10 Computed Tomography of Spinal Abnormalities
Computed tomography (CT) is a useful imaging modality for evaluating normal spinal anatomy and pathologic conditions involving the vertebrae and sacrum. Because of its high spatial resolution, CT can be utilized to evaluate pathologic disorders of vertebrae (neoplasms, inflammatory diseases, etc.), epidural soft tissues, disks, thecal sac, facet joints, and paravertebral structures.
The normal spine is comprised of 7 cervical, 12 thoracic, and 5 lumbar vertebrae. The upper two cervical vertebrae have different configurations than the other vertebrae. The atlas (C1) has a horizontal ringlike configuration with lateral masses that articulate with the occipital condyles superiorly and the superior facets of C2 inferiorly. The dorsal margin of the upper dens is secured in position in relation to the anterior arch of C1 by the transverse ligament. Various anomalies occur in this region, such as atlanto-occipital assimilation, segmentation (e.g., block vertebrae), basiocciput hypoplasia, condylus tertius, and os odontoideum. The lower five cervical vertebral bodies have rectangular shapes with progressive enlargement inferiorly. Superior and lateral projections from the C3 to C7 cervical vertebral bodies form the uncovertebral joints. The transverse processes are located anterolateral to the vertebral bodies and contain the foramina transversaria within which the vertebral arteries and veins are located. The posterior elements consist of paired pedicles, articular pillars, laminae, and spinous processes. The cervical spine has a normal lordosis.
The 12 thoracic vertebral bodies and 5 lumbar vertebral bodies progressively increase in size caudally. The posterior elements include the pedicles, transverse processes, laminae, and spinous processes. The transverse processes of the thoracic vertebrae also have articulation sites for ribs. The thoracic spine has a normal kyphosis and the lumbar spine a normal lordosis. Anterior and posterior longitudinal ligaments connect the cervical vertebrae, and interspinous ligaments and ligamenta flava provide stability for the posterior elements.
The cortical margins of the vertebral bodies have dense compact bone structure. The medullary compartments of the vertebrae are comprised of bone marrow and trabecular bone. Pathologic processes such as tumor, inflammation, and infection result in bone lysis with or without extension of the intramedullary lesions through destroyed cortical bone. Contrast enhancement may also be seen at the pathologic sites. Because of direct visualization of these pathologic processes in the marrow, magnetic resonance imaging (MRI) can often detect these abnormalities sooner than CT, which relies on later indirect signs of trabecular destruction for confirmation of disease.
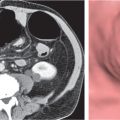
The intervertebral disks enable flexibility of the spine. The two major components of normal disks, the nucleus pulposus and anulus fibrosus, are seen as structures with intermediate attenuation. The outer anulus fibrosus is made of dense fibro-cartilage. The central nucleus pulposus is made of gelatinous material. The combination of various factors, such as decreased turgor of the nucleus pulposus and loss of elasticity of the anulus with or without tears, results in degenerative changes in the disks. CT features of disk degeneration include decreased disk heights, vacuum disk phenomena, disk bulging, and associated vertebral body osteophytes. Radial tears of the anulus fibrosus are often clinically significant and are associated with disk herniations. The term disk herniation usually refers to extension of the nucleus pulposus through an annular tear beyond the margins of the adjacent vertebral body end plates. Disk herniations can be further subdivided as protrusions (when the head of the herniation equals the neck in size), extrusions (when the head of the herniation is larger than the neck), or extruded fragments (when there is separation of the herniated disk fragment from the disk of origin). Disk herniations can occur in any portion of the disk. Posterior and posterolateral herniations can cause compression of the thecal sac and contents, as well as compression of epidural nerve roots in the lateral recesses or within the intervertebral foramina. Lateral and anterior disk herniations are less common but can cause hematomas in adjacent structures. Disk herniations that occur superiorly or inferiorly result in focal depressions of the vertebral cortical end plates (i.e., Schmorl nodes). On CT, recurrent disk herniations may be difficult to delineate from scar or granulation tissue. MRI, however, can be used in these situations because herniated disks do not typically enhance after gadolinium contrast administration, whereas scar tissue typically shows contrast enhancement.
The thecal sac is a meningeal covered compartment containing cerebrospinal fluid (CSF), which is contiguous with the basal subarachnoid cisterns and extends from the upper cervical level to the level of the sacrum. The thecal sac contains the spinal cord and exiting nerve roots. The distal end of the conus medullaris is normally located at the T12–L1 level in adults. Lesions within the thecal sac are categorized as intradural intra- or extramedullary. Intramedullary lesions directly involve the spinal cord, whereas extramedullary lesions do not primarily involve the spinal cord. Extra- or epidural lesions refer to spinal lesions outside the thecal sac.
Evaluation of the spinal cord, intradural nerves, and spinal subarachnoid space can be done with CT using myelography by placement of iodinated contrast into the thecal sac by percutaneous needle injection. Diffuse or focal abnormal expansion of the spinal cord, intradural extramedullary lesions, and nerve root compression can be evaluated with CT myelography. MRI with high soft tissue contrast resolution, however, is typically superior to CT in the evaluation of the spinal cord and various intramedullary pathologic conditions, such as congenital malformations, neoplasms, benign mass lesions (dermoid, arachnoid cyst, etc.), inflammatory/infectious processes, traumatic injuries (contusions and hematomas), and ischemia/infarction, as well as the adjacent CSF and nerve roots. MRI after the intravenous administration of gadolinium contrast agents is also useful for evaluating lesions within the spinal cord, as well as neoplastic or inflammatory diseases within the thecal sac.
The normal blood supply to the spinal cord consists of seven or eight radicular arteries that enter the spinal canal through the intervertebral foramina to supply the three main vascular territories of the spinal cord (cervicothoracic: cervical and upper three thoracic levels, midthoracic: T4 level to C7 level, and thoracolumbar: T8 level to lumbosacral plexus). The cervicothoracic vascular distribution is supplied by radicular branches arising from the vertebral arteries and costocervical trunk. The midthoracic territory is often supplied by a radicular branch at the C7 level. The thoracolumbar territory is supplied by a single artery arising from the ninth, tenth, eleventh, or twelfth intercostal arteries (75%); the fifth, sixth, seventh, or eighth intercostal arteries (15%); or the first or second lumbar arteries (10%). The radicular arteries supply the longitudinally oriented anterior spinal artery, which is located in the midline anteriorly adjacent to the spinal cord and supplies the gray matter and central white matter of the spinal cord. The radicular arteries also supply the two major longitudinally oriented posterior spinal arteries that course along the posterolateral sulci of the spinal cord, as well as one third to one half of the outer rim of the spinal cord via a peripheral anastomotic plexus. Ischemia or infarcts involving the spinal cord represent rare disorders associated with atherosclerosis, diabetes, hypertension, abdominal aortic aneurysms, and abdominal aortic surgery. Vascular malformations can be seen within the thecal sac, with or without involvement of the spinal cord.
Epidural structures of clinical importance include the (1) lateral recesses (anterolateral portions of the spinal canal located between the thecal sac and pedicles that contains nerve roots, vessels and fat), (2) dorsal epidural fat pad, (3) posterior elements and facet joints, and (4) posterior longitudinal ligament and ligamentum flavum. The intervertebral foramina represent the bony channels between the pedicles through which the nerves traverse.
Narrowing of the thecal sac, lateral recesses, and intervertebral foramina can result in clinical signs and symptoms. The narrowing can result from disk herniations, posterior vertebral body osteophytes, hypertrophy of the ligamentum flavum and facet joints, synovial cysts, excessive epidural fat, epidural neoplasms, abscesses, hematomas, spinal fractures, spondylolis-thesis, or spondylolysis. CT is useful for evaluating these disorders and for categorizing the degree of narrowing of the thecal sac, as well as compression of nerve roots in the lateral recesses and intervertebral foramina.
CT plays a major role in the evaluation of traumatic injuries to the spine. The high definition and detail of bone anatomy displayed with CT using reformatted images in coronal and sagittal planes enable detection of complex and/or subtle vertebral fractures, retropulsed fracture fragments into the spinal canal and/or intervertebral foramina, and disruption of the foramina transversaria with associated injuries of the vertebral arteries. Stability of fractures can be related to findings on CT using the Denis three-column model. The anterior column consists of the anterior half of the vertebral body and disk, along with the anterior longitudinal ligament. The middle column consists of the posterior half of the vertebral body and disk, along with the posterior longitudinal ligament. The posterior column consists of the posterior bony vertebral arch, inter- and supraspinous ligament complex, ligamentum flavum, and facet joints and capsule. Minor injuries involve only part of one column and typically do not lead to instability. Compression fractures involving only the anterior column with disruption of the anterior end plate (often between T6–T8 and T12–L3) with an intact spinal canal are considered stable. Burst fractures that result from an axial loading injury with disruption of the anterior and middle columns (often at the thoracolumbar junction and T10–L5) can be seen with CT as buckling of the anterior, superior, and posterior end plates with or without retropulsed bone fragments into the spinal canal and are often unstable. Seat belt fractures (Chance fractures) are flexion-compression fractures involving the anterior, middle, and posterior columns and are typically unstable. Fracture-dislocation fractures represent unstable fractures involving all three columns from combinations of compression, tension, and rotation/shear forces.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree