10 Computed Tomography of Spinal Abnormalities(Table 10.5 – Table 10.7)
Lesions | CT Findings | Comments |
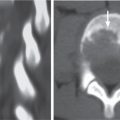
Fracture (traumatic/osteopenic) | Traumatic vertebral fracture: Acute/subacute fractures have sharply angulated cortical margins, no destructive changes at cortical margins of fractured end plates; with or without convex outward angulated configuration of compressed vertebral bodies, with or without spinal cord and/or spinal canal compression related to fracture deformity, with or without retropulsed bone fragments into spinal canal, with or without subluxation, with or without kyphosis, with or without epidural hematoma. Osteopenic vertebral fracture: Acute/subacute fractures usually have sharply angulated cortical margins, no destructive changes at cortical margins of fractured vertebral bodies; with or without compression deformities involving other vertebral bodies, with or without convex outward angulated configuration of compressed vertebral bodies, with or without spinal cord and/or spinal canal compression related to fracture deformity, with or without retropulsed bone fragments into spinal canal, with or without subluxation, with or without kyphosis, with or without epidural hematoma. Chronic healed fractures usually have normal or near normal signal in compressed vertebral body. Occasionally, persistence of signal abnormalities in vertebral marrow results from instability and abnormal axial loading. | Vertebral fractures can result from trauma in normal bone or as pathologic fractures in abnormal bone associated with primary bone tumors/lesions, metastatic disease, bone infarcts (steroids, chemotherapy, and radiation treatment), osteoporosis, osteomalacia, metabolic (calcium/phosphate) disorders, vitamin deficiencies, Paget disease, and genetic disorders (osteogenesis imperfecta, etc.). |
Occipital condyle fractures | Rough edge fragments of one or both occipital condyles. Fractures may extend to involve the hypoglossal canals and jugular foramina. | Type 1: Traumatic fracture of condyle with minimal displacement from axial loading mechanism from high-energy blunt trauma (often stable if only unilateral). Type 2: Fracture of occipital condyle from shear mechanism extending into skull base (can be stable if unilateral or unstable). Type 3: Transverse fracture of condyle from rotation/bending with injury to alar ligaments that extend from upper lateral portions of the dens to the medial aspects of the occipital condyles. Injury to the alar ligaments results in instability at the occipitocervical junction. |
Atlanto-occipital dislocation | Abnormal increased distance from the basion of the clivus to the tip of the odontoid using the basion-axial interval (BAI) and/or basion-dental interval (BDI). The BAI is the distance from the basion to a line drawn along the dorsal surface of the C2 body (normal BAI for adults ranges from –4 to 12 mm, children 0 to 12 mm). The BDI is only used in patients older than 13 y and is the distance from the basion to the tip of the dens (normal range 2–12 mm). | Unstable injury from disruption of ligaments between the occiput, C1, and upper dens from high kinetic energy injuries (usually motor vehicle collisions). Often associated with traumatic injuries to brainstem and cranial nerves. More common in children than adults. |
Jefferson C1 fracture | Rough edge fractures of the arch of C1, often multiple fracture sites. | Compression burst fracture of the arch of C1, often stable, can be unstable when there is disruption of transverse or posterior ligament or comminution of anterior arch, often associated with fractures at other cervical vertebrae. |
C2 dens fracture | Type I: Fracture at the upper portion of dens above transverse ligament (unstable) from avulsion at the alar ligament. Type II: Transverse fracture through the lower portion of the dens (may be unstable). Type III: Oblique fracture involving the dens and body of C2 (usually stable). | Traumatic fracture involving the upper, middle to lower portions of the dens. |
C2 body fracture type I | Fracture of the inferior end plate of C2 with teardrop fragment. | Extension injury with teardrop fracture of anteroinferior vertebral end plate of the C2 vertebra. |
C2 body fracture type II | Horizontal fracture plane through the lower body of C2. | Horizontal shear fracture through the lower portion of the C2 body (lower than C2 dens type III fracture). |
C2 body fracture type III (burst fracture) | Comminuted fracture of C2 body with or without separation of body from posterior arch (hangman’s fracture). Fracture fragments of C2 body are often displaced peripherally, with or without extension of fragments into spinal canal compression. | Traumatic comminuted fracture of the C2 body from axial compression force. Often unstable, especially with associated hang-man’s fracture; with or without spinal cord contusion. |
C2 body fracture type IV | Sagittal plane fracture through C2. | Severe unstable fracture in the sagittal plane through C2. |
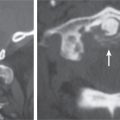
C2 hangman’s fracture | Disrupted ring of C2 from bilateral pedicle fractures separating the C2 body from the posterior arch of C2. Skull, C1, and C2 bodies are displaced anteriorly with respect to C3. | Unstable injury from traumatic bilateral pedicle fractures from hyperextension and distraction mechanisms with separation of the C2 body from the posterior arch of C2. Fractures can extend into C2 body and/or through foramen transversarium with injury/occlusion of vertebral artery. Often associated with spinal cord injury. |
Hyperflexion cervical spine injury | Sagittal plane fracture associated with compression of the anterior portion of the vertebral body, with teardrop fracture at the anteroinferior portion of the vertebral body or quadrangular fracture extending from the inferior end plate to the anterosuperior cortical margin. A portion of the fractured vertebral body is usually subluxed anteriorly with respect to the vertebral body below with resultant kyphosis. Facet joints are widened due to disruption. Narrowing of the disk height seen below the vertebral body fracture from disk injury. Typically, prevertebral soft tissue swelling is seen, with widened interspinous distance. | Flexion compression injuries that account for up to 15% of cervical vertebral fractures and often occur from motor vehicle collisions, falls, and diving into shallow water. Fractures involve the anterior portion of the vertebral body with fractures also involving the posterior elements in 50%, with or without tearing of posterior ligaments. Teardrop hyperflexion injuries result in disruption of all ligaments, facet joints, and disks. Quadrangular fractures extend from the inferior to superior cortical margins with disruption of the anterior and posterior longitudinal ligaments and disks. |
Hyperextension injury cervical fracture | Fractures of vertebral bony arch (laminae, facets, and spinous process) on axial CT images. Sagittal CT images show malalignment of facets and/or spondylolisthesis. | Extension injury from posterior displacement of the head and upper cervical spine resulting in fractures of the arch (laminae) and/or posterior elements, with or without disruption of anterior longitudinal ligament. Disruption of posterior column results in instability. Can be associated with spinal cord contusion, vertebral artery injury (dissection/occlusion), and other vertebral fractures. |
Hyperflexion-rotation cervical injuries | Rotatory subluxation of vertebral body and posterior elements, with or without jumped or perched facets, with or without fractures at facets, with or without fracture of the vertebral body. For unilateral locked facet, axial CT image shows rotatory subluxation with absence of normal facet articulation (naked facet sign). Sagittal CT images show perched or jumped facets. | Hyperflexion-rotation force resulting in traumatic disruption of spinal ligaments (facet-capsular, annular, and/or longitudinal ligaments) with subluxation involving the facet joints with or without fracture. Can occur as unilateral or bilateral locked facets. |
Hyperextension-rotation cervical injuries | Unilateral fracture of articular pillar, pedicle, and/or lamina, with or without injury/occlusion of vertebral artery. | Unilateral laminar or facet fracture with ligament disruption (anterior annular and capsular ligaments) from combined hyperextension and rotation mechanism of injury. |
Cervical vertebral burst fracture | Comminuted fracture extending through both end plates of vertebral body; associated fractures at the posterior elements. | Comminuted fractures involving the superior and inferior end plates of a cervical vertebral body secondary to axial compression mechanism without fractures involving the posterior elements. Can be unstable if both anterior and middle columns involved. |
Cervical vertebral fracture/dislocation | Comminuted fractures of posterior elements (laminae, facets, and spinous processes) associated with anterior, lateral, and/or posterior subluxations; with or without fractures involving vertebral bodies, disks, and transverse processes. | Highly unstable fractures involving all three columns from shear, rotation, and distraction mechanisms. Subluxed fracture components involving the vertebral body usually also involve tearing of the disk. Lateral flexion mechanism of injury resulting in unilateral fracture of articular pillar, with or without fractures of vertebral body, transverse process. |
Cervical lateral flexion injury | Sagittal plane fracture or articular pillar with malalignment, with or without fracture of vertebral body, transverse process. |
|
Clay shoveler’s fracture | Avulsion fracture from the spinous processes of C6 and C7. Occasionally occurs at other levels. | Stable fracture from avulsion of bone from the C6 or C7 spinous processes by the posterior supraspinous ligaments as a result of strong shear forces secondary to lifting heavy weights with arms extended. |
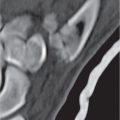
Thoracic/lumbar anterior compression fracture | Anterior wedge-shaped vertebral body from fractures involving the superior end plate and anterior cortical margin. Multiple fracture lines often seen within the vertebral body. Decrease in height of vertebral body with normal bone density up to 50%. Usually no subluxation because of lack of significant injury to posterior column. | Flexion-induced fracture of anterior portion of vertebral body from axial load injury involving only the anterior column and sparing the middle and posterior columns. Can occur from trauma in normal or osteoporotic bone. Fractures in the setting of osteoporosis can have delayed or inadequate healing, resulting in progressive height loss. Typically stable because of lack of involvement of the middle and posterior columns. Can involve more than one level. |
Thoracic/lumbar lateral compression fracture | Lateral wedge-shaped vertebral body from fractures involving the superior end plate and lateral cortical margin. Typically spares the posterior cortical margin of the vertebral body without retropulsed fragments. Commonly occur at T12 to L2 and at T6 and T7; multiple vertebrae involved in 20%. | Asymmetric fracture involving superior and anterior end plates of vertebral body from asymmetric axial load with or without flexion. Can occur from trauma in normal or osteoporotic bone. Fractures in the setting of osteoporosis can have delayed or inadequate healing resulting in progressive height loss. Typically stable because of lack of involvement of the middle and posterior columns. Can involve more than one level. |
Thoracic/lumbar burst fracture | Comminuted fracture of vertebral body involving both superior and inferior end plates, decrease in vertebral body height at anterior and posterior cortical margins, often with bone fragments displaced into the spinal canal, widened pedicles; with or without malalignment of fractured vertebral body and/or facets. | Unstable comminuted compression fractures involving the vertebral body from axial compression mechanism without fractures involving the posterior elements. Can be unstable if both anterior and middle columns involved. |
Thoracic/lumbar facet–lamina fracture | Fractures involving laminae and facet joints with widened neural arch/pedicles, with or without vertebral body and/or facet subluxation/dislocation, with or without comminution of vertebral body. | Fractures involving the posterior column from extension, flexion-distraction, or flexion-rotation mechanisms. Often occur between T11 and L4. Unstable fractures occur when all three columns are involved. Can be stable when one or two columns are involved. |
Thoracic/lumbar chance fracture | Fractures involving the anterior, middle, and posterior columns; anterior wedging of vertebral body with decrease in height of vertebral body often > 50% even with normal bone density. Horizontally oriented fracture planes through vertebral body and posterior elements, disruption/separation of facet joints and interspinous ligaments with widening of the interspinous distance; with or without comminuted fractures of vertebral body, with or without retropulsed fracture fragments from vertebral body into spinal canal; widened interspinous distance; with or without anterior displacement of vertebrae above fracture (distraction fracture). | Unstable flexion-distraction injury from high-velocity collision or fall causing compression of the anterior column and distraction of middle and posterior columns. Often occurs between T11 and L3. |
Thoracic/lumbar fracture- dislocation | Comminuted fractures of posterior elements (laminae, facets, and spinous processes) associated with anterior, lateral, and/or posterior subluxations; with or without fractures involving vertebral bodies, disks, transverse processes, and/or ribs. | Highly unstable fractures involving all three columns from shear, rotation, and distraction mechanisms. Subluxed fracture components involving the vertebral body usually also involve tearing of the disk. |
Fracture/ankylosing spondylitis | Rigidity of the spine caused by ossification of the anterior and posterior longitudinal ligaments, syndesmophytes, and osteoporosis; increases the predisposition to spinal fractures with minor trauma. Fractures can occur through the vertebral body and/or disk. Also associated with atlantodens instability. | Autoimmune inflammatory disorder associated with HLA-B27. Inflammation involves the sacroiliac joints, diskovertebral junctions, spinal ligaments, apophyseal joints, costovertebral joints, and atlantoaxial joints. Findings include osteitis, sydesmophytosis, diskovertebral erosions, calcifications along the anterior and posterior longitudinal ligaments, osseous fusion across joints, and osteoporosis. |
Fracture (malignancy-related) | Fractures often associated with destructive changes at cortical margins of vertebrae, with or without convex outward-bowed configuration of compressed vertebral bodies, with or without paravertebral mass lesions, with or without destructive lesions in other vertebrae. | Neoplasms in bone are associated with bone destruction and decreased capability for maintaining integrity with axial loading, as well as lowering the threshold for fracture with minor trauma. |
Epidural hematoma | Epidural collection with low to intermediate and/or slightly high attenuation, with or without spinal cord compression, with or without minimal peripheral pattern of enhancement at hematoma. | The CT appearance of epidural hematoma depends on the age, hematocrit, and degree of clot formation and retraction. Can be spontaneous or result from trauma or complication (coagulopathy, lumbar puncture, myelography, and surgery). |
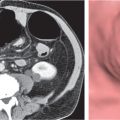
Disk herniation | Disk herniation/protrusion: Disk herniation in which the head of the protruding disk is equal in size to the neck on sagittal reconstructed images. Disk herniation/extrusion: Disk herniation in which the head of the disk herniation is larger than the neck on sagittal reconstructed images. Disk herniation/extruded disk fragment: Disk herniation that is not in contiguity with disk of origin. | Represents a disk herniation (focal > broad-based) that results from inner annular disruption or subtotal annular disruption with extension of nucleus pulposus toward annular injury with expansive deformation. Represents a disk herniation (focal > broad-based) with extension of nucleus pulposus through zone of annular disruption with expansive deformation. Disk herniation/extruded disk fragment–herniation/extrusion: Herniated fragment of nucleus pulposus without connection to disk of origin. Disk herniations can be midline, off-midline in lateral recess, posterolateral within inter-vertebral foramen, lateral, or anterior. Can extend superiorly, inferiorly, or both directions; with or without associated epidural hematoma, with or without compression or displacement of thecal sac and/or nerve roots in lateral recess and/or foramen. Disk herniations can occur into the end plates of vertebral bodies, Schmorl nodes. |



















Lesions | CT Findings | Comments |
Dural ectasia | Scalloping of the dorsal aspects of vertebral bodies, dilation of optic nerve sheaths, dilation of intervertebral and sacral foraminal nerve sheaths, lateral meningoceles. | Dural dysplasia associated with NF1. Can also be seen with connective tissue disease, such as Marfan syndrome. |
Tarlov cysts (perineural cysts) | Well-circumscribed cysts with attenuation comparable to cerebrospinal fluid (CSF) involving nerve root sleeves associated with chronic erosive changes involving adjacent bony structures. Sacral (with or without widening of sacral foramina) > lumbar nerve root sleeves. Usually range from 15 to 20 mm in diameter but can be larger. | Typically represent incidental asymptomatic anatomical variants. |
Dorsal dermal sinus | Epithelial-lined tube extending internally from the dorsal skin of lower back, with or without extension into spinal canal through the median raphe or spina bifida, with or without associated dermoid or epidermoid in spinal canal (~50%). | Abnormality resulting from lack of normal developmental separation of superficial and neural ectoderm. Lumbar region > occipital region. Potential source of infection involving spine and spinal canal. |
Dermoid | Well-circumscribed, spheroid or multilobulated, intradural extramedullary or intramedullary lesions, usually with low to intermediate attenuation. No contrast enhancement. Lumbar region most common location in spine. Can cause chemical meningitis if dermoid cyst ruptures into the subarachnoid space. Commonly located at or near midline. | Nonneoplastic congenital or acquired ectodermal inclusion cystic lesions filled with lipid material, cholesterol, desquamated cells, and keratinaceous debris; usually mild mass effect on adjacent spinal cord or nerve roots; adults: M > F; with or without related clinical symptoms. |
Epidermoid | Well-circumscribed, spheroid or multilobulated, intradural or extramedullary lesion with low to intermediate attenuation No contrast enhancement. | Nonneoplastic extramedullary epithelial-inclusion lesions filled with desquamated cells and keratinaceous debris; usually mild mass effect on adjacent spinal cord and/or nerve roots. May be congenital (with or without associated with dorsal dermal sinus, spina bifida, and hemivertebrae) or acquired (late complication of lumbar puncture). |
Neurenteric cyst | Circumscribed intradural extramedullary structures with low to intermediate attenuation. Usually no contrast enhancement. Location: thoracic > cervical > posterior cranial fossa > craniovertebral junction > lumbar; usually midline in position and often ventral to the spinal cord. Typically associated with anomalies of the adjacent vertebrae. | Results from developmental failure of separation the notochord and foregut; observed in patients older than 40 y. |
Neoplasm and other masses | ||
Ependymoma | Intradural, circumscribed, lobulated lesions at conus medullaris and/or cauda equina/filum terminale, rarely in sacrococcygeal soft tissues; lesions usually have intermediate attenuation, with or without hemorrhage. | Ependymomas at conus medullaris or cauda equina/filum terminale usually are myxopapillary type, thought to arise from ependymal glia of filum terminale. Slight male predominance. Usually are slow-growing neoplasms associated with long duration of back pain, sensory deficits, motor weakness, and bladder and bowel dysfunction; with or without chronic erosion of bone with scalloping of vertebral bodies and enlargement of intervertebral foramina. |
Schwannoma (neurinoma) | Circumscribed or lobulated extramedullary lesions, intermediate attenuation, with contrast enhancement. Large lesions can have cystic degeneration and/or hemorrhage. | Encapsulated neoplasms arising asymmetrically from nerve sheath; most common type of intradural extramedullary neoplasms; usual presentation in adults with pain and radiculopathy, paresthesias, and lower extremity weakness. Multiple schwannomas seen with NF2. |
Meningioma | Extra- or intradural extramedullary lesions, intermediate attenuation, with contrast enhancement, with or without calcifications. | Usually benign neoplasms, typically occurs in adults (> 40 y), F > M; multiple meningiomas seen with NF2; can result in compression of adjacent spinal cord and nerve roots, rarely invasive/malignant types. |
Neurofibroma | Lobulated extramedullary lesions with or without irregular margins, with or without extradural extension of lesion with dumbbell shape, with contrast enhancement; with or without erosion of foramina, with or without scalloping of dorsal margin of vertebral body (chronic erosion or dural ectasia/NF1). | Unencapsulated neoplasms involving nerve and nerve sheath; common type of intradural extramedullary neoplasms often with extra-dural extension; usual presentation in adults with pain and radiculopathy, paresthesias, and lower extremity weakness. Multiple neurofibromas seen with NF1. |
Paraganglioma | Spheroid or lobulated intradural-extramedullary lesion with intermediate attenuation, with or without tubular vessels, with contrast enhancement, with or without foci of hemorrhage; usually located in region of cauda equina and filum terminale. | Paragangliomas are neoplasms that arise from paraganglion cells of neural crest origin and usually occur at carotid body, jugular foramen, middle ear, and along vagus nerve. Rarely occur in spine. |
Leptomeningeal metastases | Single or multiple nodular lesions and/or focal or diffuse abnormal subarachnoid disease along pial surface of spinal cord. Leptomeningeal tumor is best seen on postmyelo-graphic CT images. | Disseminated tumor in the subarachnoid space (leptomeninges) usually is associated with significant pathology (neoplasm vs inflammation and/or infection). Primary neoplasms commonly associated with disseminated subarachnoid tumor include primitive neuroectodermal tumors (e.g., medulloblastoma), glioblastoma, ependymoma, and choroid plexus papilloma/carcinoma. Metastases within CSF can result from direct extension through the dura or by hematogenous dissemination or via the choroid plexus. The most frequent primary neoplasms outside CNS within subarachnoid metastases are lung carcinoma, breast carcinoma, melanoma, lymphoma, and leukemia. |
Arachnoid cyst | Well-circumscribed intradural extramedullary lesions with attenuation similar to CSF, no contrast enhancement. | Nonneoplastic congenital, developmental, or acquired extra-axial lesions filled with CSF; usually mild mass effect on adjacent spinal cord or nerve roots. |
Teratoma | Circumscribed lesions with variable low, intermediate, and/or high attenuation; with or without contrast enhancement. May contain calcifications and cysts, as well as fatty components that can cause chemical meningitis if ruptured. | Composed of derivatives of ectoderm, mesoderm, and/or endoderm. |
Leptomeningeal infection/inflammation | Single or multiple nodular subarachnoid lesions or thickened nerve roots on postmyelographic CT images. Lepto meningeal inflammation often best seen on postcontrast MRI. | Contrast enhancement in the subarachnoid space (leptomeninges) on MRI is usually associated with significant pathology (inflammation and/or infection vs neoplasm). Inflammation and/or infection of the leptomeninges can result from pyogenic, fungal, or parasitic diseases, as well as tuberculosis. Neurosarcoid results in granulomatous disease in the leptomeninges, producing similar patterns of subarachnoid enhancement. |
Adhesive arachnoiditis | Clumping of nerve roots within the thecal sac and/or peripheral positioning of nerve roots within the thecal sac, “empty sac” sign on postmyelographic CT images. | Adhesive arachnoiditis is a chronic disorder that results in aggregation of nerve roots within the thecal sac or adhesion of nerve roots to the inner margin of the thecal sac. Can result from prior surgery, hemorrhage, radiation treatment, meningitis, or myelography (pantopaque). |
Arachnoiditis ossificans | Irregular zones with high attenuation in the subarachnoid space. | Chronic inflammatory disorder that results in metaplastic ossification changes in the subarachnoid space; usually occurs in the thoracic and lumbar regions. Can be associated with prior infection, prior myelography, and surgery. |
Pyogenic arachnoiditis | Nerve root enlargement with or without clumping of nerve roots within the thecal sac on postmyelographic CT. Contrast enhancement on MRI involving one or more nerve roots within the thecal sac. | Pyogenic arachnoiditis can result from surgical complication, extension of intracranial meningitis, epidural abscess, vertebral osteomyelitis, or immunocompromised status. |
Vascular | ||
Arteriovenous malformation (AVM) | Lesions with irregular margins that can be located in the spinal cord (white and/or gray matter), dura, or both locations. AVMs contain multiple tortuous vessels, as well as areas of hemorrhage in various phases, calcifications, gliosis, and myelomalacia. The venous portions often show contrast enhancement. | Intracranial AVMs much more common than spinal AVMs. Annual risk of hemorrhage. AVMs can be sporadic, congenital, or associated with a history of trauma. |
Other | ||
Hemorrhage within CSF | Hemorrhage into CSF can result in transient amorphous increased attenuation. | Hemorrhage into CSF from cranial or spinal surgery, trauma, vascular malformation, or neoplasm can result in leptomeningeal enhancement. |
Intradural herniated disk | Amorphous structure with intermediate attenuation. | Disk herniations rarely extend through dura into the thecal sac. |





Lesions | CT Findings | Comments |
Inflammatory | ||
Demyelinating disease | ||
Multiple sclerosis | Intramedullary lesion or multiple lesions in spinal cord. MRI is the optimal test to evaluate for lesions in the spinal cord. CT myelography may show focal zones of atrophy in the spinal cord at old plaques. | Multiple sclerosis is the most common acquired demyelinating disease usually affecting women (peak ages 20–40 y). Plaques in spinal cord associated with atrophy often associated with relapsing/remitting type of multiple sclerosis (MS). Devic disease is a variant of MS that consists of optic neuritis and progressive demyelination of spinal cord without evidence of demyelination in the brain. |
Acute disseminated encephalomyelitis (ADEM) | Intramedullary lesion or multiple lesions in spinal cord. MRI is the optimal test to evaluate for lesions in the spinal cord. CT myelography may show focal zones of atrophy in the spinal cord at remote sites of demyelination. | ADEM is a noninfectious monophasic inflammatory/demyelination process involving the spinal cord and/or brain that occurs several weeks after viral infection or vaccination. Children > adults. Associated with various bilateral motor and sensory deficits. |
Transverse myelitis | Intramedullary lesion or multiple lesions in spinal cord. MRI is the optimal test to evaluate for lesions in the spinal cord. CT myelography may show focal zones of atrophy in the spinal cord at remote sites of demyelination. | Transverse myelitis is a noninfectious inflammatory process involving both halves of the spinal cord, as well as gray and white matter; multiple causes: demyelination after viral infection or vaccination (possibly a variant of ADEM), autoimmune diseases/collagen vascular diseases (systemic lupus erythematosus), paraneoplastic syndromes, atypical multiple sclerosis, idiopathic; can be diagnosis of exclusion; M > F, mean age 45 y. Associated with various bilateral motor and sensory deficits. Pathologic changes considered to be a combination of demyelination and arterial or venous ischemia. |
Other noninfectious inflammatory diseases involving the spinal cord | ||
Sarcoid | Intramedullary lesion or multiple lesions in spinal cord. MRI is the optimal test to evaluate for lesions in the spinal cord. CT myelography may show focal zones of enlargement of the spinal cord. | Sarcoidosis is a multisystem, noncaseating, granulomatous disease of uncertain etiology that involves the CNS in ~5% to 15%. Rarely involves the spinal cord. Association with severe neurologic deficits if untreated. May mimic intramedullary neoplasm. |
Infectious diseases of the spinal cord | ||
Abscess | Intramedullary lesion in spinal cord best seen with MRI. CT myelography may show focal zone of enlargement of the spinal cord at the site of abscess. | Infection can result from hematogenous dissemination or spread within CSF. Organisms reported to result in spinal cord abscess or nonviral myelitis include Streptococcus milleri, Streptococcus pyogenes, Mycobacterium tuberculosis, atypical mycobacteria, syphilis, Schistosoma mansoni, and fungi (Cryptococcus, Candida, and Aspergillus); seen in immunocompromised patients. |
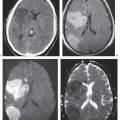
Parasitic | Intramedullary lesion in spinal cord best seen with MRI. CT myelography may show focal zones of enlargement of the spinal cord at the site of abscess; with or without leptomeningeal lesions. Concurrent lesions in brain are usually present. | Parasitic infection of the spinal cord is rare. The most common type of parasite to involve the spinal cord is Toxoplasma gondii in immuno-compromised patients. Toxoplasmosis rarely involves the spinal cord unlike cerebral infection. S. mansoni can involve the spinal cord in immunocompetent patients in Asia/Africa. Associated with rapid decline in neurologic function related to site of lesion in spinal cord. |
Vascular | ||
Intramedullary hemorrhage | Intramedullary lesion in spinal cord best seen with MRI. CT myelography may show focal zone of enlargement of the spinal cord at the site of hematoma. | Can result from trauma, vascular malformations, coagulopathy, amyloid angiopathy, infarction, metastases, abscesses, viral infections (herpes simplex, cytomegalovirus [CMV]). |
Arteriovenous malformation | Lesions with irregular margins that can be located in the spinal cord (white and/or gray matter), dura, or both locations. AVMs contain multiple tortuous tubular vessels as calcifications, as seen on CT and CT myelography. Not usually associated with mass effect unless there is recent hemorrhage or venous occlusion. | Intracranial AVMs much more common than spinal AVMs. Annual risk of hemorrhage. AVMs can be sporadic, congenital, or associated with a history of trauma. Multiple AVMs can be seen in syndromes: Rendu–Osler–Weber: AVMs in brain and lungs and mucosal capillary telangiectasias; Wyburn–Mason: AVMs in brain and retina, with cutaneous nevi. |
Syringohydromyelia | Enlarged spinal cord with intramedullary fluid-filled zone that is central or slightly eccentric. | Hydromyelia refers to distention of the central canal of the spinal cord (lined by ependymal cells). Syringomyelia refers to dissection of CSF into the spinal cord (not lined by ependymal cells). Syringohydromyelia refers to combination of both. May be secondary to congenital/developmental anomalies (Chiari I, Chiari II malformations, and basilar invagination) and also secondary to neoplasms of the spinal cord (astrocytoma, ependymoma, and hemangioblastoma). |
Neoplastic | ||
Astrocytoma | Intramedullary expansile lesions as seen on CT myelography. Lesions often extend multiple vertebral segments. Locations: cervical spinal cord > upper thoracic spinal cord > conus medullaris. | Most common intramedullary tumor in children, second most common in adults. Occurs more frequently in children than adults. Most are low-grade tumors (90% children, 75% adults). Anaplastic astrocytomas account for most of the rest, glioblastomas account for only 1%. |
Ependymoma | Intramedullary circumscribed expansile lesion, often midline/central location in spinal cord. Intramedullary locations: cervical spinal cord (44%), both cervical and upper thoracic spinal cord (23%), thoracic spinal cord (26%). Lesions often extend three or four vertebral segments. With or without scoliosis, chronic bone erosion. | Most common intramedullary tumor in adults (60% of glial neoplasms). Adults > children. Intramedullary ependymomas involving the upper spinal cord often are cellular or mixed histologic types, whereas ependymomas at the conus medullaris or cauda equina usually are myxopapillary. Slight male predominance. Usually are slow-growing neoplasms associated with long duration of neck or back pain, sensory deficits, motor weakness, bladder and bowel dysfunction. |
Ganglioglioma | Circumscribed intramedullary tumors. Association with scoliosis (44%) and bone erosion (93%). | Rare tumors involving the spinal cord (1% of spinal neoplasms). May extend inferiorly from lesion in cerebellum, ganglioglioma (contains glial and neuronal elements), ganglioneuroma (contains only ganglion cells), gangliocytoma (contains only neuronal elements). Uncommon tumors, patients younger than 30 y, slow-growing neoplasms. |
Hemangioblastoma | Circumscribed tumors usually located in the superficial portion of the spinal cord; small contrast-enhancing nodule, with or without cyst, or larger lesion with prominent heterogeneous enhancement with or without vessels within lesion or at the periphery. Usually associated with syrinx. Locations: thoracic spinal cord (50%–60%), cervical spinal cord (40%–50%). | Represent ~5% of spinal cord neoplasms. Usually intramedullary lesion but occasionally extends into the intradural space or extradural location. Sporadic lesions usually occur in patients younger than 40 y. Multiple lesions occur in adolescents with von Hippel–Lindau disease. |
Metastasis | Intramedullary lesion or superficial lesions on the spinal cord, with or without leptomeningeal tumor nodules. Often extend two or three vertebral segments. | Rare intramedullary lesions that can present with pain, bladder or bowel dysfunction, and paresthesias. Location: cervical spinal cord (45%), thoracic spinal cord (35%), lumbar region (8%). Usually solitary lesions, occasionally multiple; spread hematogenously via arteries or direct extension into leptomeninges with invasion of pial surface or central canal of the spinal cord. Primary CNS tumors include primitive neuroectodermal tumor/medulloblastoma, glioblastoma. Primary tumors outside CNS: lung carcinoma (70%), breast carcinoma (11%), melanoma (5%), renal cell carcinoma (4%), colorectal carcinoma (3%), lymphoma (3%), others (4%). |



Related posts:
 10 Computed Tomography of Spinal Abnormalities
10 Computed Tomography of Spinal Abnormalities
 10 Computed Tomography of Spinal Abnormalities(Table 10.1 – Table 10.2)
10 Computed Tomography of Spinal Abnormalities(Table 10.1 – Table 10.2)
 10 Computed Tomography of Spinal Abnormalities(Table 10.3 – Table 10.4)
10 Computed Tomography of Spinal Abnormalities(Table 10.3 – Table 10.4)
 1 Brain and Extra-axial Lesions(Table 1.1 – Table 1.2)
1 Brain and Extra-axial Lesions(Table 1.1 – Table 1.2)
 15 Trauma and Fractures: Shoulder Girdle and Upper Extremity
15 Trauma and Fractures: Shoulder Girdle and Upper Extremity
 24 Gastrointestinal Tract
24 Gastrointestinal Tract
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


