10 Test Cases: Applying Lung CT Screening Reporting and Data System (Lung-RADS)
Summary
This final chapter will test your knowledge and application of the Lung CT Screening Reporting and Data System (Lung-RADS). You will be shown 10 unknown cases. For each unknown case, determine the appropriate Lung-RADS score and best course of management. The correct answer(s) will follow.
Keywords: Lung-RADS 1, Lung-RADS 2, Lung-RADS 3, Lung-RADS 4, solid nodule, ground-glass nodule, part-solid nodule, pericystic nodule
10.1 Case 1
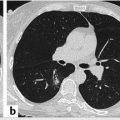
Axial low-dose computed tomography (LDCT) screen-selected mediastinal (▶ Fig. 10.1 a) and lung window (▶ Fig. 10.1 b) images of an asymptomatic current female smoker demonstrate a 12-mm solid, rounded, soft-tissue attenuation noncalcified endobronchial lesion that nearly occludes the lingular bronchus lumen. What is the correct Lung-RADS category and appropriate course of management?

10.2 Case 2
Coned-down axial LDCT screen (▶ Fig. 10.2) through the right lower lobe of a 65-year-old woman shows a 7-mm total diameter part-solid nodule composed primarily of ground-glass but with a 3-mm solid component on baseline screening LDCT. What is the correct Lung-RADS category and appropriate course of management?

10.3 Case 3
Coned-down axial LDCT screen (▶ Fig. 10.3) through the left lower lobe of a current smoking 55-year-old woman reveals a 6.2-mm average diameter solid, spiculated, noncalcified nodule in the superior segment (5.3 + 7.1 ÷ 2 = 6.2 mm) on baseline screening LDCT. The nodule is rounded off to the nearest whole number or 6 mm in diameter. Note the background of extensive centrilobular emphysema (score: 3/3). What is the correct Lung-RADS category and appropriate course of management?

10.4 Case 4
Coned-down axial LDCT screen (▶ Fig. 10.4) through the posterior segment of the right upper lobe of a 73-year-old woman, current cigarette smoker with a total 43-pack-year history of tobacco abuse, shows a pure ground-glass nodule (GGN) measuring 14 mm in maximum diameter. Although some margins appear slightly irregular, there is no solid component present and there is no architectural distortion. What is the correct Lung-RADS category and appropriate course of management?

10.5 Case 5
Baseline LDCT screen (▶ Fig. 10.5 a) of a 69-year-old former heavy smoker asymptomatic man demonstrates a 10-mm slightly lobulated nodule with an irregular border superiorly. A 3-month follow-up LDCT was recommended but not performed until 4 months later (▶ Fig. 10.5 b), which shows significant interval growth of the lesion to 18 mm with increased polylobulation and spiculated borders. Note the notch at the 7:00 plane. How would you categorize the Lung-RADS score on both the baseline (▶ Fig. 10.5 a) and follow-up study (▶ Fig. 10.5 b)? What is the appropriate course of management at this time? Calculate the percent growth of this lesion.

10.6 Case 6
Baseline LDCT screen (▶ Fig. 10.6 a) of a 69-year-old former heavy smoker asymptomatic woman shows a part-solid pericystic lesion in the peripheral anterior segment of the right upper lobe. The total diameter is 9 mm. Two subtle solid components to the lesion are identified at the 12 o’clock position (▶ Fig. 10.6 a). Follow-up LDCT 6 months later (▶ Fig. 10.6 b) shows near-complete solid replacement of the cystic component of the lesion. Even though the total diameter is still 9 mm, the solid component has significantly increased and the borders are more polylobulated. How would you categorize the Lung-RADS score on both the baseline (▶ Fig. 10.6 a) and follow-up study (▶ Fig. 10.6 b)? Do you agree with the initial recommendation to follow up the lesion in question in 6 months? What is the appropriate course of management at this time?

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree