyseal separation, showing healing. AP view of the left shoulder in a two-year-old abused child shows a relatively normal relationship of the proximal humeral epiphysis and the metaphysis. However, there is extensive subphyseal radiolucency (black arrows) and extensive SPNBF (white arrows). The configuration of the laterally situated subperiosteal new bone implies stripping and lateral displacement of the periosteum, presumptive evidence of SH type I physeal injury and epiphyseal separation.
Figure 4.16 Proximal humeral epiphyseal separation. AP view of the right shoulder in an abused infant shows the humeral metaphysis to be severely displaced (white arrows). There is massive SPNBF that ends abruptly in the medial soft tissues (black arrow). Note the healing rib fractures.
Nicastro and Adair reported a unique example of a fracture-dislocation of the shoulder in a 32-month-old child with suspected abuse (Fig. 4.17) (55). The epiphysis was “buttonholed” anteriorly through the capsule, lying in a subglenoid location. The metaphysis was displaced superolaterally. An open reduction with internal fixation was performed with excellent results.
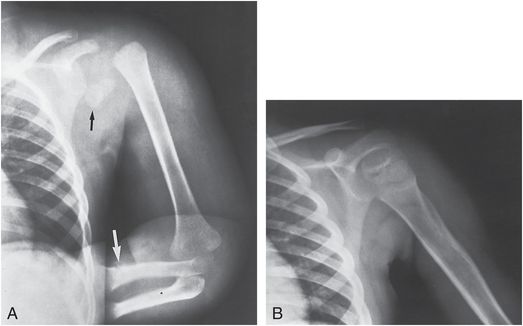
Figure 4.17 Fracture-dislocation of the proximal humerus. A, AP view of the upper extremity in a 32-month-old child suspected of being abused shows separation of the humeral metaphysis from the proximal epiphysis, which is dislocated anteriorly to a subglenoid position (black arrow). There is also a distal radial fracture (white arrow) as well as a distal clavicle fracture. B, Excellent results were achieved after open reduction and internal fixation. (From Nicastro JF, Adair DM. Fracture-dislocation of the shoulder in a 32-month-old child. J Pediatr Orthop. 1982;2:427–9.)
Although these injuries have a remarkable capacity to heal and remodel despite impressive epiphyseal displacement, disruption of the growth mechanism may lead to severe deformity. Figure 4.18 illustrates the consequences of an early physeal injury which led to a medial physeal growth arrest with consequent humeral shortening and lateral bowing. In such cases, MRI is useful in preoperative planning. Physeal bridging may be inconspicuous or absent, but the orientation of the physis, with shortening and irregularity of the adjacent metaphyseal cortex, indicates a periphyseal growth disturbance.
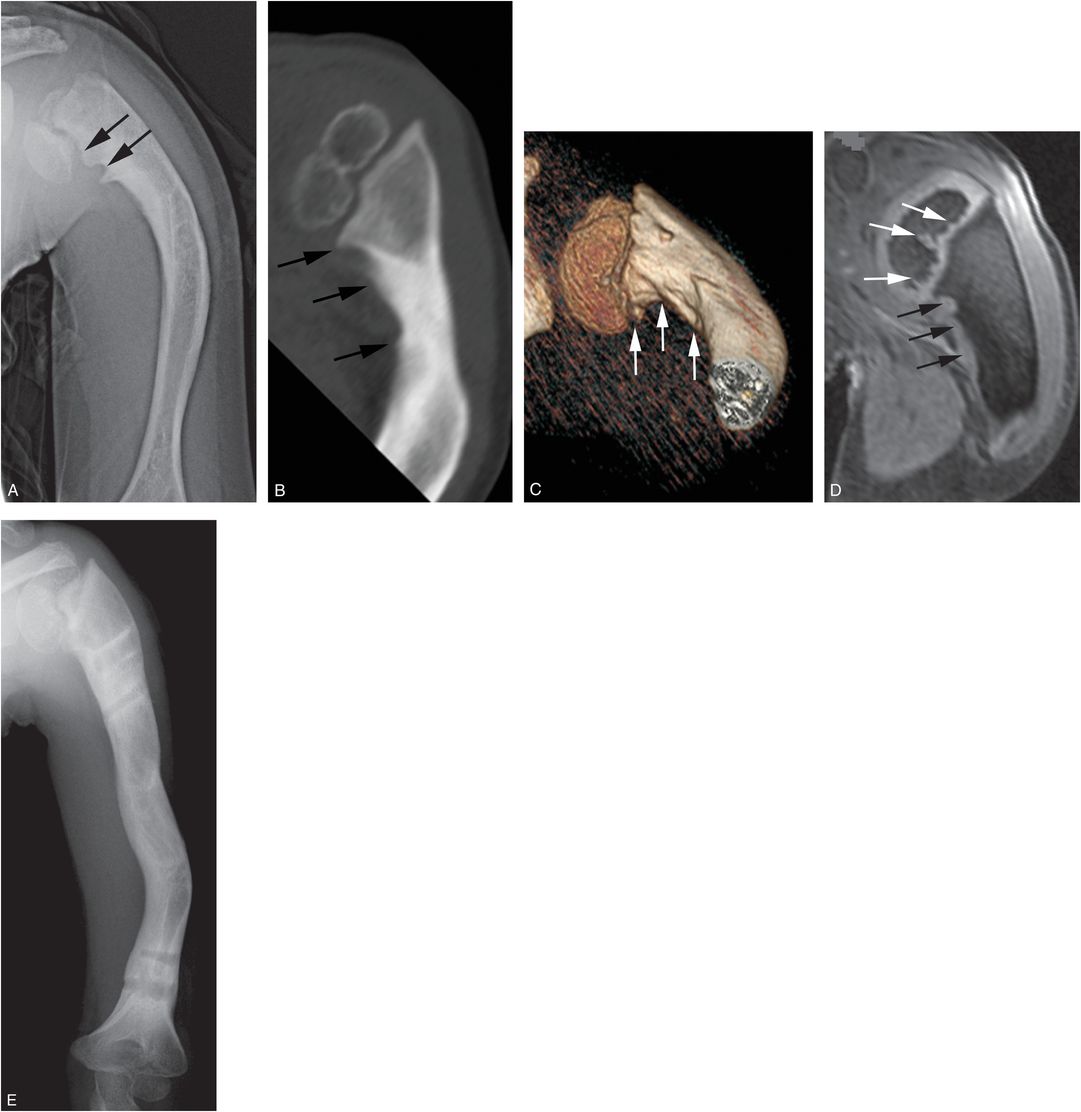
