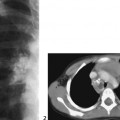
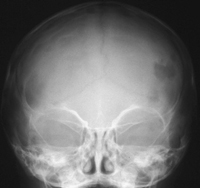
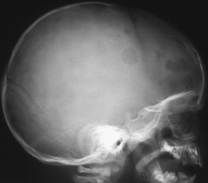
CASE 101 A 4-year-old girl presents with back pain. Figure 101A Figure 101B Frontal radiograph (Fig. 101A) demonstrates marked loss of T12 vertebral body height (vertebra plane) with preservation of adjacent disk spaces and posterior elements. Coronal enhanced MRI (Fig. 101B) depicts asymmetrically marked collapse of the vertebral body and a left paraspinal enhanced soft tissue mass. Langerhans’ cell histiocytosis (LCH) LCH is a spectrum of disease processes resulting from the abnormal clonal proliferation of the Langerhans’ cell histiocyte (and its precursors), and the resultant infiltration of these cells into normal tissues. Bone, skin, and lymph nodes are the most common sites for infiltration, with 80 to 95% of patients demonstrating bone lesions at some time during the course of illness. LCH was previously known as histiocytosis X and grouped into three forms based on clinical manifestations. What was previously labeled eosinophilic granuloma, Hand-Schüller-Christian disease, and Letterer-Siwe disease are now referred to as localized, chronic recurring, and acute/subacute disseminated LCH, respectively. The disease process occurs during the first 3 decades of life, with a peak between 5 to 10 years. Males are more often affected, and the disease is less prominent outside the Caucasian population. Overall, the disease is rare, representing <1 to 2% of biopsied bone lesions. The disseminated form is found primarily in infants, whereas isolated bone lesions are seen in the 5- to 10-year-old age group. The cause of LCH is unknown. Spontaneous resolution in some cases and a response to steroids in others has suggested a possible infectious (viral) etiology. Immunologic alterations in various patients support the concept of a disorder of immune regulation. The disease is usually sporadic; however, an autosomal recessive inheritance has been proposed by some researchers. The clinical presentation will be dependent on the site, tissue, and extent of infiltration. The localized form of LCH is the mildest form usually presenting with pain and tenderness at the involved bone site. These patients are between 5 and 15 years of age and make up ~75% of cases of LCH. Skull, mandible, ribs, and pelvis account for >50% of involved sites. Approximately one third of lesions involve the long bones, usually the femur. The chronic-recurring form of LCH makes up ~20% of the patient population, with otitis media being the most common presentation. Bone pain, dermatitis, and growth retardation are further symptoms. The classic triad of diabetes insipidus, exophthalmos, and destructive skeletal lesions (90% in skull) is seen in 10 to 15% of patients with this form of LCH. The acute disseminated or fulminant form of LCH presents in infants and children generally <2 years of age. Hepatosplenomegaly, lymphadenopathy, anemia, diffuse bone marrow infiltration, and hemorrhage are the typical clinical findings. Figure 101C Frontal skull radiograph depicts multiple, mostly ill-marginated lytic lesions. Figure 101D
Clinical Presentation


Radiologic Findings
Diagnosis
Differential Diagnosis
Discussion
Background
Etiology
Clinical Findings
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree