Introduction
Foreign bodies are uncommon, but they are important and interesting. Sometimes, they may provide a great deal of low-brow amusement. Foreign bodies may be ingested, inserted into a body cavity, or deposited into the body by a traumatic or iatrogenic injury. They may go unrecognized or mistaken for a normal structure or a normally functioning medical device. Because of this, they can cause harm to the patient.
Most ingested foreign bodies pass through the gastrointestinal tract without a problem. Most foreign bodies inserted into a body cavity cause only minor mucosal injury. However, ingested or inserted foreign bodies may cause bowel obstruction or perforation; lead to severe hemorrhage, abscess formation, or septicemia; or undergo distant embolization.
Motor vehicle accidents and bullet wounds are common causes of traumatic foreign bodies. Metallic objects, except aluminum, are opaque, and most animal bones and all glass foreign bodies are opaque on radiographs. Most plastic and wooden foreign bodies (cactus thorns, splinters) and most fish bones are not opaque on radiographs.
All patients should be thoroughly screened for foreign bodies before undergoing a magnetic resonance imaging study. This screening may consist of a detailed questionnaire filled out by the patient, a detailed medical history obtained by the MRI technologist, or possibly radiographs to look for a suspected foreign body, such as a tiny piece of metal in the eye.
The interpretation of ultrasonographic (US), computed tomographic (CT), and magnetic resonance (MR) imaging studies is particularly fraught with error if one does not appreciate the presence of a medical device or a foreign body. It is crucial that all US, CT, nuclear medicine, and MR images be interpreted in light of any current radiographic studies of the same body region. The scout image obtained for CT and MR imaging studies should be examined carefully for unexpected foreign bodies and medical apparatus and for unexpected bone, bowel, and soft-tissue lesions not easily visualized on cross-sectional images.
Appearance of Foreign Bodies on Radiographs
| Category | Description |
|---|---|
| Opaque materials | Glass of all types; most metallic objects except aluminum; most animal bones and some fish bones; some foods; some soil fragments; some medications and poisons (CHIPES: chloral hydrate, condoms, cocaine; heavy metals; iodides, iron; psychotrophics–phenothiazines; enteric-coated pills, barium; and solvents) |
| Non-opaque materials | Most foods and medicines; most fish bones; most wood, splinters, thorns of all types; most plastics; most aluminum objects |
Foreign Body Ingestions
Foreign body ingestions or insertions are seen most commonly in four broad categories of patients: (a) children, (b) mentally handicapped or mentally retarded persons, (c) adults with unusual sexual behavior, and (d) “normal” adults. The latter often have predisposing factors or injurious situational problems. This includes individuals who may abuse drugs or alcohol, engage in criminal activities, engage in extreme sporting activities, or may be subject to child or spousal abuse. Mentally handicapped or mentally retarded individuals are often repeat offenders and will present multiple times for unusual injuries and foreign body insertions and ingestions. On occasion, an adult or child may inadvertently ingest a foreign body with their food or drink. It may not be recognized due its small size and unexpected nature (Gharib et al., 2015).
Foreign Body Ingestions, Basic Principles
| Category | Description |
|---|---|
| General principles | Most foreign objects traverse the GI tract without a problem Elongated or sharp objects (e.g., needles) may impact at a point of intestinal narrowing or bending (e.g., duodenal loop, duodenojejunal junction, terminal ileum, or area of bowel stricture) Always consider esophageal or airway foreign bodies if there is unexplained stridor, drooling, or respiratory distress in a child or mentally impaired individual Always look for a second or third foreign body after the first foreign body – never rest: examine the entire GI tract from the base of the skull to the anus |
| Predisposed patients | Infants and young children Mentally incapacitated individuals Individuals with reduced palatal sensitivity due to denture use, advanced age, or excessive drug and alcohol use Those ingesting especially hot or cold liquids Persons with poor vision who eat rapidly |
| Complications | Esophageal or intestinal perforation or obstruction Peritonitis, mediastinitis, abscess formation Generalized septicemia |
Foreign body ingestions are common in children and mentally handicapped adults. Typical examples include children swallowing coins and mentally handicapped adults swallowing razor blades and silverware. Fortunately, the vast majority of all swallowed objects pass through the gastrointestinal tract without a problem (Table 10.2; Figures 10.1–10.8).
Figure 10.1 28-year-old woman who periodically swallowed pins and razor blades. The open safety pin in her descending colon passed without mishap.
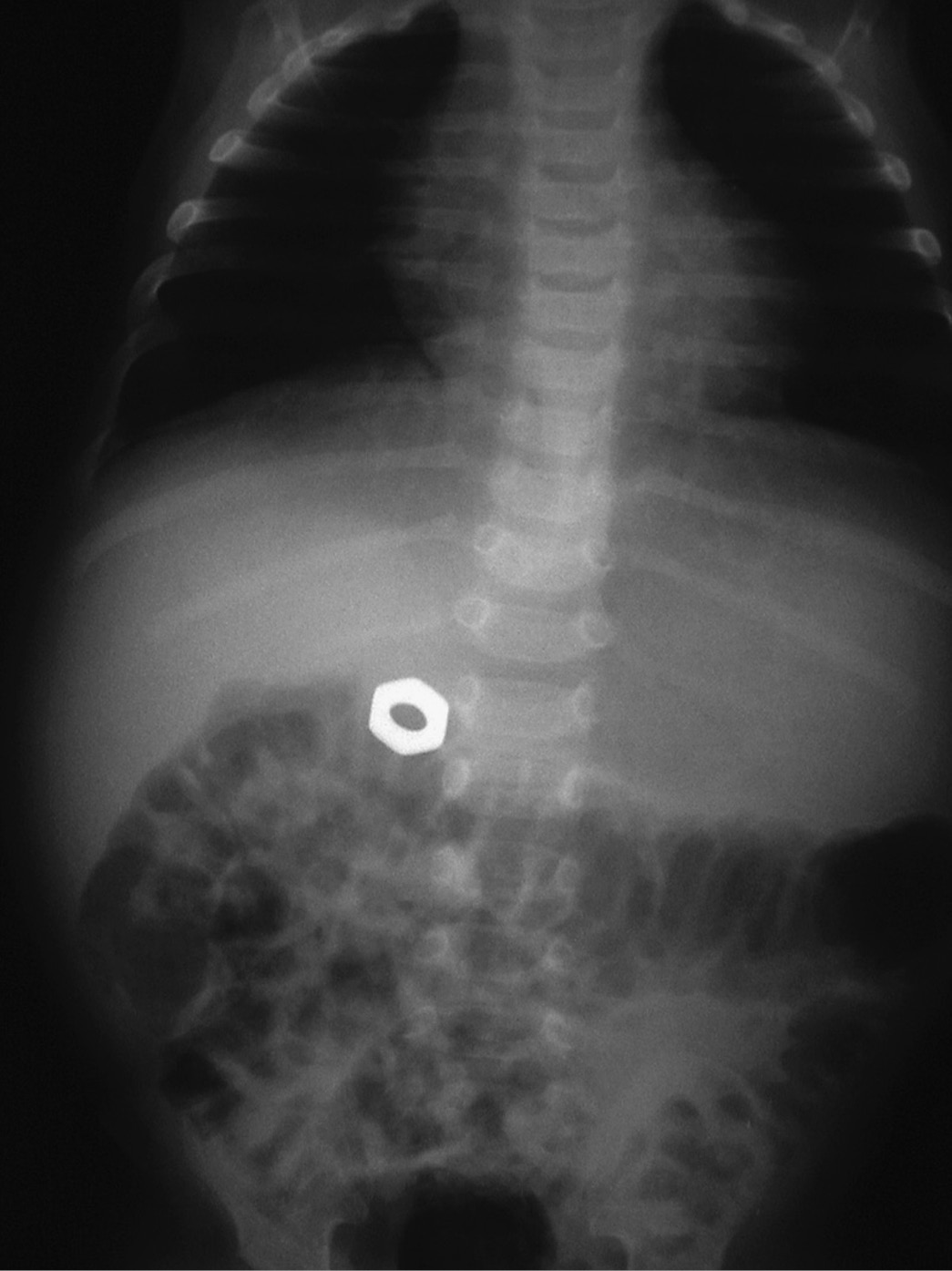
Figure 10.2 Small child who swallowed a metal nut.
Figure 10.3 Box cutter blade in descending colon.
Figure 10.4 15-year-old mentally incapacitated child who periodically swallowed objects. This radiograph shows a safety pin and key in the jejunum and rubber flexible Khrushchev doll head in the descending colon. It passed without difficulty.
Figure 10.5 The arrows show a pencil lodged in the ascending colon. It passed without difficulty which is unusual for such an elongated object.
Figure 10.6 Elderly patient with a coffee cup fragment lodged in the distal esophagus.
Figure 10.7 Quarter in hypopharynx. 35-month-old infant who swallowed a quarter. (A) Frontal view of the chest. (B) Lateral view of the neck.
Figure 10.8 Pill bottle lodged in proximal esophagus. Radiograph (A) and images (B,C) from a barium swallow of a 62-year-old man who accidentally ingested a pill bottle cap while taking his medications. The cap was lodged in his proximal esophagus. It was removed at endoscopy.
Elongated or sharp objects, such as needles, eating utensils, bobby pins, or razor blades, are more likely to lodge at areas of narrowing (from bowel adhesions or strictures) or to impinge at regions of anatomic acute angulation (Figure 10.5). The duodenal loop, duodenojejunal junction, appendix, and ileocecal valve region seem to be more predisposed to impaction from these types of objects (Balch & Silver, 1971; Eldridge, 1961; Himadi & Fischer, 1977; Maglinte et al., 1979; Maleki & Evans, 1970; McPherson et al., 1957; Price et al., 1988; Schwartz & Polsky, 1976; Segal et al., 1980; Selivanov et al., 1984).
Large spherical or cylindrical objects may pass through the esophagus only to be halted at the pylorus (Muhletaler et al., 1980). Some large rounded objects (e.g., coins, meat) can impact at the thoracic inlet, the gastroesophageal junction or an area of stricture (Figures 10.8–10.13) (Bunker, 1962; Chaikhouni et al., 1985; Hunter, 1991; Jackson, 1957; Nandi & Ong, 1978; Vizcarrondo et al., 1983). The indications for foreign body removal by endoscopy or surgery vary depending on local experience, as do suggested radiographic protocols for monitoring the progress of foreign body passage through thegastrointestinal tract, although broad general principles have been published (Guelfguat et al., 2014; Ikenberry et al., 2011; Webb, 1995).
Figure 10.9 Metallic mercury in the appendix of an asymptomatic patient from rupture of mercury bag on a Miller–Abbott tube.
Figure 10.10 72-year-old man with no symptoms. BBs are in the appendix. He used to eat BBs as child.
Figure 10.11 (A,B). Sequential radiographs of a 4-year-old girl who ingested a watch battery show it first in the stomach (A) and later in the transverse colon (B). The battery passed without complications.
Figure 10.12 A 3-year-old boy swallowed four cylindrical magnets, which were evident in his stomach (A). The next day they were in the sigmoid colon (B) and passed with no patient harm.
Figure 10.13 Soft-tissue neck radiograph of a 1-year-old girl who was coughing after swallowing a red coin-like plastic wafer. The plastic is lodged in her hypopharynx (arrowheads). She coughed it up a few minutes later. Most plastic objects are not visible on radiographs.
Appendicitis
The occurrence of appendicitis secondary to an impacted foreign body is an interesting although rare occurrence (Balch & Silver, 1971; Price et al., 1988). There are reports of appendicitis, appendical perforation, and appendical abscess formation months to years after the ingestion of a foreign body. Appendicitis is a common disease, and its association with a foreign body may be coincidental. It is certainly well known that small rounded objects, such as lead shot, BBs, barium, and mercury globules can reside in the appendix for years without apparent effect (Figures 10.9 and 10.10).
It is probable that sharp objects such as toothpicks and pins are more likely than small rounded objects to induce appendix inflammation or perforation. In general, small rounded objects are probably harmless as far as the appendix is concerned. Larger rounded objects such as an airgun pellet lodged in the appendix may predispose a patient to appendicitis. However, if a large rounded foreign body is discovered in the appendix in an otherwise asymptomatic patient, there is no consensus on whether there should be elective surgery to remove the object and the appendix (Price et al., 1988).
Disk Batteries; Cylindrical Magnets
Disk (button) batteries such as those used in watches, calculators, hearing aids, and cameras are potentially very hazardousif ingested (Figure 10.11). Because of their small size and resemblance to a dime, watch batteries are attractive to children and mentally incapacitated persons. They are seemingly harmless because their small rounded contour should permit easy passage through the gastrointestinal tract, and in fact, most of them pass without difficulty. However, they can cause grave injury or even death. Batteries contain a variety of alkaline corrosive agents, such as aqueous potassium hydroxide, and heavy metals, such as mercury and cadmium. If their containers fracture, they can spill their caustic content, which may lead to perforation and systemic toxicity from heavy metal poisoning.
The treatment for watch battery ingestion is controversial (Ikenberry et al., 2011; Jaffe & Corneli, 1984; Kuhns & Dire, 1989; Studley et al., 1990). Most authorities avoid surgery or endoscopy in routine cases in which the battery is found in the stomach. Any evidence for lack of progression through the gastrointestinal tract is cause for concern and probable intervention. Batteries usually can be removed from the esophagus, stomach, and duodenum by endoscopy- or fluoroscope-directed interventional techniques with magnets (the battery case contains nickel and is magnetic), Foley catheters, forceps, or some type of retrieval basket (Jaffe & Corneli, 1984; Shaffer et al., 1986; Volle et al., 1986). Disk batteries impacted in the esophagus are considered to be especially dangerous and should be removed promptly (Ikenberry et al., 2011).
Small cylindrical magnets, such as those used to hold notes on a refrigerator door (Figure 10.12), are seemingly harmless and may pass through the gastrointestinal tract without mishap. These magnets may be especially high-powered and are often composed of neodymium. They are sometimes known as “rare earth” magnets and are often available as desk “toys” and “stress relievers” with many small magnets clustered as balls, cubes, cylinders, or other objects. They are marketed for adults only, but they can get in the hands of young children or mentally incapacitated adults (Brown et al., 2013).
If more than one magnet has been ingested, they may cause severe harm to the gut. One or more of the magnets may be attracted to the others by their magnetic pull and tear or perforate the mucosa of the stomach or intestinal tract by pressure necrosis, leading to fistula formation, volvulus, perforation, and severe hemorrhage if mesenteric vessels are trapped between magnets in different portions of the bowel. A particularly worrisome finding is a gap between magnets on radiographs (Guelfguat et al., 2014). The magnets may entrap bowel wall between them, leading to pressure necrosis. They can also lodge in the hypopharnyx, distal esophagus, or at other points of narrowing in the bowel. Endoscopy or other intervention is recommended if a cylindrical magnet is lodged in the esophagus or if cylindrical magnets do not show rapid progression out of the stomach and through the small and large bowel (see Foreign body ingestions in children).
Plastic Clips; Pull Tabs
Another seemingly innocuous but potentially extremely dangerous ingested foreign body is the plastic clip used to close plastic bags, such as those for bread packages (Figure 10.13). These plastic clips have been noted to grip various portions of the bowel mucosa, producing inflammation and ulceration and eventually leading to severe complications – perforation, obstruction, intussusception, fistula formation, abdominal abscess formation, and death (Bundred et al., 1984; Guindi et al., 1987; Jamison et al., 1983; Rivron & Jones, 1983; Sutton, 1984). Unfortunately, these clips are usually not opaque on radiographs and are difficult to detect. They may become encrusted with mineral or bile salts and thereby are rendered opaque.
Less than 1% of ingested foreign bodies cause perforation of the gastrointestinal tract. Sharp, elongated objects are the most likely to penetrate the bowel or esophageal mucosal lining and cause significant injury to the bowel wall or frank perforation (Ashby & Hunter-Craig, 1967; Danielson & Hunter, 1985; Guelfguat et al., 2014; Gunn, 1966; Maglinte et al., 1979; Ngan et al., 1990; Schwartz & Graham, 1977; Ziter, 1976). Perforations are more common in the ileocecal region, especially in a Meckel diverticulum or the appendix. Metallic objects such as needles or elongated objects such as fish bones, chicken bones, and toothpicks are the foreign bodies most frequently reported to have caused a perforation (Gharib et al., 2015).
In many cases, these perforations do not occur acutely or cause acute symptoms. The object may only partially perforate the bowel wall and produce a chronic inflammatory process that has few symptoms, being discovered months or years later. Sometimes, these chronic inflammatory processes are discovered when they produce unusual areas of opacity or lucency on radiographs obtained for other reasons. Sometimes, they are discovered at abdominal surgery performed for another reason. Even at surgery, the foreign body may be hard to diagnose because of its encrustation by bile and mineral salts.
Almost all objects composed of plastic and most thin aluminum objects, such as pull tabs on cans, are not radiopaque (Table 10.1). On the other hand, all chicken bones and most meat bones are opaque on radiographs (Figures 10.14–10.18), whereas the majority of fish bones are not, although some fish bones are readily evident. Glass is always radiopaque, and its radiopacity does not depend on its lead content or other metal content (Fornage & Schemberg, 1986; Gordon, 1985; Tandberg, 1982). Glass foreign bodies, whether ingested, inserted into a body cavity, or deposited in the soft tissues of an extremity by an injury, should always be visible on radiographs. This visibility obviously depends on the size of the object. Submillimeter pieces of glass buried deep in the soft tissue of an obese person may not be visible. However, any substantial piece of glass 1–2 mm or larger should generally be visible.
Figure 10.14 81-year-old man who swallowed a turkey bone (arrows). It is located just posterior to the cricoid cartilage. The bone could not be seen at direct laryngoscopy, but was removed at endoscopy.
Figure 10.15 Xeroradiograph of an elderly man with painful swallowing after eating a bowl of “oxtail soup.” There is an impacted piece of bone lying anterior to the 7th cervical vertebra. Note the prominently calcified posterior margin of the cricoid bone (arrow). This normal variant should not be mistaken for a foreign body. The impacted bone fragment was removed from the proximal esophagus at endoscopy.
Figure 10.16 68-year-old man with difficulty swallowing after eating fish. A bone (arrow) had perforated the hypopharyngeal wall and was lodged in the soft tissues of the neck. Indirect laryngoscopy was negative, and the bone was removed at surgery after an unsuccessful endoscopy.
Figure 10.17 36-year-old woman with painful swallowing after eating chicken. (A) A small calcific density (arrowhead) represents a lodged chicken bone. (B) A radiograph after the woman swallowed a barium capsule shows it temporarily lodged at the point of obstruction. The bone was impacted in her proximal esophagus and removed at rigid endoscopy.
Figure 10.18 Radiograph of an adult who was in the habit of swallowing rubber gloves. The mottled lucent area (arrow) in the right lower quadrant represents a rolled-up rubber glove in the terminal ileum. It has a similar appearance to swallowed drug packets.
Coins
Often radiologists and other physicians are not aware that aluminum is relatively radiolucent, unlike most other common metals. Ingested or inhaled aluminum objects are not easily detected on radiographs. The US federal government actually abandoned plans to produce an aluminum penny, because many physicians pointed out the danger to children if a common coin were radiolucent (Dorst et al., 1982; Eggli et al., 1986; Heller et al., 1974).
Coin ingestions are common in children and would be hard to diagnose if coins were not readily apparent on radiographs. Although most coin ingestions cause no harm, with the coin passing through the gastrointestinal tract in a few days, coins may enter the airway or become impacted at the thoracic inlet or the gastroesophageal junction. In these cases, intervention is required. The diagnosis of coin ingestion could be significantly delayed if radiolucent coins were common. In fact aluminum pull tabs and Italian lira are radiolucent and have caused difficulty in the diagnosis of esophageal perforations.
Coin ingestions are generally benign, but it is possible for zinc toxicity to develop if a large number of pennies are ingested. Pennies produced after 1981 consist mainly of zinc. There are at least two reports of schizophrenic patients ingesting massive amounts of pennies with resultant systemic symptoms of zinc poisoning from the caustic partial digestion of the pennies in the stomach and bowel (Dhawan et al., 2008; Pawa et al., 2008).
The diagnosis of an ingested foreign body is often overlooked in those patients who cannot furnish an adequate history or who have swallowed objects that are not inherently opaque (Berger et al., 1980; Chaikhouni et al., 1985; Eldridge, 1961; Humphry & Holland, 1981; Jackson, 1957; Nandi & Ong, 1978; Schwartz & Polsky, 1976; Smith et al., 1974). In selected cases, contrast material studies with barium tablets, barium capsules (Figure 10.17), barium impregnated cotton balls, or barium-coated food may be useful. CT of the abdomen or chest may be helpful, particularly if an unusual area of opacity or lucency is found at radiography, and the diagnosis of a perforating foreign body is entertained (Guelfguat et al., 2014). Correlation of the CT findings with radiographic findings and careful examination of the scout image is critical for diagnosing foreign bodies or unexpected medical devices.
Young children with an esophageal foreign body may present with mainly respiratory symptoms and may not volunteer a history of foreign body ingestion. Stridor, wheezing, and pneumonia can be unsuspected sequelae from an ingested, impacted foreign body in the hypopharynx, esophagus, or respiratory tree (Figures 10.19–10.23) (Berger et al., 1980; Humphry & Holland, 1981; Smith et al., 1974).
Figure 10.19 8-month-old boy with vague respiratory symptoms. Lateral view of the chest shows a thin, twisted metallic foreign body. A piece of wire was removed from his hypopharynx at endoscopy.
Figure 10.20 2-year-old girl with severe respiratory symptoms. She had a left-sided pneumonia and empyema requiring a tracheostomy. For several days the ring-like metallic density noted on her portable chest radiograph was assumed to be associated with her tracheostomy. The lateral (A) and frontal (B) chest radiographs reveal the metallic density is not associated with the tracheostomy. A bingo chip was removed at endoscopy.
Figure 10.21 37-year-old mentally disabled woman who was admitted comatose with a 24-hour history of difficulty breathing. An open safety pin had perforated the wall of her esophagus and penetrated her larynx. It was extracted at laryngoscopy, and she recovered without sequelae.
Figure 10.22 13-year-old boy with a pin in his trachea. He had been playing with a blowgun and inhaled a corsage pin. It was removed at bronchoscopy
Figure 10.23 Foreign body in unsuspected location. Whenever there is a plausible history of a foreign body ingestion, the patient should be examined from the base of the skull to the anus. (A) This radiograph shows no opaque body in the chest or stomach of an 8-year-old boy who was reported to have swallowed a foreign object. The radiologist asked for a repeat radiograph (B) to include all the abdomen and pelvis. There is a metallic tweezer in the child’s distal small bowel.
Whenever there is a history of a foreign body, whether in an adult or a child, more than one object should be suspected and looked for. The patient should be examined from the base of the skull to the anus (Figure 10.23). Often, there is ingestion of more than one object, and the search for foreign bodies should not be suspended just because one has been found. Children are especially prone to ingest objects in multiples.
Drug Packets; Medications
We live in a world plagued by illicit drug traffic and use in which the importation of illegal drugs is a major industry. Some of the bit players in this trade are the “mules” or “body packers,” who smuggle drugs by ingesting drug-filled packets or by inserting them into their rectum or vagina. These packets are usually filled with cocaine, although heroin is also common. The packing material is typically a condom or balloon, and the packets vary in their relative opacity. Some are opaque, whereas others are equal in opacity to or less opaque than the bowel (Beerman et al., 1986;).
On serial abdominal radiographs (Figure 10.24), these packets may be detected by observing a definite crescent of air surrounding an ovoid area of opacity. This finding is sometimes called the double-condom sign. The packets may also be noted as multiple, well-defined areas of opacity in the stomach, small intestine, or colon. They may have a rosette configuration at one end. Recent work suggests low-dose unenhanced multidector CT (MDCT) without bowel preparation is an excellent means for detecting ingested cocaine-filled packets (Poletti et al., 2012; Schmidt et al., 2008). It is probably superior to abdominal radiography (Laberke et al., 2016).
Figure 10.24 Radiographs of adults who were smuggling drugs. A packet is visible in the transverse colon (arrow in A). Relatively dense packets are visible in the transverse and descending colons in B and C.
The main medical complications from this type of smuggling are bowel obstruction and acute drug toxicity. Bowel obstruction occurs in slightly less than 10% of documented cases. Acute drug overdose is a very serious risk to the smuggler if one or more of the condoms should rupture. There have been reports of sudden deaths from massive drug overdoses. Considering the large amount of smuggling that no doubt takes place by this means, this complication is rare.
Esophageal and bowel strictures may be produced by improper ingestion of common prescription medications, such as potassium chloride or quinidine preparations. Most of the strictures develop in the middle or proximal esophagus. Risk factors for developing esophageal caustic injury related to medications include older age, male sex, left atrial enlargement, and prior esophageal structural abnormality. Ingestion of sustained release formulations appears to increase the risk for injury (McCord & Clouse, 1990).
Children, mentally incapacitated adults, and suicidal individuals may knowingly or inadvertently ingest poisonous substances. Most medications and toxic agents are probably not opaque enough to be easily detected by routine imaging methods. However, many metals and their compounds are sufficiently opaque to be seen on abdominal radiographs (Figures 10.25–10.29) (Goldfrank et al., 1986; Gray et al., 1989; Hilfer & Mandel, 1962; Spiegel & Hyams, 1984; Staple & McAlister, 1964). These substances include barium, lead, arsenic, bismuth, thorium, and iodine compounds.
Figure 10.25 Sand in the bowel. Young child with a history of eating sand.
Figure 10.26 Lead in the bowel. Radiograph of a typesetter shows opaque lead in his distal colon. He had inadvertently ingested high amounts of lead over a period of years while eating his lunch at the plant. He had very high lead levels in his blood, neurological symptoms, anorexia, and constipation.
Figure 10.27 3-year-old boy who ingested multiple iron tablets probably containing ferrous gluconate and sulphate salts. He recovered without sequelae.
Figure 10.28 Pepto-Bismol. Radiograph showing bismuth subsalicylate (Pepto-Bismol) tablets in the right lower quadrant producing a pseudo-appendicolith appearance.
Figure 10.29 3-year-old girl who ate half-melted crayons which formed a bezoar in the stomach. It required surgical removal.
Sometimes children or mentally incapacitated adults will ingest a substance that is not directly toxic but can lead to bezoar formation in the stomach or cause bowel obstruction (Figure 10.29). There is an accumulation of ingested material which most commonly forms a hard mass or concentration in the stomach. Diabetes with poor gastric emptying, peptic aciddisease with gastric scarring, prior partial gastric resection, or medication which slows gastric emptying may be causal factors in the development of a gastric bezoar. Bezoars are generally classified according to their composition (See Foreign bodies of the esophagus and gastrointestinal tract in children). Phytobezeoars are composed of vegetable material, those being caused by persimmons are the classic example of a phytobezoar. Trichobezoars are composed of hair, and those patients with a trichobezoar often have an underlying psychiatric illness.
Iron poisoning is the leading cause of poisoning-related deaths in young children (Morris, 2000). Medications containing iron are widely used, and many adults do not appreciate the potential toxicity of iron tablets. The US Food and Drug Administration requires the following statement on packages for preparations that contain iron or iron salts for dietary supplemental or therapeutic purposes: “WARNING: Accidental overdose of iron-containing products is a leading cause of fatal poisoning in children under six. Keep this product out of reach of children. In case of accidental overdose, call a doctor or poison control center immediately” (FDA).
Severe iron poisoning results in hemorrhagic gastroenteritis followed by a significant blood chemistry imbalance and subsequent multiorgan damage. Iron tablets that are intact, fragmented, or in a coarse powder form are usually visible in the stomach and small bowel (Figure 10.27). However, iron preparations that are dissolved or form a fine suspension may not be sufficiently radiopaque to be recognizable. Thus, although potentially helpful, abdominal radiography may not permit the diagnosis of iron ingestion or allow it to be convincingly ruled out. Also, abdominal radiography should not be relied on to gauge the success of efforts to remove iron from the gastrointestinal tract.
Although most poisonous substances are not sufficiently opaque to be visible on radiographs, many industrial solvents, such as carbon tetrachloride, are radiopaque. Most medications are radiolucent and will not be visible on radiographs. However, bismuth subsalicylate (Pepto-Bismol) is sufficiently opaque to be visible throughout the gastrointestinal tract if it has been ingested in a sufficient amount (Figure 10.28).
Some other medications, such as chloral hydrate, the phenothiazines, and many enteric-coated pills, are radiopaque as well. CHIPES (chloral hydrate, condoms, cocaine; heavy metals; iodides, iron; psychotrophics–phenothiazines; enteric-coated pills, barium; and solvents) is a good mnemonic for remembering classes of radiopaque ingested compounds (Spiegel & Hyams, 1984).
Endoscopic Capsules
Many small bowel diseases are diagnosed or evaluated by (video) capsule endoscopy (VCE). Clinical applications include workup of obscure gastrointestinal bleeding and iron-deficiency anemia, detection of small bowel polyps and tumors, and evaluation of celiac disease, Crohn’s disease, and other inflammatory bowel diseases (Mustafa et al., 2013; Neuman et al., 2014;). VCE may be particularly indicated when gastroscopy or colonoscopy fail to find the source of gastrointestinal bleeding.
VCE can be dangerous and even contraindicated in any situation where there is risk of retention or small bowel obstruction. Contraindications include pregnancy, patients with a swallowing disorder, history of previous abdominal surgery, or any other situation in which there is potential narrowing of the bowel lumen. Capsule retention is a feared complication of VCE occurring in up to 20% of patients with symptoms of chronic small bowel obstruction (Singeap et al., 2011). In a more diverse population of patients, 2.1% experienced capsule retention, and surgical or endoscopic retrieval was necessary in 1% (Rondonotti et al., 2010). The endoscopic capsules can be retained for long periods with minimal patient discomfort, and many eventually pass on their own. The decision to endoscopically or surgically remove a retained endoscopic capsule depends on the individual patient circumstance, although on rare occasions they may cause or worsen acute bowel obstruction or lead to bowel perforation. A retained endoscopic capsule is a contraindication for MRI (MRI Safety Information).
Foreign Body Insertions
No matter the body opening, there are individuals who will attempt to insert something into it themselves or allow others to insert a foreign object into it. The rectum, vagina, urethra, nose, and ear are favorite sites for insertion of foreign objects. These types of insertions are most frequently seen in children, but adult patients may derive sexual pleasure from it, be mentally incompetent, or do it merely out of curiosity (Table 10.3; Figures 10.30–10.37).
Figure 10.30 Young child who had placed a screw in her vagina resulting in chronic vaginitis.
Figure 10.31 A 2-year-old girl had placed a bobby pin in her bladder.
Figure 10.32 Pen refill in urethra. Young man who had inserted a pen refill in his urethra with partial rupture of the urethra and soft tissue gas in the penis.
Figure 10.33 15-year-old boy with a broken rectal thermometer lying free in the peritoneum. Its origin was unknown. He denied inserting any foreign objects into his rectum or urethra. He had had no treatments or hospitalization since he was one year old.
Figure 10.34 19-year-old woman with a bobby pin lodged in her uterus. She had attempted to induce an abortion with the bobby pin. A subsequent self-induced abortion was successful.
Figure 10.35 Young woman with multiple “piercings” including an umbilical ring and labial rings.
Figure 10.36 18-year-old man with bladder calculi that formed around a wire in his bladder. Six months prior he lost a fine telephone wire in his bladder when he achieved an erection while inserting the wire into his urethra during masturbation.
Figure 10.37 60-year-old man with a condensed milk can that he had inserted into his rectum.
Foreign Body Insertions: General Principles
| Category | Description |
|---|---|
| General principles | Most insertions cause no harm Minor mucosal injuries are common Retained objects may be encrusted with mineral salts Retained objects may perforate and travel to distant sites |
| Predisposed patients | Children (especially those with emotional problems) Mentally incapacitated individuals Adults engaging in “unusual” sexual activities Patients undergoing surgery or instrumentation Patients undergoing non-traditional medical therapy |
| Complications | Severe bleeding from mucosal injury Edema preventing natural passage or easy removal Organ perforation with hemorrhage, abscess formation, or sepsis |
Rectal, urethral, or bladder foreign bodies are usually purposefully introduced by the patient himself or herself, although occasionally they are the result of a penetrating injury, past surgery, or past instrumentation (Barone et al., 1976; Busch & Starling, 1986; Classen et al., 1975; Crass et al., 1981; Fuller, 1965; Kraker, 1935; Lebowitz & Vargas, 1987; Maddu et al., 2014; Rebell, 1948; Rosser, 1931). Their occurrence is more frequent in children or adults with mental illness.
Bladder foreign bodies are particularly prone to being a site for deposition of mineral salts with the formation of one or more bladder calculi (Figure 10.36) (Lebowitz & Vargas, 1987). In fact, a bladder calculus in a child or young adult should raise the suspicion of an encrusted foreign body.
Surprisingly, most foreign bodies inserted into the urethra or rectum do not cause significant injury even if they are large, sharp, or pointed (Figures 10.38–10.44). These tubular structures are capable of considerable expansion, and they are well-lubricated by natural fluids. Patients also learn how to “dilate” these structures so that they will accommodate large objects (Figures 10.37 and 10.38). The most common complications of a rectal foreign body are retention and rectal bleeding. The most serious complication is perforation either related to the foreign body insertion or the attempts to remove it (Yildiz et al., 2013).
Figure 10.38 Policeman who somehow lost his traffic wand in his rectum.
Figure 10.39 25-year-old man who sat on a dildoa.
Figure 10.40 Drinking glass in the rectum.
Figure 10.41 Cigarette lighter in the rectum.
Figure 10.42 Cordless screwdriver in the rectum.
Figure 10.43 Bottle in Hartman pouch. 51-year-old man with bottle of gargling fluid in his Hartman pouch which had been placed three weeks previously after he had distal colon surgery to remove an impacted shampoo bottle.
Figure 10.44 Ship in bottle in rectum.
Common rectal foreign bodies that result from medical procedures going awry include thermometers, rectal tubes, anal packs, light covers, enema tips and covers, suppository wrappers, and oral or topical medication used inappropriately in the rectum (Zelegman et al., 1986).
The supine view of the abdomen is often the first radiograph obtained to evaluate a patient with abdominal or pelvic pain with or without a history of foreign body insertion. If the object lies in the bladder, it will generally be oriented mediolateral. If it lies in the vagina or rectum, it will generally be oriented craniocaudally. This rule is probably more applicable in children than in adults, because vaginal foreign objects may lie mediolateral in adults. Oblique and lateral radiographs of the pelvis as well as endoscopy and cross-sectional studies (mainly ultrasound and CT) can help determine the exact location of a foreign body. CT is recommended if a colonic foreign body is proximally located or cannot be removed manually (Maddu et al., 2014).
Cleansing enemas are sometimes a source of complications for patients. There can be mucosal injury from the enema fluid being too hot or too caustic. The enema tube or its protective sheath may be retained in the rectum or sigmoid or the mucosa may be lacerated and perforated. Small, retained colonic foreign bodies usually pass spontaneously. Large ones may induce enough wall edema or bowel atony so that they cannot be passed naturally. In such instances, they must be removed endoscopically; by perianal extraction with the patient under anesthesia; or surgically, with either direct removal of the object from the bowel or with laparotomy and anal removal of the object (Eftaiha et al., 1977; Richter & Littman, 1975; Wolf & Geracy, 1977).
Retained rectal bodies may rarely form asymptomatic calcified fecaliths. More commonly, they cause acute and chronic discomfort and can produce severe bleeding, bowel obstruction, and perforation. Retained objects can also ascend higher into the colon, even as far as the hepatic flexure. If they perforate the colon, they may lodge in the retroperitoneal tissues, induce localized contained abscesses, lie free within the peritoneum, or even travel to distant sites in the body (Buzzard & Waxman, 1979; Eftaiha et al., 1977; Lau & Ong, 1981; Morales et al., 1983).
Foreign Body Injuries
Even the most sheltered individual has a life filled with a multitude of minor injuries, including falls, cuts, abrasions, scratches, and burns. Everyone has suffered puncture wounds from splinters, needles, and thorns and has been cut with glass. The entire range of possible foreign body injuries cannot be covered herein. However, it is possible to illustrate many common types of accidents and point out general principles concerning these injuries (Table 10.4).
Jewelry, clothing, and items lying on a patient, or in a patient’s clothing, may simulate a foreign body (Figures 10.45–10.48). When viewing or interpreting imaging studies, one should always take care to identify all objects seemingly in or on a patient, including medical devices, foreign bodies, and generally innocuous items which simulate a medical device or foreign body.
Figure 10.45 Decorative design on underwear simulates a vaginal or bladder foreign body.
Figure 10.46 Buckshot bra. A woman’s bra is packed with metallic shot to make her breasts appear larger.
Figure 10.47 E-cigarette. 64-year-old woman who had postoperative bowel obstruction. A supine view of the abdomen shows an e-cigarette the patient had hidden in her hospital gown.
Figure 10.48 These earrings resemble cervical spine apparatus on the lateral view (A). The frontal view (B) shows their true nature.
Foreign Body Injuries: General Principles
| Category | Description |
|---|---|
| General principles | Diagnosis may be difficult and require CT, US, or other techniques to identify non-opaque foreign bodies |
| Predisposed patients | Children and mentally incompetent adults Individuals with a history of recent trauma who cannot furnish a history Individuals who undergo instrumentation, surgery, or non-conventional medical treatments Individuals who have “unusual” sexual practices, engage in wizardry or sorcery, abuse drugs or alcohol, or engage in criminal activities Victims of physical abuse or terrorist attack; military personnel; individual with hazardous occupations – police and fire protection, heavy industry, construction, mining |
| Complications | Pain, swelling, tenderness, cellulitis, abscess formation, sepsis, migration of foreign object to distant locations with potential vascular or nerve injury |
Bullets
Bullet wounds are far too common in the United States (Figures 10.49–10.54). A detailed review of these injuries isbeyond the scope of this discussion except for a few general comments from more extensive reviews on the subject (Dodd & Budzik, 1990; Hollerman & Fackler, 1994; Wilson, 1999). Handguns usually fire relatively “low-velocity” single bullets with speeds less than 2000 ft/s (610 m/s). Rifles typically fire high-velocity solitary bullets with speeds above 2000 ft/s (610 m/s). Shotguns usually fire multiple metallic pellets (BBs, buckshot, or birdshot). The most common shotguns are 12 and 20 gauge. Gauge describes the number of lead balls fitting the shotgun barrel that total one pound (0.45 kg) in weight in a 0.410 inch bore (internal diameter) barrel (Dodd & Budzik, 1990).
Figure 10.49 Young man shot in the foot with a handgun. There is a fifth metatarsal fracture and deformed bullet fragment. The BB overlying the cuboid is from a remote injury.
Figure 10.50 Young man with multiple pieces of shrapnel in the hand after gunshot injury.
Figure 10.51 Bullet debris. Young man shot in the knee with multiple bullet debris in the soft tissues about the knee as well as in the knee joint.
Figure 10.52 Young man who accidentally shot himself in the chest and right arm with a shogun. (A) The scout view from a chest CT shows multiple pellets in the right shoulder and right chest wall with contusion of the right upper lobe. A right chest tube, an endotracheal tube, and a nasogastric tube are in place. (B) A CT image of the lower portion of the chest shows an inferior pellet in the right ventricle. It had penetrated the right subclavian vein and embolized to the right ventricle. It was visible bouncing in the right ventricle when fluoroscopy was performed during right upper extremity angiography. The pellet was successfully removed at cardiac catheterization.
Figure 10.53 Transverse ultrasound image of an elderly man with a bullet (arrow) in his liver. He had a history of a gunshot wound many years previously, and the bullet was an incidental finding.
Figure 10.54 A bullet in the left breast from an old injury was incidentally noted on mammography.
Bullets are often described by their caliber, which is a measurement of their diameter in inches or in millimeters or the internal diameter (bore) of the gun barrel holding the bullet, such as 22 (5.6), 32 (8.1), 38 (9.7), and 45 (11.4) calibers representing, respectively, the hundredths of an inch or (mm) of the bore (Dodd & Budzik, 1990). Although the caliber of a bullet is important, it has only a loose relationship to the weight of the bullet and the size of its charge. Its velocity is also a very important parameter, as its kinetic energy varies by the square of the bullet velocity. Kinetic energy relates directly to how much tissue damage a bullet causes.
Bullets are most commonly composed of lead. They may be fully or partially covered by an outer metal jacket (full metal jacket) that is usually composed of copper. If a bullet has a hollow cavity at its tip (hollow-point bullet), it will deform more on impact and produce more tissue damage. When it comes to rest, a hollow-point bullet typically has a mushroom shape. Bullets are not sterile, and gunshot wounds can deposit live bacteria and other contaminants deep into the body.
Shotgun pellets are measured by their gauge: the larger the number, the smaller the pellet size. Because the pellets are round, they do not travel through air or tissue as well as the more aerodynamically shaped bullets. However, the combined mass of multiple pellets striking someone at a small distance from the gun barrel can cause severe soft-tissue and bone damage – a relatively large mass is decelerated over a short distance, and its kinetic energy is deposited in a small volume of tissue (Figure 10.52).
Shotgun pellets used for hunting were formerly composed of lead. Nowadays, they often have a composition of steel, bismuth, and tungsten. Lead is not ferromagnetic. However, lead pellets left in the environment produce considerable toxic effects on waterfowl. Because steel composite pellets may be ferromagnetic, they may undergo dangerous motion if a patient with imbedded steel shotgun pellets is exposed to a strong magnetic field; therefore, MR imaging may be contraindicated in such patients (Eshed et al., 2010).
It is sometimes possible to distinguish steel and lead pellets from one another at radiography (Wilson, 1999). Lead pellets tend to be deformed and fragmented by impact with soft tissues and bone. Steel pellets usually remain round. Unjacketed bullets are composed of lead and should not cause any problems for MR imaging. On the other hand, some bullet jackets are composed of steel rather than copper. If the nature of the bullet injury is unknown, it may not be safe to perform MR imaging on a bullet wound victim if radiographic findings suggest that the imbedded bullets are jacketed (Eshed et al., 2010; MRI Safety Information; MRIMaster.com; RadiologyInfo.org).
Most lead bullet fragments can be left in place. They usually become encapsulated with fibrous tissue (Figure 10.54). Lead toxicity is a potential problem if the lead fragments are in a joint space, bursal space, or disc space (Figure 10.51). Lead fragments left in a joint space also can lead to a severe, destructive synovitis (Hollerman & Fackler, 1994).
Bones; Metals; Surgical Injuries
Most metallic materials are opaque on radiographs (Figure 10.55). Sometimes clothing or material on a patient will have opaque elements that many simulate a foreign body or a medical device (Figures 10.45–10.48). Many radiologists and referring physicians do not realize that thorns, splinters, wooden fragments, and pieces of plastic are usually not sufficiently opaque to be visualized (Figure 10.56) (deLacey et al., 1985; Gordon, 1985; Spouge et al., 1990).
Figure 10.55 49-year-old man scheduled for knee MRI. History of BB injury to left eye. Frontal (A) and lateral (B) facial views confirm presence of BB in left orbit, possibly in left globe. MRI was contraindicated.
Figure 10.56 Wood in calf. 22-year-old man with large piece of wood (arrows) in his calf after being assaulted with a wooden stake.
On the other hand, animal bones and shells and glass of all types are radiopaque (Figures 10.57 and 10.58) (deLacey, 1985; Gordon, 1985; Tandberg, 1982). The opacity of glass is not related to its lead content; therefore, all substantially large pieces of glass should be visible on radiographs.
Figure 10.57 Barnacles in heel. 17-year-old boy with barnacle fragments in his heel. He had been water skiing when he came into the dock and unexpectedly encountered barnacles, pieces of which lodged into his heel.
Figure 10.58 Glass in forearm. 39-year-old woman who punched a window, receiving a forearm laceration. Frontal (A) and lateral (B) views of the forearm show a large glass foreign body.
The diagnosis of a non-opaque object may be difficult. In selected cases, CT and ultrasound offer hope for visualization of a suspected foreign object in the superficial tissues of the body (Bodne et al., 1988; Fornage & Schemberg, 1986; Gooding et al., 1987; Horton et al., 2001; Meyer et al., 1982; Peterson et al., 2002). At ultrasound, foreign objects frequently give a localized, reproducible hyperechoic appearance (Figure 10.59). Needle localization techniques similar to those used for mammographic needle localization of non-palpable breast lesions before surgical breast biopsy may occasionally aid in the surgical removal of a foreign body from the extremities or other superficial soft tissues of the body.
Figure 10.59 Mesquite thorn at ultrasound. Ultrasound image of a young man who stepped on a broken mesquite tree branch. A large wooden fragment that pierced his foot was removed, but he continued to have pain and swelling over the dorsum of his foot. An echogenic focus was evident on ultrasound (cursors) which proved to be a mesquite thorn at surgery.
Most foreign body injuries to the extremities or other parts of the body involve common daily activities. Motor vehicle accidents and industrial accidents account for the majority of the cases. Infrequently, foreign objects such as bullets may travel a great distance from their original site of entrance into the body (Figure 10.52). It is well recognized that bullets and other foreign bodies may undergo arterial or venous embolization or movement within the subarachnoid space of the head and spine. These possibilities should be considered whenever a bullet is not found on radiographs of the body part predicted to contain it based on the entrance wound and there is no obvious exit wound. Additional radiography, CT, or fluoroscopy should be performed to find the bullet (Hollerman & Fackler, 1994).
Some individuals who practice sorcery or wizardry may insert wires, paper clips, or other objects in themselves to ward off evil spells (Desrentes, 1990). Patients undergoing instrumentation or surgery may experience an iatrogenic injury involving foreign material inserted into the body (Hunter & Hirai Gimber, 2010; Rappaport & Haynes, 1990; Sturdy et al., 1967). Most acupuncture needles are temporarily inserted into the subcutaneous tissues of the body, but they may be deliberately or accidentally left in place (Figure 10.60) (Behrstock & Petrakis, 1974; Glauten & Austin, 1988; Imray & Hiramatsu, 1975; Saenz et al., 1978; Schatz & Fordham, 1976).
Figure 10.60 Acupuncture needles. Acupuncture needles in the paraspinal subcutaneous soft tissues of a 37-year-old Korean woman. The needle fragments were purposefully left in place.
Surgical items placed within or on a patient’s body are common in postoperative patients. Materials normally seen after surgery include large rubber retention sutures; large and small wire sutures; surgical drains; wound gauze packs; bandages; osteotomy bags; skin staples; hemoclips; small surgical staples; hernia mesh; and intravenous, intra-arterial, intraspinal, and intra-abdominal catheters. Other materials, such as retained abdominal sponges and needles, have been accidentally left behind after surgery (Figure 10.61). Fortunately, abnormal retained surgical materials are rare, but they may be difficult to detect clinically and radiographically. This difficulty arises from the often non-specific patient symptoms, poor visibility of the objects on radiographs, and the low suspicion of the radiologist and referring physician for such objects.
Figure 10.61 Retained surgical sponge. Elderly man with right hip pain and a draining sinus tract near the right hip. He had a right hip unipolar prosthesis placed several weeks prior in Mexico. Radiographs of the pelvis and right hip (A) show a unipolar prosthesis as well as a retained surgical sponge (arrow) in the medial aspect of the right acetabulum. The prosthesis was removed and replaced with a temporary antibiotic-impregnated right hip “prosthesis” (B) made from antibiotic laden cement and held in place by press-fitting and cerclage wires.
Although retained surgical sponges are not common, they are dreaded by surgeons and other physicians because of their potential for considerable patient morbidity. Retained sponges are also a frequent source of litigation and bad publicity for physicians. A retained surgical sponge may be discovered immediately near the end of a surgical procedure through a thorough sponge count performed by the nursing staff. If undiscovered at that point, a misplaced sponge may not be found for months to years after surgery (Figures 10.61 and 10.62).
Figure 10.62 Gossypiboma. 25-year-old woman who had undergone a Cesarean section in Mexico. She presented with abdominal pain and fever. The abdominal radiograph shows a large complex, partially lucent left flank mass with an associated linear density. At surgery there was a retained surgical sponge with surrounding area of granuloma formation, a gossypiboma.
Whenever there is the possibility of a missing sponge or other retained surgical foreign body at the end of a surgical procedure, a radiograph of the abdomen and pelvis or affected body part should be obtained to look for the retained object prior to the patient leaving the operating theater (Hunter & Hirai Gimber, 2010; Porter et al., 2015; Walter et al., 2015). Every medical center should develop a policy and procedure for rapid identification of a retained surgical foreign body (Figure 10.63).
Figure 10.63 Surgical sponges used at University Medical Center, Tucson, Arizona, in 2010.
Gossypiboma is the term sometimes used to describe the foreign body reaction to a surgical sponge left within the body for a long period (Figures 10.62 and 10.64). The cotton matrix of the sponge forms the nidus of the foreign body reaction. Around the cotton nidus, there is surrounding fibrosis, retraction, and development of a foreign body granuloma (Sturdy et al., 1967). The frequency of retained surgical foreign material is one per 1000–1500 laparotomies (Rappaport & Haynes, 1990). Many patients are asymptomatic, and the retained sponge is discovered accidentally when the patient undergoes a radiologic study for some other reason.
Figure 10.64 Elderly man with a retained surgical sponge granuloma (gossypiboma) (arrow).
Vertebroplasty and kyphoplasty are procedures to treat compression fractures in the thoracic and lumbar spine. Recently, their usefulness has been called into question, but they are common procedures, and many patients appear to gain considerable pain relief from them. The injected cement (usually methymethacrylate) may on occasion extrude from the vertebral body. If it does not impinge upon the spinal cord or a nerve root, there is usually no patient harm. The material may also enter the vascular system, usually the spinal venous complex, and embolize to distant sites, such as the patient’s lungs (Figure 10.65) (Karlsson et al., 2005; Taljanovic et al., 2006a, 2006b).
Figure 10.65 Vertebroplasty cement has embolized to the patient’s lungs. This was an incidental finding on a routine chest radiographic series.
An interesting foreign body injury results from the deliberate or accidental injection of metallic mercury. Metallic mercury is easily recognized on radiographs. It is most commonly seen in patients who ingest it deliberately as part of a suicide attempt or who inadvertently ingest or aspirate it as a complication of long intestinal tube use. Metallic mercury at room temperature is fairly non-toxic; however, mercury compounds and metallic mercury that is warmed enough to produce significant mercury vapor are quite toxic. Nowadays, metallic mercury is rarely seen as it is no longer used for everyday applications in thermometers or barometers, and intestinal tubes no longer contain mercury-weighted bags to help with tube passage.
Deliberate injection of mercury subcutaneously or intravenously produces a dramatic radiographic appearance (Figure 10.66). Individuals may inject themselves in the mistaken belief that mercury increases their strength, or they may be drug abusers or even attempting suicide (Naidich et al., 1973; Peterson et al., 1980; Spizarny & Renzi, 1987; Wenzel et al., 1980).
Figure 10.66 21-year-old man who injected himself with metallic mercury. (A,B) Metallic mercury emboli are evident in the lungs, and (C,D) metallic emboli are evident in the antecubital fossa of the left elbow.
At one time, mercury was used as an anaerobic seal for arterial blood gas sampling during cardiac catheterization and as a seal for arterial blood gas sampling syringes and arterial pressure monitors. If the seal was broken, metallic mercury could be inadvertently injected into the arterial or venous system of the patient. Although mercury thermometers are uncommon nowadays, soft-tissue mercury deposits may be seen in patients who injure themselves by breaking a mercury thermometer.
If mercury is injected into subcutaneous tissues, it forms irregular globules and may remain in place for months to years. If it is injected into the venous system, it will embolize to the lungs where it forms small globules in the peripheral branches of the pulmonary arteries. The mercury may also pool in the right ventricle. Differentiating aspirated metallic mercury from mercury embolism to the lungs is difficult on the basis of chest radiographic appearances alone. The diagnosis depends on the patient history, presence of mercury in the right ventricle or subcutaneous tissue of the arm or leg (favoring mercury embolism) or the presence of mercury in the gastrointestinal tract (favoring mercury aspiration) (Peterson et al., 1980; Spizarny & Renzi, 1987; Wenzel et al., 1980). Surprisingly, metallic mercury in the bronchial tree or in the pulmonary arterial tree is usually not associated with symptoms, and it may remain undiscovered indefinitely.
Halloween is a fun time of year for children. Unfortunately, some individuals have taken delight in hiding needles, razor blades, and other harmful items in candy and food given to trick or treaters. Radiography of food and candy is surprisingly effective (Figure 10.67) and can be used to identify harmful objects or to reassure parents that there is a low likelihood for a sharp object lurking in treats.
Figure 10.67 Halloween candy. Trick or treat candy. There are no hidden needles or razor blades. The candy and the apple (round density) were eaten with much enjoyment.
Blast Injuries
Blast injuries encountered in terrorist attacks using improvised explosive devices (IEDs) are fortunately rare even in this age of global terrorism. Such injuries are most commonly encountered on the battlefield, but may be seen in an urban terrorist attack, such as the Boston Marathon bombing (Kellerman & Peleg, 2013; Singh et al., 2014, 2016). In principle, they are no different than more routine injuries. The forces involved in blast injuries, however, are usually of much greater magnitude than more common injuries from automobile accidents, gunshot wounds, and other daily trauma.
Blast forces may produce extensive soft-tissue and bony injury with frequent foreign bodies composed of metallic shrapnel as well as non-metallic debris (paper, cardboard, wood fragments, dirt, rocks, plastic) from the bomb itself or from nearby objects caught up in the blast. Blast injuries are described as a spectrum of primary, secondary, tertiary, and quaternary blast patterns (Champion et al., 2009; Garner & Brett, 2007; Horrocks, 2001; Proud, 2013; Singh et al., 2016). These include the barotrauma of the explosive detonation (primary blast injury), debris in the blast wind (secondary blast injury), physical displacement of the victim with blunt or penetrating trauma (tertiary blast injury), and burns, crush, and inhalational injuries (quaternary blast injury).
A more extensive discussion of blast injuries is beyond the scope of this chapter. It is safe to say that blast injuries, whether occurring on the battlefield, in a terrorist attack, or in an industrial accident, are likely to produce severe soft-tissue and bony abnormalities with a great potential for foreign bodies, both metallic and non-metallic. In nearly all cases, standard radiography and cross-sectional imaging, especially CT, play an important role in the evaluation of foreign bodies and skeletal trauma (Singh et al., 2016).
Foreign Bodies and MR Imaging
All patients should be properly screened before undergoing an MR imaging study. Patients should be asked about prior surgery, foreign body injuries, the presence of a medical device or implant, and the possibility of a pregnancy (Eshed et al., 2010; Hunter, 1996; Shellock, 2001; Shellock & Karacozoff, 2013). Metallic foreign bodies such as bullets or shrapnel may present a hazard to the patient, because they can be moved or twisted by the strong magnetic fields encountered in MR imaging studies. The seriousness of the risk depends on the ferromagnetic characteristics of the foreign body, its location, and the strength of the MR magnetic fields (Dula et al., 2014). See the following sites for more specific and timely information: MRI Safety Information; MRIMaster.com; RadiologyInfo.org.
Small intraocular ferromagnetic fragments are a contraindication to MR imaging. They have a significant risk of causing vitreous hemorrhage and possible blindness. However, if a patient with a possible foreign body in the eye, such as a metal worker constantly exposed to tiny metallic slivers, has no symptoms and radiographs of the orbits show no recognizable foreign bodies, then MR imaging is considered safe (Shellock, 2001). Some eyeliners applied with a tattooing process and some eye makeup may contain enough ferrous pigment to produce MR imaging artifacts. They may also interact with the magnetic fields enough to cause skin irritation and swelling.
In general, tattoos in other parts of the body cause no problems. Microscopic pieces of metal may be deposited into subcutaneous and muscular tissues after orthopedic surgery. These fragments are often invisible on radiographs, but they will produce visible MR imaging artifacts that are usually minor, although they can impair the diagnostic utility of a study (Figure 10.68).