Figure 4.18 Proximal humeral physeal growth disturbance. A 3-year-old child who had presented at 14 months of age with a skull fracture, multiple extremity injuries, and FTT. Progressive shortening of the left arm was noted at 2½ years of age. A, AP radiograph of the left humerus demonstrates a short laterally bowed humerus. Proximal humeral physeal/metaphyseal irregularity is evident medially (arrows), with associated varus deformity. B, Coronal oblique CT reformat at four years of age shows deformity of the proximal humeral epiphysis, varus deformity of the neck, and irregularity of the medial humeral metaphysis (arrows). C, 3D model shows the physeal and metaphyseal changes (arrows) to advantage. D, Coronal oblique 3D SPGR FS reformat at age five years shows gross patency of the physis, but there is irregularity along the base of the epiphysis (white arrows) suggesting a physeal growth disturbance. There is a scalloped appearance of the medial humeral metaphysis associated with hyperintense tissue (black arrows), possibly reflecting bridging cartilage. E, At age 11 years, following osteotomies and lengthening, bowing is reduced but varus deformity persists.
Although the typical CML and proximal humeral epiphyseal separation have distinctive radiologic and pathologic features, an intermediate injury occurs. We noted focal intrusion of the metaphyseal fracture line into the zone of hypertrophic chondrocytes in half of the proximal humeral CMLs studied pathologically (36). The findings point to a continuum between the CML and the epiphyseal separation of the proximal humerus. This is nicely demonstrated in Figs. 4.12 and 4.13 where an epiphyseal separation on the right was accompanied by a proximal humeral CML on the left. Although the mechanisms of injury may vary, the degree of force required for epiphyseal separation is likely greater than that causing the CML. It is reasonable to assume that the tractional and torsional forces applied during most infant assaults result in a mainly osseous injury without significant epiphyseal displacement. When more severe forces are entailed, a primarily cartilaginous injury with epiphyseal separation results. In some instances, differentiation of a CML from a nondisplaced SH type I fracture of the proximal humerus on radiographic grounds is impossible.
Proximal humeral metaphysis
Nonspecific proximal humeral metaphyseal fractures may be grossly displaced, angulated, or comminuted with overlying soft tissue swelling (Fig. 4.19). Exuberant callus is often evident in the healing phase. An apparent transverse metaphyseal fracture may be associated with extension to the physis with physeal irregularity, displaying features of both a SH type II injury and a CML pattern (Fig. 4.20; also see tibial injuries in Figs. 3.84, 3.87). These proximal injuries, as well as more distally situated humeral fractures are on occasion associated with forearm and hand injuries (Figs. 4.19, 4.20).

Figure 4.19 Proximal humeral metaphyseal fracture with multiple upper extremity injuries. A one-year-old boy not moving his left arm. (See same patient in Figs. 3.15, 3.69, 5.40, 17.13.) SS showed multiple extremity, rib, clavicle, and skull fractures. A, AP view of the left humerus demonstrates a transverse comminuted fracture of the proximal humeral metaphysis with early callus formation. There is also cortical disruption of the supracondylar region (arrow). B, Oblique view of the left forearm shows transverse fractures of the midshafts of the radius and ulna (thick arrows). There is early SPNBF along the ulnar fracture site (thin arrows) and along the supracondylar fracture (arrowheads). C, Anterior MIP of the upper body from the 18F-NaF PET study shows intense uptake corresponding to the left proximal humeral fracture with abnormal activity in the left supracondylar region (arrowhead) and forearm bones (thin arrows). There is also a left clavicular fracture (thick arrow). Note subtle increase uptake in the right distal ulnar metaphysis (open arrow). D, Frontal view of the right ulna shows faint SPNBF corresponding to the scintigraphic finding (open arrows). E, One month later there is exuberant callus around the proximal humeral fracture. F, Frontal view of the left elbow and forearm shows further callus about the forearm fractures (thick arrows) and a healing supracondylar fracture with robust callus (thin arrows).

Figure 4.20 Proximal humeral metaphyseal fracture with other upper extremity injuries of varying ages. A nine-month-old infant with history of a fall three days earlier and an unwillingness to bear weight on the right leg. (See same patient in Fig. 3.97.) SS revealed multiple fractures. A, Anterior MIP of the humerus from the 18F-NaF PET study shows intense uptake in the left proximal humerus (thick arrow). Mild increased activity is also evident in the mid/distal humeral shaft (arrowhead). Note rib fractures. B, AP view of the left humerus shows an irregular transverse fracture (thick black arrows) of the proximal metaphysis with surrounding SPNBF (thin black arrows). There is extension of the fracture to the physis (thick white arrow) and associated physeal irregularity (thin white arrows), with features of both a SH type II injury and a CML. There are no findings corresponding to the distal humeral abnormality in A. C, Frontal view of the left forearm demonstrates sclerosis in the distal radial metaphysis consistent with a healing fracture (arrow). D, Frontal view of the right forearm shows a buckle fracture of the distal radial metaphysis (arrow). E, F, Oblique views of the left and right hand show SPNBF along the proximal shaft of the proximal phalanx of the left fifth digit (arrow) and along the right second metacarpal (arrow) indicating healing injuries. G, Two-week follow-up of the left humerus shows further healing of the proximal fracture. Note that the physeal irregularity has resolved. SPNBF (arrows) is now evident corresponding to the region of increased scintigraphic activity in A. The findings indicate injuries occurring in at least two time frames.
Buckle fractures can be quite subtle, and radiography may be inconclusive, despite straightforward histopathologic findings at autopsy (Fig. 4.21). In fact, there may be histologic evidence of extension of the injury to the physis, which is inapparent, even on specimen radiography. Buckle fractures of the proximal humeral metaphysis may be accompanied by more significant distal humeral and forearm injuries (Fig. 4.21; also see Fig. 4.36). On occasion it may be difficult to differentiate a simple metaphyseal fracture from a SH type II injury, which extends to the physis (Fig. 4.21).
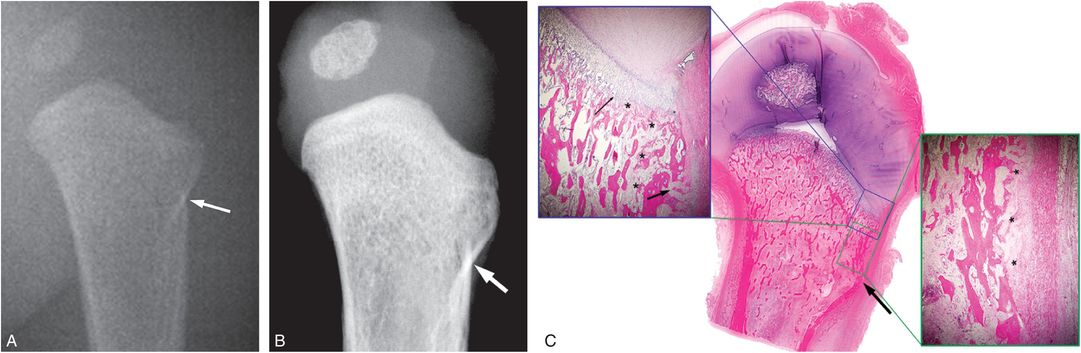
Figure 4.21 Proximal humeral buckle fracture with pathologic correlation. A five-month-old infant with a fatal head injury. (See same patient in Figs. 2.11, 3.78, 3.87, 4.29, 4.42.) A, AP view of the left humerus from the postmortem SS shows a subtle buckle fracture (arrow). B, Specimen radiograph shows metaphyseal cortical discontinuity laterally (arrow). C, Very low power histologic section shows corresponding cortical deformity. Higher power image (lower insert) shows early SPNBF (*). Proximally (upper insert), there is a cortical defect (thick arrow), as well as trabecular disruption and early repair extending to the physis (*). Note focal increase in the hypertrophic chondrocyte zone (thin arrow).
The humeral shaft
Most humeral fractures in abused children involve the shaft. Even in early infancy, where metaphyseal lesions may be more common, humeral shaft fractures constitute a large proportion of humeral injuries (8, 13, 14, 17, 18, 22, 23, 28, 56, 57). Fractures tend to involve the middle and distal thirds of the shaft (27). Most fractures are of the spiral or oblique variety and occur with torsional forces as the arm is twisted. As with nondisplaced shaft fractures at other sites, the fracture line may be absent or inconspicuous on one view and well demonstrated on others (Fig. 4.22). For this reason, Karmazyn and others have advocated the addition of lateral views to the customary frontal projection of the long bones in the routine SS (57). Strait and colleagues found that all seven of the inflicted diaphyseal fractures in their study were of the oblique or spiral variety (23, 25). However, transverse fractures do occur, particularly in young infants (Fig. 4.23, see Fig. 4.25). Although transverse humeral fractures occasionally occur from blunt impact (58), it is likely that most result from indirect forces. Grabbing the infant by the forearm and/or elbow and applying a bending force can result in a distraction/compression injury just above the gripping hand. Typically, the fracture is angulated, with separation of the fragments along one margin and impaction along the other (Fig. 4.23).
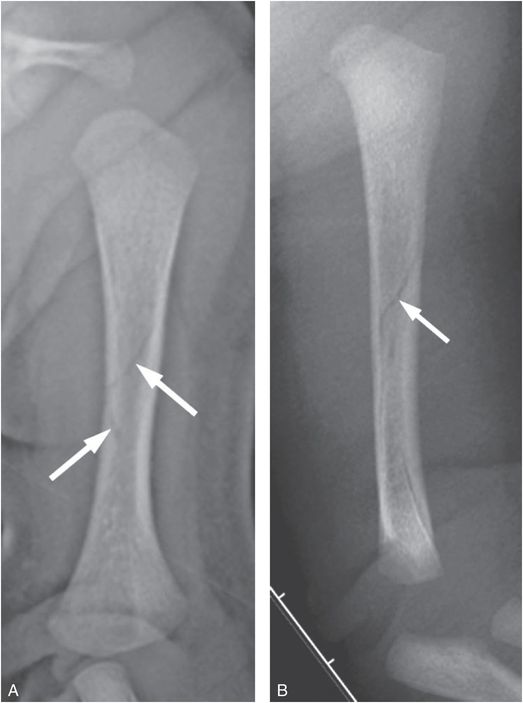
Figure 4.22 Nondisplaced humeral spiral fracture. A 16-day-old infant not moving left arm 1 day after parent reportedly heard a snap upon forcefully trying to pull the infant’s left arm through a jacket sleeve. A, AP radiograph shows a vague spiral lucency in the mid diaphysis (arrows). B, Lateral radiograph confirms a nondisplaced midshaft humeral spiral fracture (arrow). SS revealed a right proximal tibial CML.
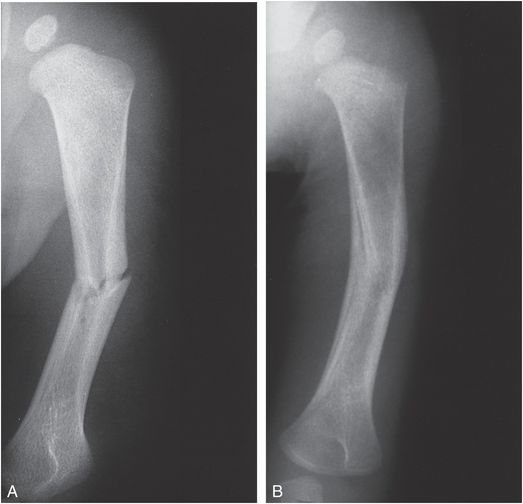
Figure 4.23 Transverse humeral shaft fracture with follow-up. A, AP view of the humerus in a six-month-old abused infant demonstrates an irregular transverse fracture with varus angulation of the distal fragment. The infant was in a high chair and the assailant grabbed and twisted the child’s arm. B, Repeat study 2½ months later shows advanced healing and remodeling.
Bone scintigraphy may be performed acutely, and despite impressive radiographic findings, a recent humeral shaft fracture may produce only diffuse increased activity along the entire shaft, without focal increased uptake at the fracture site (Fig. 4.24). In other instances, scintigraphy may demonstrate increased uptake acutely in the humeral shaft in the absence of radiographic findings (see Fig. 4.20).

Figure 4.24 Humeral fracture with diffuse uptake on scintigraphy. A three-week-old infant not moving arm with no history of trauma. A, AP view of the right humerus done elsewhere shows an oblique mid-shaft humeral fracture (arrow) B, Anterior MIP of the upper extremities and chest from the 18F-NaF PET study shows diffuse increased uptake in the right humeral shaft (arrow) and focal uptake at the site of multiple left-sided rib fractures confirmed at SS.
Shaft fractures in infancy heal relatively rapidly with variable callus and remarkable remodeling (Figs. 4.23, 4.25). SPNBF reflecting repair may occur along the humeral shaft. Although it can be difficult to distinguish this from normal physiologic new bone, a thick diffuse and rapidly evolving pattern suggests a traumatic etiology (Fig. 4.25). Despite swelling, deformity, and obvious discomfort, these injuries can be neglected and may be detected only if the child undergoes subsequent radiologic investigations. Untreated healing displaced and angulated humeral shaft fractures may demonstrate a lucent band extending through a thick circumferential zone of callus/SPNBF (Fig. 4.26). This may suggest a refracture of a prior healing injury, but the absence of acute soft tissue swelling is more in keeping with the well-known pattern of extension of the fracture lucency through robust callus in persistently mobile untreated fractures (Fig. 4.26). Deep soft tissues changes surrounding the fracture, without more superficial signal abnormality on MRI, suggest a single healing injury with delayed union.
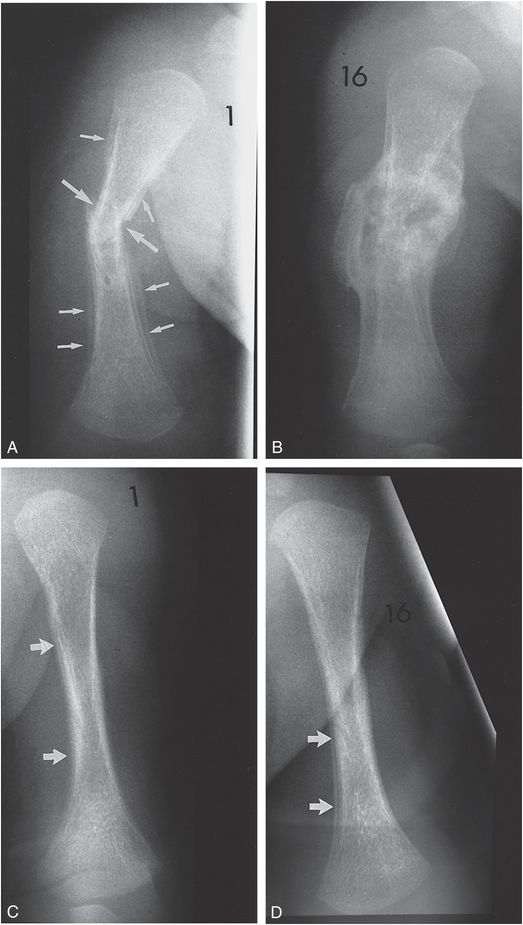
Figure 4.25 Transverse humeral shaft fracture and contralateral SPNBF. A, AP view of the right humerus in a two-month-old former premature infant shows a transverse fracture of the middle one-third of the diaphysis of the humerus (large arrows). The fracture is associated with a moderate amount of SPNBF (small arrows). B, A follow-up study 16 days later demonstrates striking maturation of SPNBF and callus that bridge the fracture site. C, AP view of the left humerus demonstrates indistinct cortices with SPNBF most evident medially (arrows). D, A follow-up study 16 days later demonstrates further organization of subperiosteal new bone (arrows), likely of a traumatic origin.
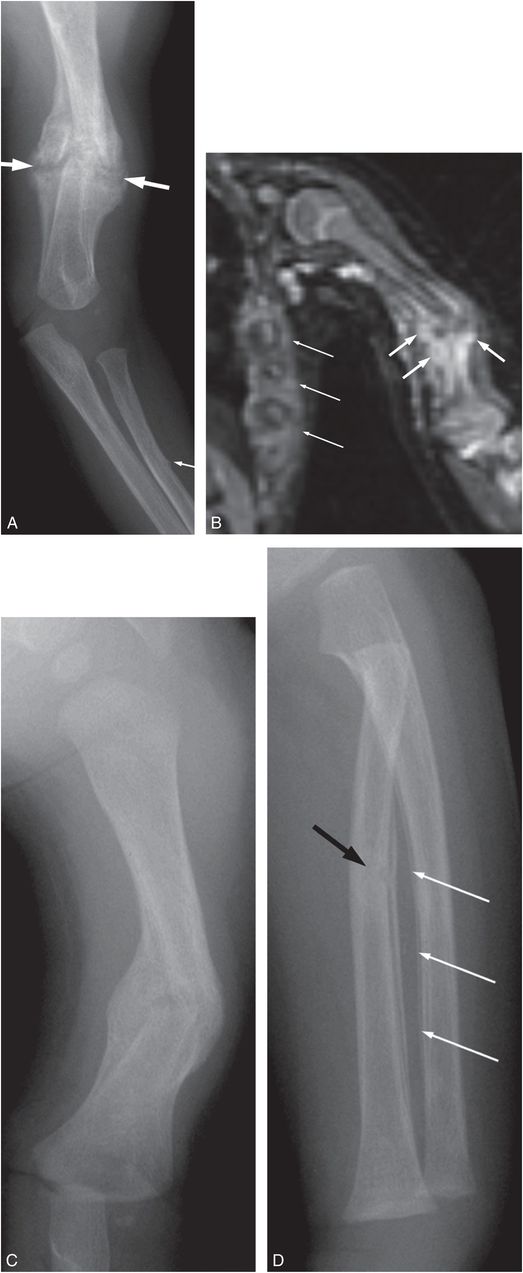
Figure 4.26 Healing humeral fracture with fracture lucency extending through callus. A three-month-old infant transferred with widespread skeletal injuries. (See same patient in Fig. 3.14.) A, Initial frontal view of the left humerus and forearm demonstrates an angulated transverse midshaft left humeral fracture with mature callus (thick arrows). Note that the fracture lucency extends through the callus, more consistent with motion at the fracture site, than a superimposed acute injury. There is a buckle fracture of the radius without healing (thin arrow). B, Coronal WB-MRI shows deep soft tissue hyperintensity (thick arrows) concentrated around the humeral fracture. Also note hyperintensity around multiple rib fractures (thin arrows) confirmed radiographically. C, AP radiograph three weeks later shows firm bridging around the fracture with persistent angular deformity. D, Oblique view of the left forearm now shows healing of the radial fracture (black arrow) as well as SPNBF along the adjacent ulnar shaft (white arrows).
The distal humerus
The unique anatomic structure of the growing distal humerus determines the varied radiographic appearances of injuries involving the metaphyseal–epiphyseal complex. Consequently, the stage of epiphyseal ossification influences the imaging features evident radiographically and with cross-sectional imaging. The distal humeral epiphysis is unossified at birth. The capitellum appears at 3–4 months, the medial epicondyle at 4–6 years, the trochlea at 8–9 years, and the lateral epicondyle at 9–11 years (34). However, variations from this pattern do occur. Absent ossification complicates imaging diagnosis during infancy, and even when epiphyseal ossification is present, diagnosis may be difficult. Inflicted distal humeral injuries can be roughly divided into three major categories; supracondylar fractures, SH/epiphyseal separations, and CMLs.
Supracondylar fractures
In contrast to diaphyseal fractures, fractures of the supracondylar portion of the distal humeral metaphysis have an overall low specificity for abuse (28). In Thomas and colleagues’ report of 14 humeral accidental and inflicted fractures in infants and toddlers noted over a 5-year period, they found all 3 supracondylar fractures to be due to accident (24). They concluded that “if a fall including trauma to the elbow is reported, supracondylar fractures should rarely be considered suspicious.” Their limited experience is at variance with that of Strait and colleagues, who found that 30% of inflicted humeral fractures were supracondylar (23). In infants under 15 months of age, 20% of supracondylar fractures were due to abuse. These authors found that patient age was a better predictor of fracture cause than fracture type. They noted only 1 supracondylar fracture due to abuse in children over 15 months of age. These findings are supported by Pandya and others who found that nearly two-thirds of their abusive humeral fractures were of the supracondylar type (27).
Although inflicted supracondylar fractures are less common than fractures of the shaft, it is clear that they do make up a significant percentage of humeral injuries in very young children. As with accidental injuries, most occur with hyperextension of the elbow. In the infant and young toddler, a humeral fracture should not be considered accidental simply because it involves the supracondylar region. Both accidental and inflicted supracondylar fractures may be accompanied by a history of a fall, and, thus, each patient must be assessed in a thorough manner, and when the mechanism is unclear, consultation with a Child Protection Team (CPT) is advisable.
Supracondylar fractures manifest a wide spectrum of radiologic patterns ranging from the subtle to the dramatic. Figure 4.27 illustrates bilateral injuries in a two-year-old abused child. Supracondylar fractures typically extend from the lateral metaphysis medially through the olecranon fossa. They may cross to the opposite cortex, producing a slight cortical irregularity where the fracture exits the bone. They may also be incomplete, extending a variable distance across the metaphysis (Fig. 4.28). The only indication of a supracondylar fracture may be a buckling of the posterior cortex. The findings at pathologic assessment may be considerably more striking (see Fig. 2.6). Occasionally SPNBF can be encountered in the supracondylar region without contour abnormality to indicate cortical disruption. Histologic assessment at autopsy may reveal only SPNBF without osseous disruption (Fig. 4.29).

Figure 4.27 Bilateral supracondylar fractures. A, Lateral view of the forearm and elbow in a two-year-old abused child demonstrates a grossly comminuted fracture with angulation and displacement of the distal fragments. There are associated distal radial and ulnar fractures (arrows). B, Lateral view of the other elbow obtained at the same time as A shows a subtle buckle-type supracondylar fracture (arrow). C, Follow-up study five days later demonstrates subtle SPNBF along the distal metaphysis, most evident anteriorly (arrows).
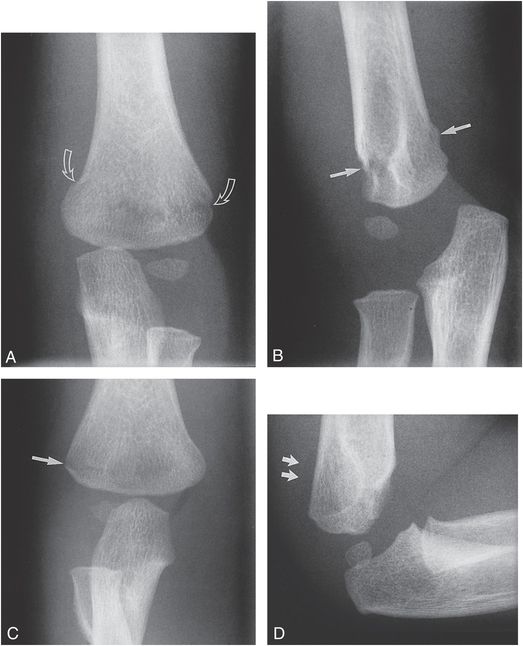
Figure 4.28 Bilateral supracondylar fractures. A, AP view of the left elbow in a 16-month-old abused child demonstrates a supracondylar fracture extending from the medial to the lateral cortices (arrows). (Same patient as in Fig. 4.49.) B, On the lateral view, there is buckling of the dorsal cortex and discontinuity of the ventral cortex (arrows). C, AP view of the right elbow demonstrates a fracture disrupting the lateral supracondylar cortex (arrow) that extends as far as the olecranon fossa. The medial cortex is intact. D, The lateral view fails to define the fracture but does indicate a joint effusion that displaces the posterior fat pad (arrows).
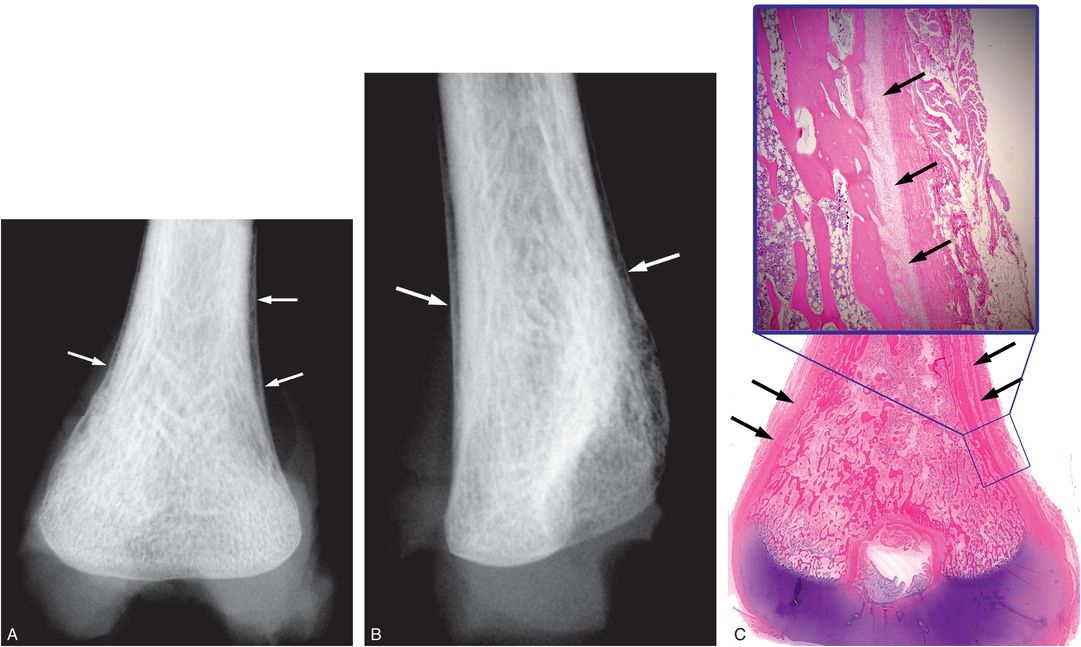
Figure 4.29 Supracondylar SPNBF without visible fracture – pathologic correlation. A five-month-old infant with a fatal head injury. (See same patient in Figs. 2.11, 3.78, 3.87, 4.21, 4.42.) A, B, Frontal and lateral specimen radiographs of the right distal humerus show SPNBF (arrows) without visible fracture. C, Corresponding very low power histologic image, with higher power insert, shows SPNBF (arrows), but no cortical or trabecular disruption.
SH injuries/epiphyseal separations
Physeal injuries and epiphyseal separations of the distal humerus are uncommon, but distinctive abusive fractures. Classically, they are transcondylar fractures, extending fully across the COJ, resulting in separation of the entire epiphysis, with variably sized and positioned metaphyseal fragments. They may also be unicondylar injuries, where the fracture extends either medially or laterally from the metaphysis into the physis, resulting in medial or lateral condylar fractures.
The distal humerus appears to be the most common site of epiphyseal separation in child abuse. Of the 15 SH injuries noted in 13 infants, Barber et al. found that 5 involved the distal humerus, more than at any other site (21). The accidental injury was first noted by Smith in 1850 (59). Even in the preradiography era, a distinction was made between distal humeral epiphyseal separation and the more common supracondylar fracture. The imaging features of these injuries received little attention until Rogers and Rockwood’s description in 1973 (60). The youngest patient in their series was a seven-month-old girl who was allegedly found in a crib with elbow deformity. In 1974, Chand described an epiphyseal separation in a 7-month-old abused infant who also had a femoral neck fracture (61). Others have stressed the importance of this lesion in abused infants (52, 62, 63). Modern cross-sectional imaging techniques have simplified the diagnosis.
Distal humeral epiphyseal separation is a well-described birth injury (see Chapter 11) (64, 65). The features of the birth injury are identical to those of the inflicted fracture, and insights gained from study of the injury in neonates are directly applicable to patterns noted in abuse. Although accidental epiphyseal separations can occur throughout early childhood, most inflicted injuries are found in infants and toddlers (66). The fracture presumably occurs as the infant is grabbed by the arm and pulled, twisted, or swung. The mechanics involved in the birth injury suggests that hyperextension of the elbow is a factor and the typical patterns of displacement also support this mechanism. With rare exceptions, the distal humeral epiphysis is displaced and angulated posteriorly with respect to the metaphysis. Additional medial, and less commonly, lateral displacement may occur (Fig. 4.30). Radiographic diagnosis is particularly difficult in young infants when there is no epiphyseal ossification (Fig. 4.31). The frontal radiograph may show normal anatomic relationships. Although the injury will be evident on a true lateral projection, it may be difficult to obtain this view; the diagnosis may be apparent only on an appropriate oblique view. The key to diagnosis is malalignment of the radial metaphysis and shaft with the distal humeral metaphysis (Fig. 4.31). Although the capitellum is not ossified, its normal location can be inferred from the radiograph, and a line drawn through the medullary cavity of the radius should intersect the capitellum. When epiphyseal separation is present, this line will fall medial to its normal point of intersection. In the absence of epiphyseal ossification, the pattern may be misconstrued as a dislocation. However, acquired elbow dislocations are rare in infants, and given the typical anatomic alterations, epiphyseal separation should be presumed.
Figure 4.30 Diagrams of distal humeral epiphyseal separation. Normal frontal (left, top) and lateral (left, bottom) views of the elbow. With physeal injury and epiphyseal separation (right images), there is posterior displacement and angulation with medial displacement (right upper image) of the distal humeral epiphysis (shaded regions).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree