13 Sella Turcica/Pineal Gland
13.1 Introduction
Both the pituitary gland and pineal gland are small structures that can have a variety of rare normal and abnormal conditions that can be difficult to interpret and diagnostically confusing. Understanding the normal anatomy and embryologic origins of these structures can aid in characterizing the pathologic conditions and physiologic variants they are likely to manifest.
13.2 Anatomy of the Pituitary Gland and Sella Turcica
The pituitary gland is an endocrine organ of dual origin; in fact, it may be easier to consider it as being two separate but adjacent organs. The anterior pituitary (adenohypophysis) is composed of glandular tissue, whereas the posterior pituitary is of neural origin (neurohypophysis). The pituitary sits within the sella turcica, within the central portion of the sphenoid bone (basisphenoid). The pituitary gland is bounded laterally by the cavernous sinuses (Fig. 13.1), and is connected by a stalk (the pituitary stalk, also known as the pituitary infundibulum) to the hypothalamus.
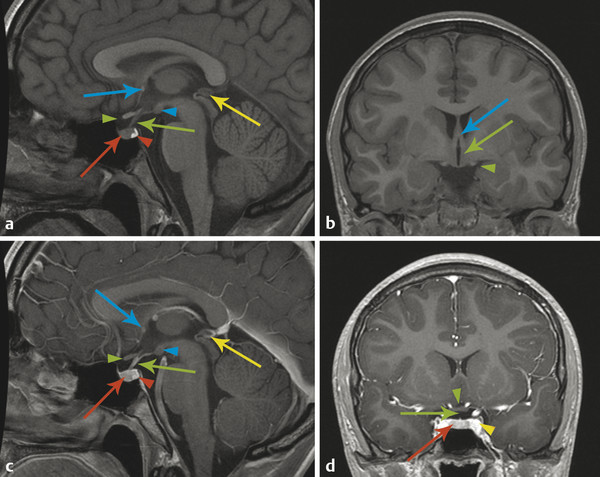
The adenohypophysis arises from an evagination of nasopharyngeal mucosa, known as Rathke’s pouch, through the basisphenoid bone within the craniopharyngeal canal. Rarely, there is a persistent craniopharyngeal canal; however, it is common to see the remnants of the obliterated craniopharyngeal canal (Fig. 13.2). The adenohypophysis joins with the neurohypophysis, a caudal extension from the median eminence of the hypothalamus. The adenohypophsyis manufactures and secretes hormones under control by the hypothalamus. The hypothalamus secretes releasing hormones (s. Tab.) that traverse the hypothalamic–hypophyseal portal venous system within the pituitary stalk. Because of this vascularity, the adenohypophysis shows a rapid and homogeneous enhancement pattern.

Hormone | Stimulant | Target |
Thyroid-stimulating hormone | Thyrotropin-releasing hormone | Thyroid gland |
Growth hormone | Growth-hormone–releasing hormone | Viscera (growth) |
Follicle-stimulating hormone | Gonadotropin-releasing hormone | Germ-cell maturation |
Luteinizing hormone | Gonadotropin-releasing hormone | Triggers ovulation |
Adrenocorticotropic hormone | Corticotropin-releasing hormone | Adrenal gland |
Prolactin* | Milk production | |
*Prolactin is normally secreted without stimulation; its secretion is inhibited by dopamine. | ||
13.3 Pituitary Lesions
Hypoenhancement within the pituitary gland raises the possibility of a neoplasm, typically a “microadenoma,” although an intraglandular cyst will also appear as a hypoenhancing focus. The two types of intraglandular cyst are an inclusion cyst between the adenohypophysis and neurohypophysis, known as a pars intermedia cyst (Fig. 13.3), and a Rathke’s cleft cyst (Fig. 13.4). Both types of cyst are incidental. A pars intermedia cyst is typically not a diagnostic challenge and requires no follow-up or intervention. A Rathke’s cleft cyst can sometimes be difficult to differentiate from a cystic neoplasm, and occasionally can be enlarged and exert mass effect that may require surgical intervention.


In one variant appearance of the pituitary gland, it is flattened to the floor of the sella turcica (Fig. 13.5). In the early days of computed tomography (CT) and magnetic resonance imaging (MRI), this was called an empty sella; however, with high-resolution imaging, it is known that the gland is present but flattened, making the term “partially empty sella” more appropriate for the appearance of this condition. This is typically a normal variant of pituitary shape, but is commonly seen in the clinical setting of pseudotumor cerebri, which should therefore be considered a possibility when a partially empty sella is found in an evaluation for headache or palsy associated with cranial nerve VI.

Primary pituitary tumors are much less common in children than in adults. As in adults, they nearly always arise from the adenohypophysis. Pituitary tumors are referred to as microadenomas (if smaller than 10 mm) and macroadenomas (if larger than 10 mm), but this distinction in size may be less important than determining why a given lesion is symptomatic. A microadenoma will not cause mass effect, and will therefore present only with endocrine abnormalities, such as elevated prolactin levels. Because microadenomas are typically secreting adenomas, their surgical resection optimally requires removal of the entire lesion.
Macroadenomas tend to present present with mass effect, most commonly on the optic chiasm, which can cause a bitemporal hemianopsia. An adenoma that reaches the size at which it exerts such an effect will typically be a nonsecreting adenoma, and the goals of its surgical management will primarily be to relieve its mass effect while preserving the function of adjacent structures. A subtotal resection of a nonsecreting macroadenoma may allow it to recur and require repeat surgery at a later date, but would appropriately address the patient’s symptoms. In the case of some secreting macroadenomas, however, such as those that secrete growth hormone, a gross-total resection is preferred. Other tumors in the sellar region, particularly craniopharyngiomas, are addressed in Chapter 8.
An enlarged pituitary gland raises the possibility of a pituitary tumor, and in this situation, thin-section pre- and postcontrast imaging of the pituitary gland is warranted. However, this requires determination of what constitutes an enlarged gland. As a rough estimate, a glandular height of up to 6 to 8 mm can be considered normal, but focal irregularity or asymmetry should raise concern even with a smaller gland size. Because of the hormonal changes associated with menarche, a slight physiologic hypertrophy of the pituitary, of up to approximately 9 or 10 mm, can be seen in females during early adolescence (Fig. 13.6). An additional situation in which there is physiologic pituitary glandular hypertrophy is in the newborn child, in whom the pituitary has a convex superior margin related to maternal hormonal stimulation (Fig. 13.7); this typically reverses over the first two weeks of life, and the finding of a suspected pituitary mass in a newborn should therefore be regarded with extreme caution.


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree