12 Joint Disease
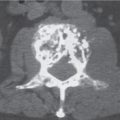
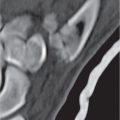
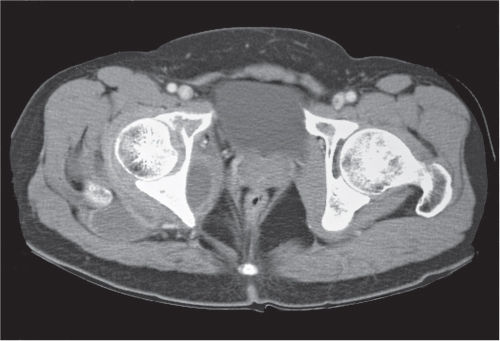
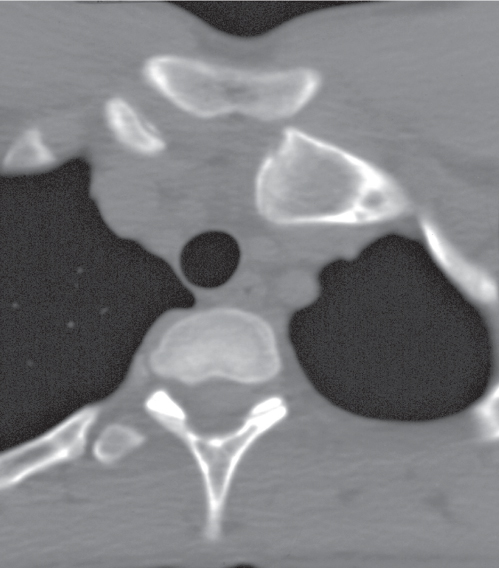
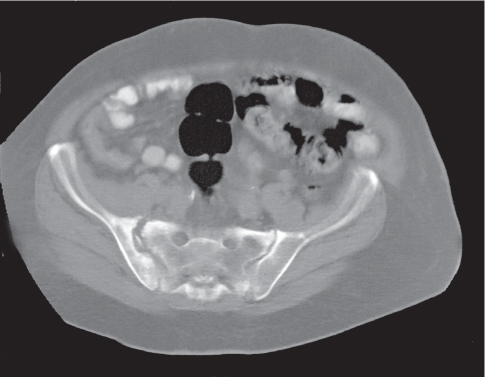
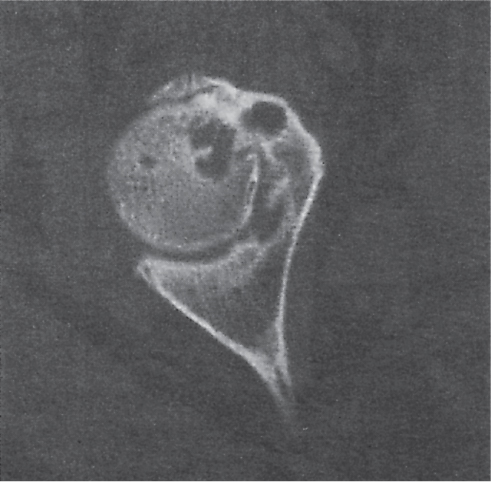
The diagnosis of articular disorders is primarily made by conventional radiography. Computed tomography (CT) is useful to assess the extent of both bone and soft tissue involvement. Para-articular soft tissue masses such as synovial cysts and abscesses are readily depicted by CT (Fig. 12.1). In skeletal trauma with joint involvement, CT can be very valuable to accurately define fractures and dislocations and to delineate intra-articular osteochondral fragments that may escape detection by plain film radiography. This is particularly true for the evaluation of joints that either have a complex anatomy or are difficult, if not impossible, to visualize in two perpendicular planes by conventional radiography. An example of the latter is the diagnosis of a sternoclavicular joint dislocation that is difficult to ascertain by conventional imaging technique but is easily documented by CT, as the dislocated clavicle is usually located anteriorly or occasionally posteriorly to the adjacent sternum (Fig. 12.2).
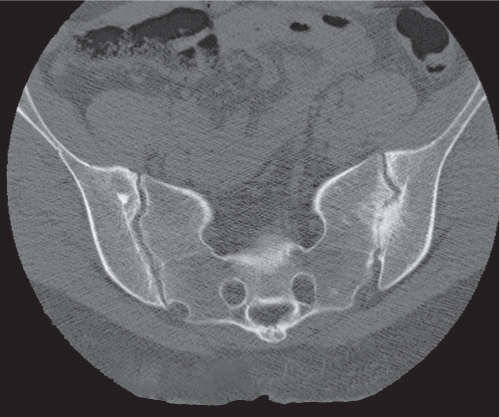
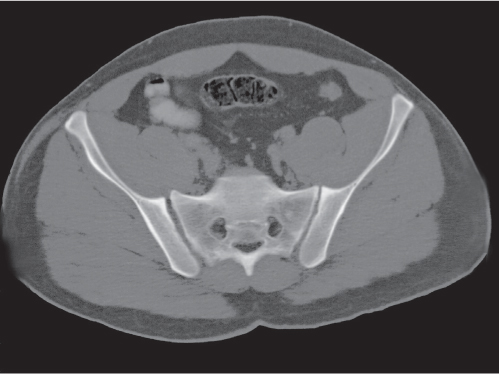
Each sacroiliac joint consists of two articulations: the posterosuperior two thirds of the joint are syndesmotic, and the anteroinferior one third is synovial. Sacroiliac joints are difficult to analyze on plain films, and their interpretation is greatly facilitated by CT. The normal synovial sacroiliac joint measures 2 to 4 mm in width; the ligamentous portion of the joint is more variable and wider. Normal sacroiliac joints are symmetric and without erosions, sclerosis, and fusions. Widening of the sacroiliac joints is commonly found in traumatic diastasis (Fig. 12.3), where it can be unilateral or bilateral, and in primary or secondary hyperparathyroidism (Fig. 12.4). Unilateral widening of a sacroiliac joint associated with erosions, destruction, and sclerosis suggests an infectious process (Fig. 12.5). Occasionally, widening of the sacroiliac joints is also observed in the early (erosive) stage in a variety of inflammatory diseases, such as ankylosing spondylitis, enteropathic spondyloarthropathy, Reiter syndrome, psoriasis, and rheumatoid arthritis. These conditions, however, tend to progress to a more characteristic joint space narrowing and eventual fusion. Associated erosions and particularly sclerosis are always more pronounced on the iliac side of the joint.
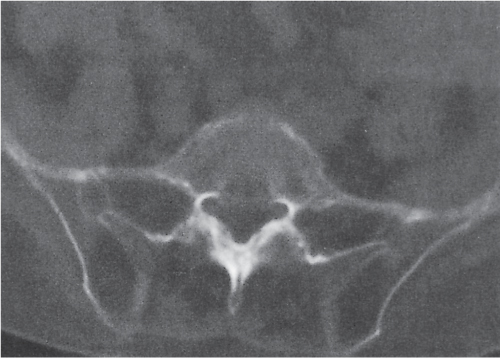
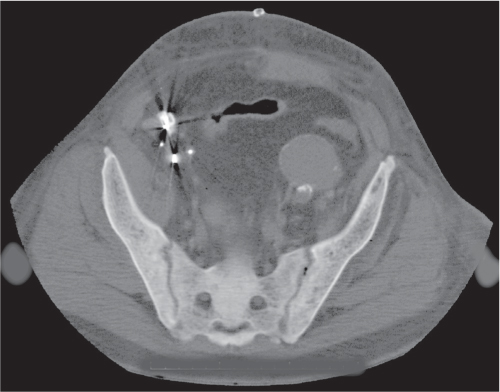
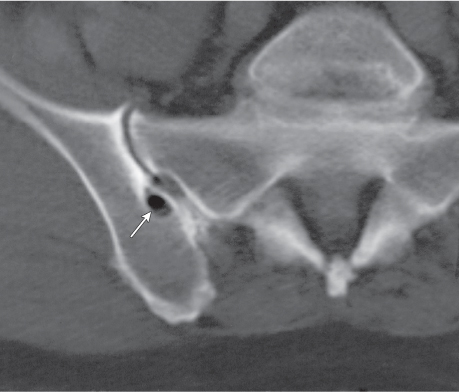
Sacroiliitis can be differentiated by both distribution and morphology of the articular changes. A bilateral and symmetrical involvement of the sacroiliac joints with poorly defined erosions and adjacent sclerosis, joint space narrowing, intra-articular osseous fusion, and ligamentous ossification is characteristic for ankylosing spondylitis (Fig. 12.6) and enteropathic spondyloarthropathy. In psoriasis and Reiter syndrome, the sacroiliac joint involvement is usually bilateral but characteristically asymmetric and associated with extensive sclerosis, particularly on the ilium, and occasional fusion. Both conditions must be differentiated from osteitis condensans ilii (Fig. 12.7), where a symmetric triangular sclerosis of the inferior aspect of the ilium is not associated with any sacroiliac joint abnormality. In rheumatoid arthritis, sacroiliac joint manifestations occur only late in the disease and include bilateral superficial erosions with minimal sclerosis but usually without bony ankylosis. In primary and secondary hyperparathyroidism (renal osteodystrophy), subchondral bone resorption results in symmetric widening of the sacroiliac joints with adjacent sclerosis (Fig. 12.8). Unilateral sacroiliac joint involvement suggests infectious or posttraumatic joint disease. Pyogenic sacroiliitis occurs commonly in intravenous drug abusers, and CT may demonstrate an associated soft tissue abscess besides erosive and sclerotic changes in the involved sacroiliac joint (Fig. 12.9). Degenerative sacroiliac joint disease is relatively frequently seen in patients older than 40 y. Narrowing of the joint space, sclerosis with usually smooth subchondral bone margins, and anterior osteophytes progressing occasionally to complete bony bridging of the sacroiliac joint can be encountered. Rarely, small subchondral cysts that may simulate erosions are also present. Occasionally, these cysts contain air (pneumatocysts) (Fig. 12.10). Many other arthritic processes such as gout and calcium pyrophosphate deposition disease (CPDD) may rarely affect the sacroiliac joints also, but they have no characteristic features. Sacroiliitis circumscripta (Fig. 12.11) is a nonspecific localized inflammatory process of unknown etiology presenting initially with superficial erosions with subsequent sclerosis and eventually a bridging osteophyte anteriorly.
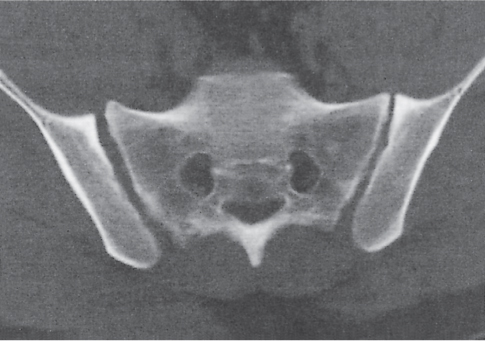
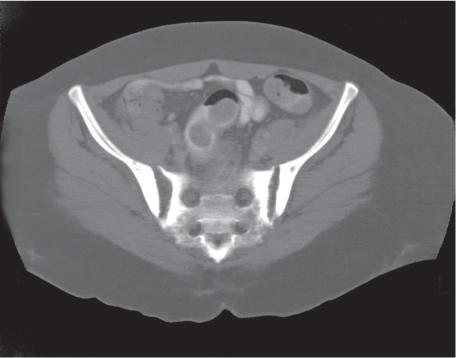
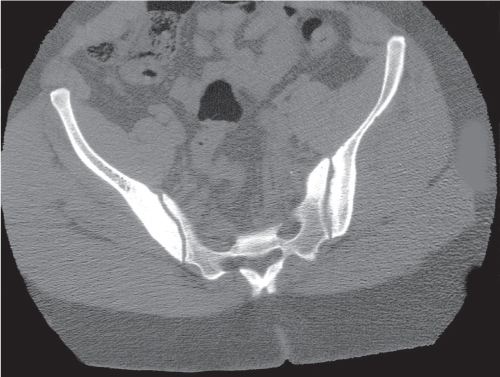
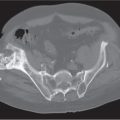
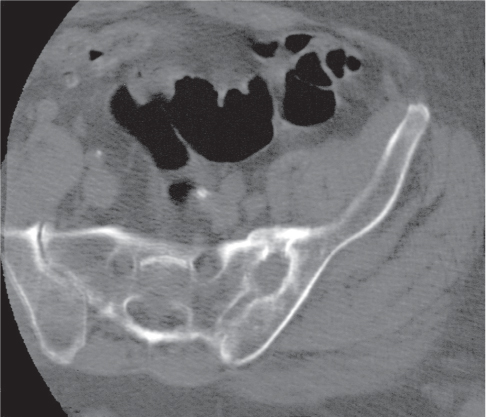
Pelvic trauma may involve the sacroiliac joint and can be difficult to detect with conventional radiographs. Diastasis of one or both sacroiliac joints (Fig. 12.12) may be associated with separation of the pubic symphysis (“pelvic dislocation”). Uni-lateral sacroiliac joint dislocation associated with a fracture of the ipsilateral superior and inferior pubic rami is termed a is a bucket handle–type injury. The pelvic ring is formed by the pelvis and sacrum. All conditions with at least two complete interruptions of the pelvic ring such as fractures or dislocations are unstable and require open or closed stabilization to prevent complete pelvic collapse.
The hip is a ball-and-socket joint consisting of the femoral head and the acetabulum. The latter is composed of the acetabular roof, the anterior and posterior wall, the quadrilateral lamina, and the anterior and posterior labrum. In contrast to conventional radiography, these parts can readily be discerned by CT with the exception of the fibrocartilaginous labrum and therefore assessed individually for disease involvement (Fig. 12.13).
Fractures involving various components of the acetabulum and femoral head can be diagnosed with high accuracy with proper anteroposterior, lateral, and oblique (Judet) views of the hip. However, in a multitrauma patient, adequate conventional radiographs cannot always be obtained. In these conditions, CT is useful in the detection of acetabular and femoral head fractures.
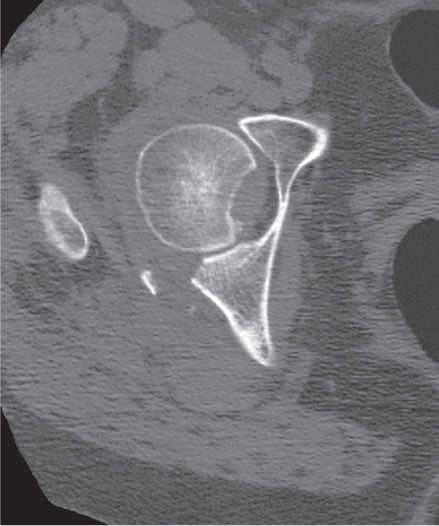
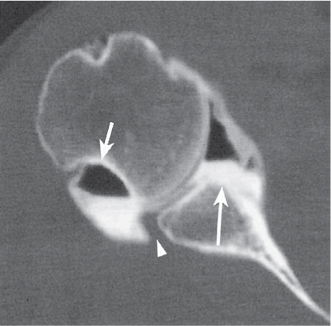
Compared to conventional radiography, the greatest contribution of CT consists of the accurate depiction of the fracture-dislocation pattern in the hip that dictates whether a particular injury will subject to open or closed reduction and treatment. This decision is largely dependent on the number and size of intra-articular bone fragments, fracture fragment displacement, and congruity between femoral head and acetabulum (Fig. 12.14). Usually these questions cannot be satisfactorily answered by conventional radiography.
Osteochondral fractures of the femoral head (capital fractures) are frequently associated with posterior hip dislocations caused by a pull of the ligamentum capitis femoris connecting the fovea of the femoral head with the transverse ligament at the bottom of the acetabulum (Fig. 12.15). These avulsion fractures are often difficult to diagnose by conventional technique and may eventually result in a clinical and radiographic picture that is impossible to differentiate from avascular necrosis of the femoral head.
Avascular necrosis (AVN) of the femoral head is caused by obstruction or disruption of its blood supply. The most common causes include sequelae of a femoral neck fracture, steroid therapy, sickle cell disease, and collagen vascular diseases (especially lupus erythematosus and rheumatoid arthritis). Less common causes of AVN include human immunodeficiency virus (HIV) infection, alcoholism, pancreatitis, a variety of vascular diseases, including arteriosclerosis, caisson disease (dysbaric osteonecrosis), Gaucher disease, amyloidosis, radiation therapy, and pregnancy. An idiopathic form of AVN of the hip can occur at any age, but it is most common in children between 4 and 7 y of age, where it is termed Legg–Calvé–Perthes disease (Fig. 12.16).
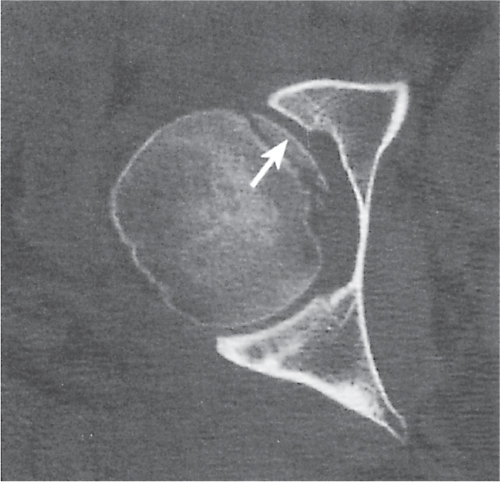
CT is less sensitive in diagnosing AVN of the hip than either nuclear medicine or magnetic resonance imaging (MRI). Compared with conventional radiography, CT upgrades the stage of AVN in approximately one third of cases, which may have consequences for the selection of the optimum therapy. In the normal hip, an asterisk-like condensation of bone in the center of the femoral head is seen on transaxial CT images at the level of the fovea caused by the crossing of compressive and tensile trabeculae (asterisk or star sign, Fig. 12.17). In early AVN, the well-defined and centrally located asterisk appears smudged by focal sclerosis and bone resorption, or, in slightly more advanced cases, the radiodense zone reaches the articular surface of the femoral head (Fig. 12.18). The following stages of AVN of the hip can be recognized: (1) minimal focal sclerosis and osteopenia; (2) distinct sclerosis and focal lucencies or cyst formation; (3) subchondral lucency (crescent sign) but without flattening (collapse) of the femoral head; (4) subchondral fracture and/or flattening of the femoral head; and (5) marked collapse of the femoral head with secondary arthritic changes, including joint space narrowing and acetabular involvement.
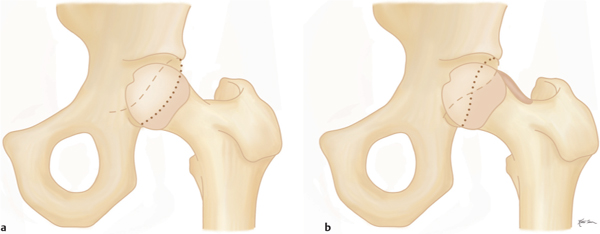
Femoroacetabular impingement (FAI) is caused by abnormal abutment between the proximal femur and adjacent acetabular rim in flexion and internal rotation, resulting in damaging of the acetabular labrum and cartilage with subsequent osteoarthritis. A cam-type impingement caused by a bony prominence or bump of the anterolateral femur head–neck junction is differentiated from a pincer-type impingement caused by overcoverage of the femoral head by the acetabulum. Acetabular overcoverage results from acetabular retroversion (posteriorly rotated acetabulum), coxa profunda (deep acetabular socket extending on conventional radiographs medial to the ilioischial line), or protrusio acetabuli (acetabular protrusion into the pelvis). FAI is most commonly caused by a combination of both types (mixed cam–pincer type) (Figs. 12.19, 12.20).
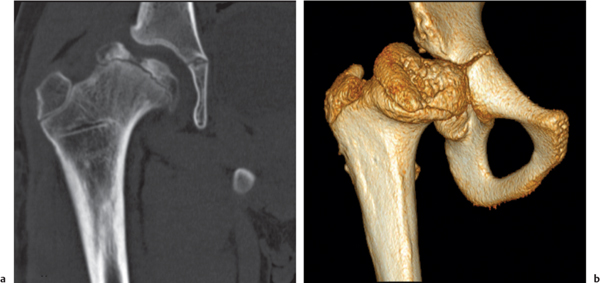
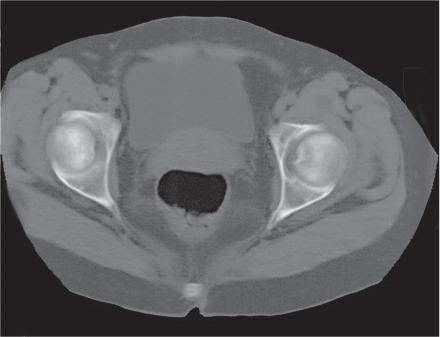
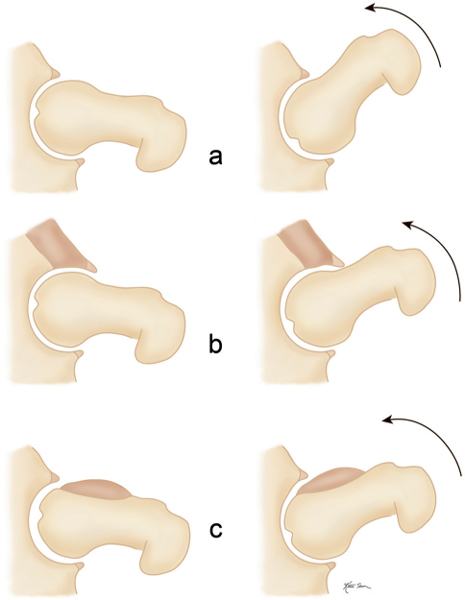
CT findings of the cam-type FAI may also include, besides the bony bump at the anterolateral femur head–neck junction (sometimes referred to as a “pistol grip” deformity), a femoral osteophyte posterolateral to the osseous bump (bump–osteophyte complex), herniation pit (synovial or fibrocartilaginous defect with thin sclerotic border anterolateral in the proximal femur neck), and thickened iliofemoral ligament. Acetabular findings in the pincer-type impingement may include, besides retroversion, coxa profunda, or protrusio acetabuli, acetabular rim osteophytes, an os acetabuli, subchondral sclerosis, and labral (paralabral) cysts. FAI typically presents in young, physically active patients and if untreated may progress to premature full-blown osteoarthritis with its characteristic imaging findings.
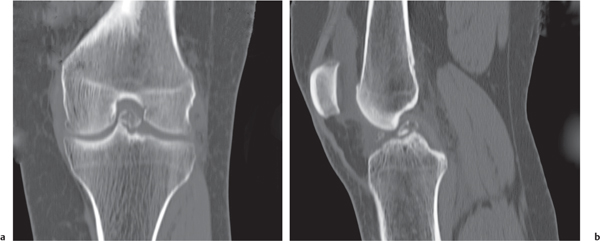
Plain-film radiography and MRI are the main imaging methods for evaluation of the knee. MRI is far superior to CT in the assessment of ligamentous, meniscal, and articular cartilage pathology. CT might be useful in identifying intra-articular loose bodies in such conditions as osteochondritis dissecans, osteochondromatosis, and a variety of arthritic joint diseases (e.g., degenerative, neuropathic, posttraumatic, infectious, CPDD, hydroxyapatite crystal deposition disease [HADD], and ochronosis) (Fig. 12.21).
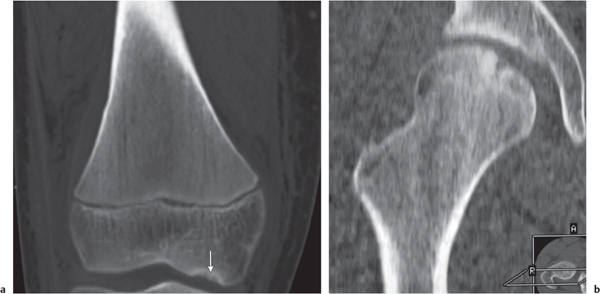
Spontaneous osteonecrosis of the knee (SONK, Ahlbäck disease) (Fig. 12.22) typically affects elderly, predominantly female patients with acute medial joint pain. It characteristically involves the weight-bearing surface of the medial femoral condyle, a lthough the lateral femoral condyle and the tibia plateau may occasionally be affected. More recently, an insufficiency fracture in an osteoporotic patient has also been implicated as etiology besides the vascular pathogenesis. Mild flattening of the weight-bearing aspect of the femoral condyle associated with an area of radiolucency with sclerosis proximal to it precedes the full-blown picture of a radiolucent focus surrounded by a sclerotic halo associated with a collapsed subchondral bone. In contrast, osteochondritis dissecans (Fig. 12.23) most commonly affects the non–weight-bearing portion of the medial femoral condyle in the intercondylic notch area and occurs primarily in young male patients.

CT, including reformatted coronal and sagittal scans, can be useful in the accurate delineation of fractures of both the femur condyles and tibial plateau (Fig. 12.24). The degree of subchondral depression and fracture fragment displacement are crucial factors in the selection of the treatment modality (e.g., conservative vs surgical intervention).
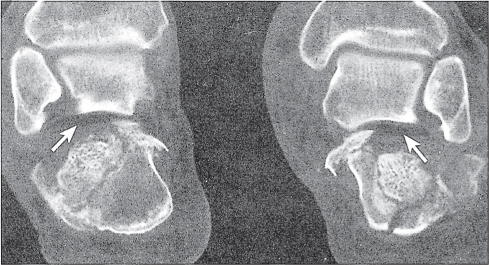
Fractures of the ankle and foot are reliably diagnosed with conventional radiography. CT may be useful in these cases to assess fragment displacement and joint involvement and to identify the number and position of loose bodies (Fig. 12.25). CT may also depict subtle fractures and subluxations, especially in the tarsal bones, that may escape detection with conventional technique. For both therapeutic and prognostic reasons, an accurate fracture assessment is particularly important in the tibial plafond, the dome of the talus, the subtalar joints, and the tarsometatarsal joints (Lisfranc joint). Accompanying soft tissue injuries, including trapped soft tissue structures and lacerated ligaments and tendons, may also be diagnosed, but their CT evaluation is inferior to MRI. Nevertheless, the bony structures in the ankle and foot are well suited for CT evaluation, as images in different planes can be obtained by reformation of the axial images.
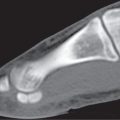
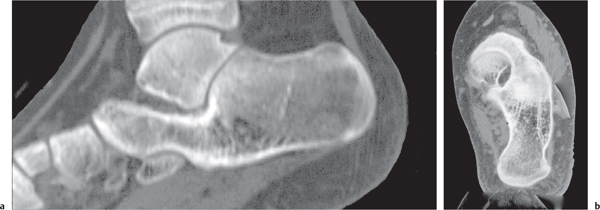
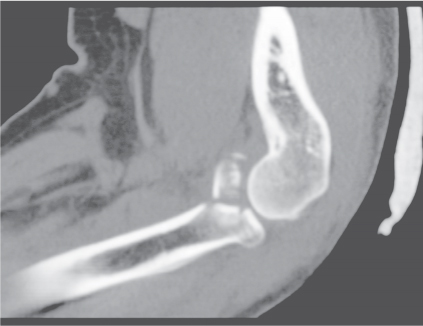
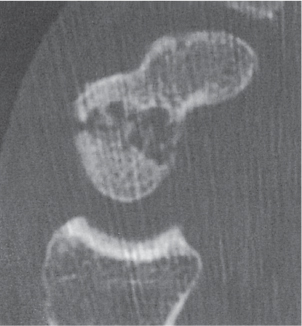
CT is effective in diagnosing tarsal coalitions that may be complete or incomplete and composed of fibrous (40%), cartilaginous (10%), or osseous (50%) tissue. Coalitions commonly occur between the calcaneus and navicular and between the talus and calcaneus, less frequently between the talus and navicular, and rarely between the calcaneus and cuboid (Figs. 12.26 , 12.27). Occasionally, more than two tarsal bones are affected. Fusion between the talus and calcaneus most frequently occurs at the level of the sustentaculum tali (Fig. 12.28) and may be difficult to demonstrate by plain film radiography. Coalition of the posterior subtalar facet joint is not uncommon either. Reformatted coronal images are most useful for the unequivocal demonstration of this coalition. In case of a fibrous or cartilaginous union, secondary changes such as close apposition of the involved joints, sclerosis of the articular margins, and cortical irregularities may be evident. Hypoplasia of the talar head and/or a talar beak arising characteristically at the talonavicular joint may also be associated with tarsal coalitions. This talar beak has to be differentiated from the more common degenerative talar spur that originates at the insertion of the talonavicular joint capsule and is therefore not directly contiguous with the distal articular surface of the talus.


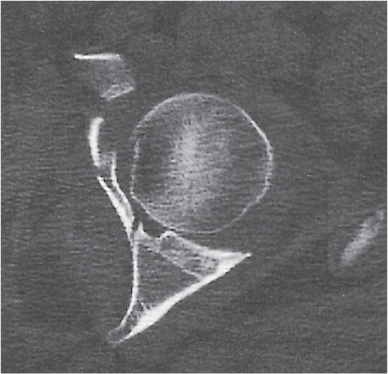
CT is useful for displaying various shoulder fractures, including Hill–Sachs compression fractures, involving the posterolateral humeral head, and osseous Bankart lesions, involving the anteroinferior glenoid rim, both of which are commonly associated with anterior glenohumeral dislocations (Fig. 12.29). The glenoid labrum is best evaluated with CT double-contrast arthrography. The normal glenoid labrum is a fibrocartilaginous structure with smooth margins. It is triangular-shaped anteriorly and more rounded and thicker posteriorly. With shoulder instability pattern and recurrent dislocations, the labrum may be blunted, frayed, embedded with iodinated contrast material, and partially or completely torn. CT arthrotomography demonstrates associated capsular and rotator cufftears, loose bodies, joint cartilage abnormalities, synovial hypertrophy, and anomalies of the intra-articular portion of the long biceps tendon, which may be either displaced from its normal location in the bicipital groove or completely absent, indicating a complete tear.
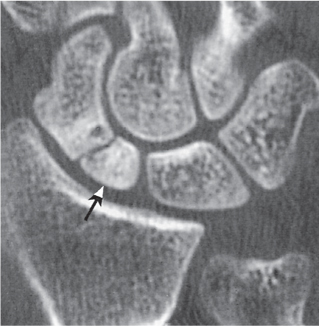
In the complex articulations of the elbow and wrist, CT may be useful for the identification of subtle fractures and subluxations that are not recognized by conventional methods (Fig. 12.30). Fracture complications such as nonunion and avascular necrosis (e.g., in the scaphoid) are also effectively evaluated by CT (Figs. 12.31 , 12.32).
The temporomandibular joint is divided by a disk that may dislocate, usually in an anterior direction. CT is comparable to arthrography in diagnosing this condition, as the disk can be accurately localized because of its relatively high CT density in excess of 60 HU. However, MRI is the imaging procedure of choice in this condition, as it demonstrates disk displacement as well as other joint pathology far better than CT.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree