15 Trauma and Fractures: Shoulder Girdle and Upper Extremity
Scapula fractures are classified according to their anatomical location. Fractures of the body and spine, acromion, coracoid, extra-articular glenoid, and intra-articular glenoid are differentiated. Acromial fractures are classified as minimally displaced (type 1), displaced but without encroachment of the subacromial space (type 2), and displaced with encroachment of the subacromial space (type 3). An os acromiale (Fig. 15.13) should not be confused with a distal nondisplaced acromion fracture. Coracoid fractures proximal (type 1) and distal (type 2) to the coracoclavicular ligament are differentiated. Extra-articular glenoid neck fractures may involve either the anatomical neck (distal glenoid) or the surgical neck (proximal glenoid) and are divided in fractures without (type 1) or with (type 2) associated clavicle fracture or acromioclavicular (AC) separation. Accurate classification of the intra-articular glenoid fractures is most important for the selection of the appropriate treatment modality (Fig. 15.14).
Clavicle fractures are classified into three types according to the anatomical segment involved. Fractures of the proximal (medial) third (5%), middle third (80%), and distal (lateral) third (15%) are distinguished. The proximal fracture fragment is commonly elevated, whereas the distal fragment may be medially and caudally displaced. Fractures of the distal clavicle have been classified by Neer into three types. Type 1 consists of a nonarticular fracture without significant displacement, indicating intact coracoclavicular ligaments. Type 2 is a displaced nonarticular fracture with detached conoid component of the coracoclavicular ligament from the medial segment and intact trapezoid component of this ligament attached to the distal (lateral) segment. Type 3 fracture extends into the AC joint.
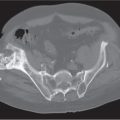
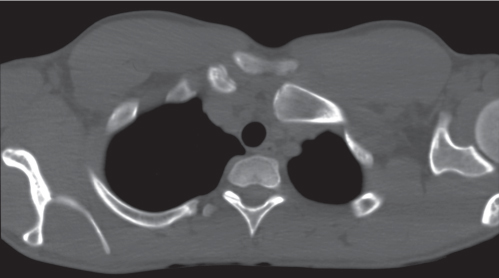
Sternoclavicular joint dislocations (Fig. 15.15) essentially occur in an anteroposterior direction and thus are virtually impossible to assess with conventional radiography unless some subluxation in the craniocaudal plane is associated, resulting in asymmetry of the medial clavicle ends on chest radio-graphs. CT is the imaging modality of choice in the evaluation of the sternoclavicular joint. Anterior (presternal) subluxation and dislocation are most common, with the medial end of the clavicle displaced anteriorly or anterosuperiorly. Except for a “cosmetic bump,” they are not associated with serious complications. Posterior (retrosternal) dislocations and subluxations are uncommon. The medial end of the clavicle is displaced posteriorly or posteromedially, and injuries to the adjacent neurovascular structures and airways are frequently associated. Sternoclavicular trauma may be accompanied with fractures of the clavicle and dislocations of the AC joint.
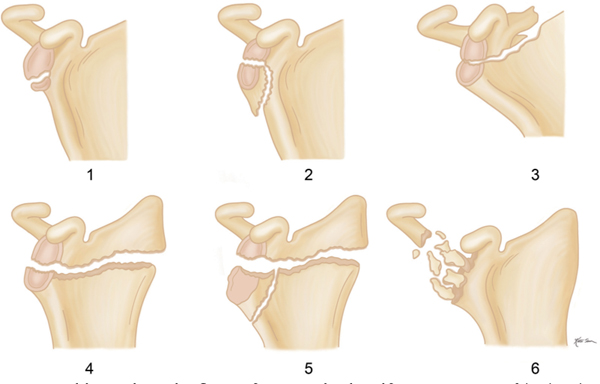
AC joint injuries are assessed radiographically by the width and displacement in this joint and the coracoclavicular distance. The width of a normal AC joint ranges from 0.3 to 0.8 cm, and the normal coracoclavicular distance measures 1.0 to 1.2 cm. These measurements, however, are not completely reliable because of an enormous variation in the normal population. Therefore, in borderline cases, comparison with the normal contralateral side should be obtained. Six types of AC joint injuries can be differentiated. In type 1 injury, the AC joint is normal or minimally widened. Para-articular soft tissue swelling may be the only abnormality. In type 2 separation, the distal end of the clavicle is slightly elevated (subluxed), the width of the AC joint widened between 1 and 1.5 cm, and the coracoclavicular distance typically varying between 1.3 and 1.5 cm. Type 3 injury represents a complete dislocation (separation) of the AC joint, with the lateral end of the clavicle projecting completely above the superior border of the acromion. The coracoclavicular distance measures 1.6 cm or more; otherwise, a fracture of the coracoid process is also suspected. Type 4 injury appears similar to a type 3 separation, but posterior displacement of the distal clavicle is also present. Type 5 injury appears like a severe type 3 separation, but instead of the clavicle being displaced superiorly, the finding is caused by marked inferior displacement of the scapula. Type 6 injuries represent an inferior dislocation of the distal clavicle with either a decreased coracoclavicular distance (subacromial type) or a reversed coracoclavicular distance (subcoracoid type).
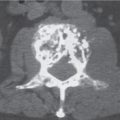
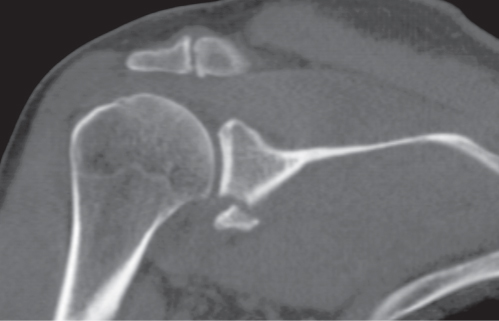
In glenohumeral joint dislocations, anterior, posterior, superior, and inferior dislocations are differentiated. Anterior dislocations may be associated with a compression fracture on the posterolateral aspect of the humeral head (Hill–Sachs lesion) and less frequently with a fracture of the anteroinferior rim of the glenoid (Bankart lesion), which may be limited to the cartilaginous labrum and not involve the osseous structures (Fig. 15.16). Posterior dislocations (Fig. 15.17) are much less common and often not recognized on conventional radiographs. A compression fracture on the humeral head (“reverse Hill–Sachs lesion”) may be evident. Both anterosuperior (subcoracoid) and inferior (luxatio erecta) dislocations are very rare. An inferior subluxation (drooping shoulder) is associated with hemarthrosis in proximal intra-articular humerus fractures, but it is also seen with neuro-muscular disease involving the rotator cuffand hemiparesis.
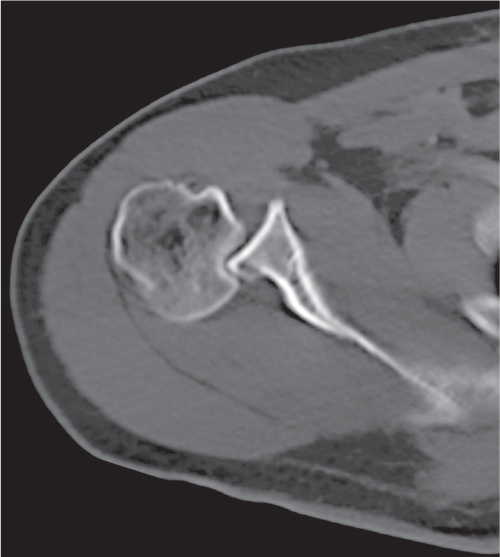
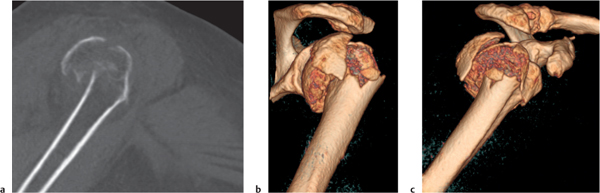
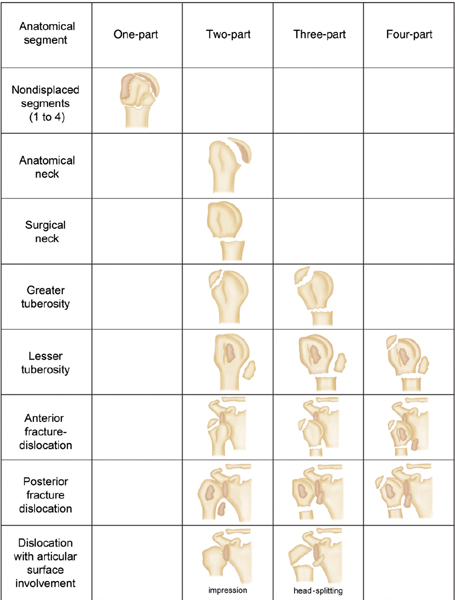
Fractures of the proximal humerus (Fig. 15.18) occur between one or all four major segments, which include the articular segment (anatomical neck fracture), the proximal humerus shaft (surgical neck fracture), the greater tuberosity, and the lesser tuberosity. The modified Neer four-segment classification (Fig. 15.19) is based on the number of displaced segments. Any fracture that is not displaced or only minimally displaced (< 1 cm) and is not angulated or only minimally angulated (< 45°) is disregarded. A one-part fracture may involve any or all four anatomical segments, but there is no displacement or angulation between fracture fragments. A two-part fracture indicates that only one segment is displaced in relation to the three that remain undisplaced or are intact. A two-part surgical neck fracture is also diagnosed in the absence of any angulation or horizontal displacement when the fracture is either impacted or comminuted. A three-part fracture commonly consists of a displaced greater or lesser tuberosity fracture combined with a surgical neck fracture. A four-part fracture typically involves both greater and lesser tuber-osities in addition to the surgical neck with displacement of all four segments. Two-, three-, and four-part fractures may be associated with either anterior or posterior glenohumeral joint dislocation.
If a single tuberosity fracture is present in an anterior shoulder dislocation, it invariably involves the greater tuberosity, whereas in a posterior dislocation, it involves the lesser tuberosity. Fractures of the surgical neck and the second tuberosity, however, may also be associated in these conditions. Furthermore, the fracture may involve the articular surface, resulting in “head-splitting” and “impression” fractures caused by severe impaction of the humeral head into the glenoid. Head-splitting fractures caused by central impact are not always associated with dislocations. In impression fractures, the defect in the humeral head is anterior and represents a severe reverse Hill–Sachs lesion extending into the articular surface of the humeral head, resulting from a traumatic posterior dislocation. In both conditions, loose intra-articular fracture fragments are a frequent finding.
Humerus shaft fractures are best classified into three types: noncomminuted; comminuted, but with contact between the main proximal and distal fragments; and comminuted, but without contact between the main fragments. In addition, the fracture pattern (e.g., transverse, oblique, or spiral) should be indicated.
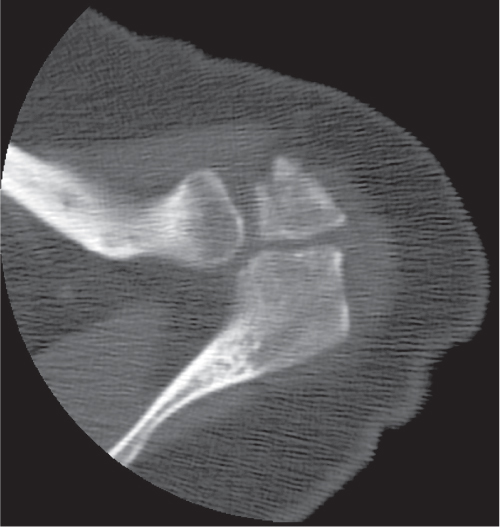
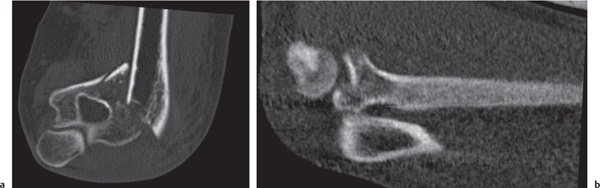
Fractures of the elbow (Fig. 15.20) may involve the distal humerus, proximal radius, and proximal ulna. Extra-articular fractures of the distal humerus may involve the epicondyles or supracondylar area. Intra-articular fractures of the distal humerus may involve either the trochlea or the capitellum alone (transcondylar or unicondylar fractures) or both (bicondylar or intercondylar fractures with or without supracondylar comminution) (Fig. 15.21). Supracondylar fractures are the most common elbow fracture in children younger than 10.
Fractures of the radial head are common in adults, but when nondisplaced or minimally displaced, they may be difficult to demonstrate with conventional radiography. Radial head fractures with extension into the articular surface must be differentiated from extra-articular radial neck fractures. Radial head fractures are classified in four types: nondisplaced or minimally displaced fractures; marginal fractures with partial displacement of the radial head, including impaction, depression, or angulation; comminuted fractures involving the entire head; and fracture and dislocation of the radial head (Fig. 15.22). An Essex–Lopresti fracture consists of a comminuted displaced fracture of the radial head associated with posterior subluxation of the distal ulna secondary to a tear of the entire interosseous membrane of the forearm. Fractures of the proximal ulna may involve the coronoid process or the olecranon, but the former rarely occurs as an isolated injury and is often associated with a posterior elbow dislocation.
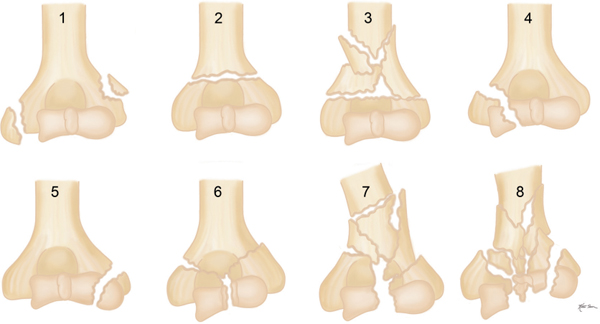
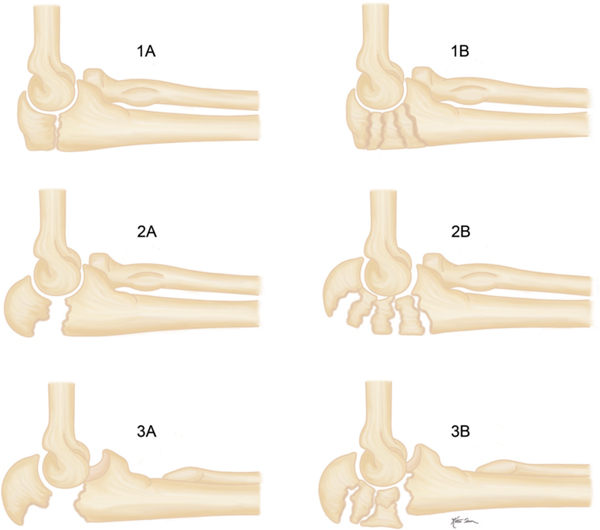
Olecranon fractures may be classified according to their location in the proximal, middle, or distal third of the olecranon. The proximal olecranon fracture may be extra-articular (avulsion fracture) or intra-articular, whereas the remaining fractures are all intra-articular. Transverse or oblique fractures in the middle third of the olecranon are most common. A more useful classification for the patient’s management is based on displacement, comminution, and ulnohumeral instability (Fig. 15.23).
Simple elbow dislocations without associated fractures may involve the ulna alone, the radius alone, or both the ulna and radius. Posterior and posterolateral dislocations of both ulna and radius account for 80% to 90% of all elbow dislocations. Anterior dislocations without associated fractures are exceedingly rare. Medial and lateral dislocations are likely to represent incompletely reduced posterior dislocations.
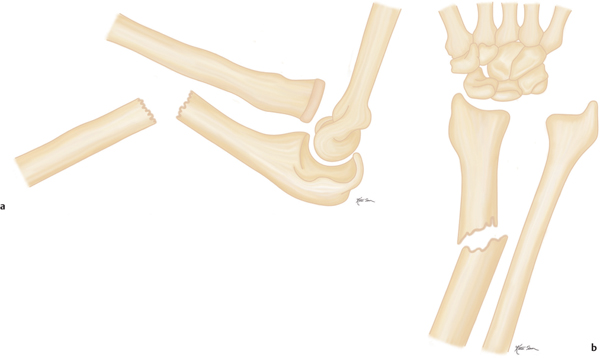
A Monteggia fracture (Fig. 15.24a) is the association of a proximal ulnar shaft fracture with dislocation of the radial head. Both the apex of angulation of the ulnar fracture and the dislocation of the radial head are anterior in type 1 (60%), posterior in type 2 (15%), lateral in type 3 (20%), and similar to type 1 but associated with a radius shaft fracture at the level of the ulnar fracture in type 4 (5%). A Galeazzi fracture (Fig. 15.24b) consists of a fracture of the distal third of the radius with angulation apex dorsal and medial (ulnar) associated with dorsal and medial dislocation of the ulna in the distal radioulnar joint. A Piedmont fracture is an isolated fracture of the distal radius shaft without involvement of the distal radioulnar joint. A nightstick fracture is an isolated ulnar shaft fracture caused by a direct blow to the forearm.
Distal radius fractures (Fig. 15.25) include (1) Colles fracture (extra-articular, usually occurring about 2–3 cm from the articular surface with typically radial and dorsal displacement and angulation apex volar associated frequently with an ulnar styloid fracture; in another definition of a Colles fracture, an intra- articular extension is also acceptable), (2) Smith fracture (extra- or intra-articular fracture with volar displacement of the distal fragment), (3) Barton fracture (intra-articular oblique fracture of the dorsal distal radius), (4) reverse (volar) Barton fracture (intra-articular oblique fracture of the volar distal radius), and (5) Hutchinson or chauffeur’s fracture (fracture of the radial styloid process).
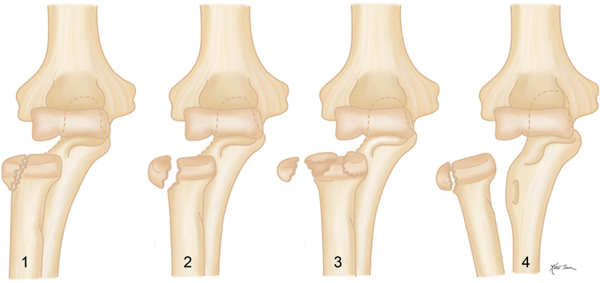
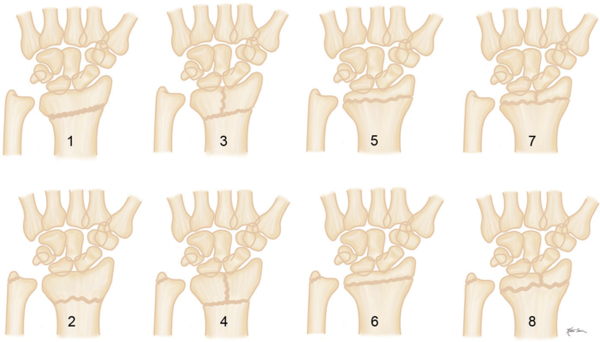
A more useful classification system of distal radius fractures was devised by Frykman that takes into consideration the involvement of both the radiocarpal and distal radioulnar joints, besides the ulnar styloid (Fig. 15.26).
Isolated intra-articular fractures of the distal ulna, including the ulnar styloid, are uncommon. Posttraumatic symptoms in the distal ulna are frequently caused by an injury to the triangular fibrocartilage complex (TFCC) that is best evaluated by MRI. The TFCC is the main stabilizing structure of the distal radioulnar joint. Subluxations and dislocations in this joint are therefore invariably associated with a disruption in the TFCC that besides being traumatic may also be inflammatory or degenerative in nature. An isolated injury to the TFCC or ulnar styloid fracture may be associated with a distal radioulnar joint subluxation or dislocation. The latter occurs frequently in combination with a radius fracture, for example, the radius shaft (Galeazzi fracture) or the radial head (Essex–Lopresti fracture).
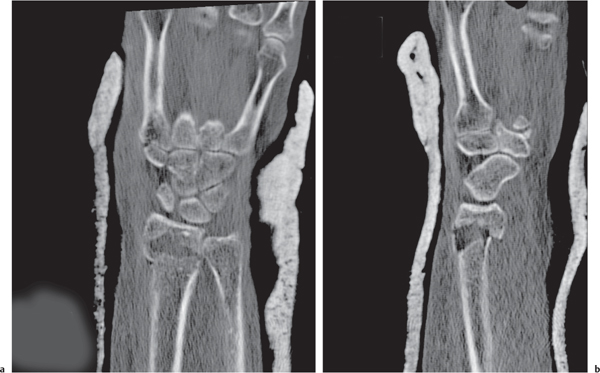
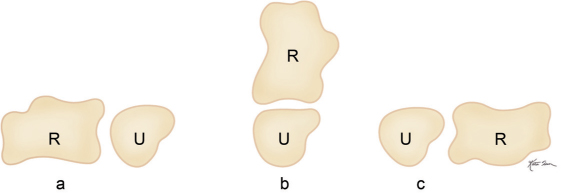
To diagnose a distal radioulnar joint instability, the wrist has to be imaged in pronation, neutral position, and supination of the forearm. In the normal wrist, the articulating surfaces of the distal radius and ulna are congruent in pronation and neutral position, but not in supination due to the normal configuration of the distal ulna (Fig. 15.27). Furthermore, minimal dorsal (posterior) subluxation of the ulna in pronation and minimal volar (anterior) subluxation of the ulna in supination may occur in the normal wrist. Comparison views of the opposite side are therefore helpful for diagnosing minor degrees of instability.
Severe wrist injuries may result in a positive or negative ulnar variance, which, however, is more commonly a normal variant. A positive ulnar variance (long ulna) may be associated with ulnar impaction (abutment) syndrome, in which the chronic impaction of the ulnar head against the TFCC and the ulnar-sided carpal bones results in progressive degeneration of these structures. This condition has to be distinguished from the ulnar impingement syndrome, which is associated with a negative ulnar variance. It is caused by a short distal ulna that impinges on the distal radius proximal to the sigmoid notch, resulting in scalloping of the distal radius or pseudoarthrosis formation at that site. A negative ulnar variance may also be associated with Kienböck disease.
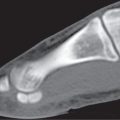
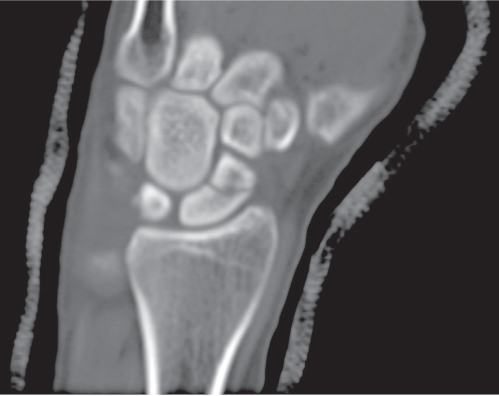
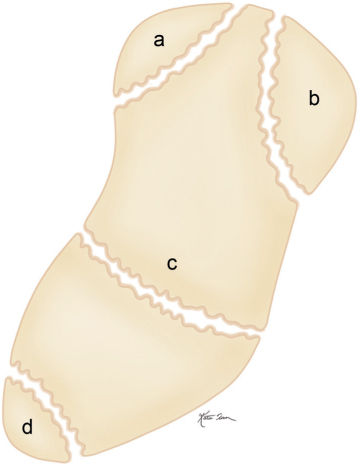
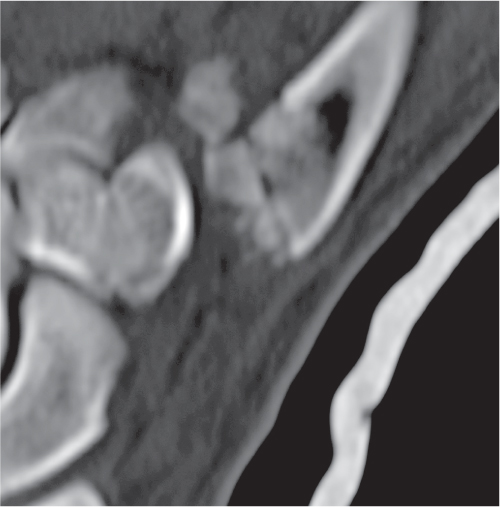
The scaphoid is the most commonly fractured carpal bone, accounting for approximately two thirds of all carpal fractures (Fig. 15.28). Scaphoid fractures can be classified according to the direction of the fracture line (e.g., horizontal, oblique, or vertical) or by anatomical location (Fig. 15.29). Waist fractures account for 80% of scaphoid fractures, proximal pole fractures for 15%, tuberosity fractures for 4%, and distal articular pole fractures for 1%. The vascular blood supply of the scaphoid occurs by volar and dorsal branches of the radial artery entering the bone in its distal half. Because of the retrograde vascular supply, the risk of complications markedly increases with fractures involving the proximal half of the scaphoid. Common complications of the scaphoid waist and even more so of proximal pole fractures include nonunion and avascular necrosis of the proximal fracture fragment.
The triquetrum is the second most fractured carpal bone, accounting for almost 20%. Most fractures of this bone are avulsion fractures associated with ligamentous damage. Transverse fractures may be associated with perilunate dislocation. Fractures in the remaining carpal bones are rare. In the lunate osteochondral and transverse body fractures as well as avulsions of the dorsal and palmar horns occur. Lunate fragmentation associated with Kienböck disease should not be confused with an acute fracture. The majority of trapezium fractures are either avulsions or vertical fractures of the body. Capitate fractures may be isolated or combined with other carpal fractures or fracture-dislocations. Complications in these fractures are rare, and they may heal even without immobilization. Hamate fractures are frequently associated with fractures of the fifth or less frequently fourth metacarpals. Fracture of the hook of the hamate is the most common hamate fracture. Fractures of the pisiform and trapezoid are the rarest carpal bone fractures.
Carpal instability can be classified into static or dissociative and dynamic or nondissociative types. Imaging of the latter may be difficult and usually requires a functional study, such as fluoroscopy or cineradiography. Triquetrohamate instability presents with painful clicking caused by abnormal motion between the triquetrum and hamate. Static instability patterns include volar, dorsal, or ulnar translocation (subluxation) of the carpus with regard to the distal radius. Instabilities within the proximal carpal row include scapholunate and lunotriquetral dissociations and scapholunate advanced collapse (SLAC). Two other major carpal instability patterns are dorsal (DISI) and volar (VISI) intercalated segmental instability (Fig. 15.30). In sagittal projection with the wrist in neutral flexion-extension, the angle between the axes of the scaphoid and lunate ranges from 30° to 60°. In DISI, the lunate is tilted dorsally 15° or more, and the scapholunate angle measures > 60°. In VISI, the lunate is tilted volarly 15° or more, and the scapholunate angle measures < 30°. DISI is associated with rotary subluxation of the scaphoid (distal pole of the scaphoid is tilted toward the palm) and scapholu-nate dissociation (scapholunate distance at the site of ligamentous insertion measures > 4 mm in coronal plane). In VISI, the capitate is often tilted dorsally, resulting in a capitolunate angle > 30° (normal 0–30°), and lunotriquetral dissociation may be associated. Scapholunate dissociation and rotary subluxation of the scaphoid represent stage 1 of four sequential stages of dislocations involving the lunate. Stage 2 (perilunate dislocation) represents a dorsal dislocation of the capitate (Fig. 15.31). Stage 3 (midcarpal dislocation) consists of an anterior subluxation of the lunate associated with a dorsal dislocation of the capitate. Stage 4 (lunate dislocation) represents a complete anterior lunate dislocation associated with a dorsal dislocation of the capitate (Fig. 15.32). These four sequential stages of lunate injuries are also referred to as the lesser arc pattern, whereas a greater arc injury involves fracture of any carpal bones adjacent to a dislocated lunate (usually a perilunate dislocation). In these cases, the prefix trans indicates which bone is fractured. The most common carpal fracture-dislocation is the transscaphoid perilunate dislocation. A pure albeit rare greater arc injury consists of a transscaphoid, transcapitate, transhamate or transtriquetral perilunate dislocation.
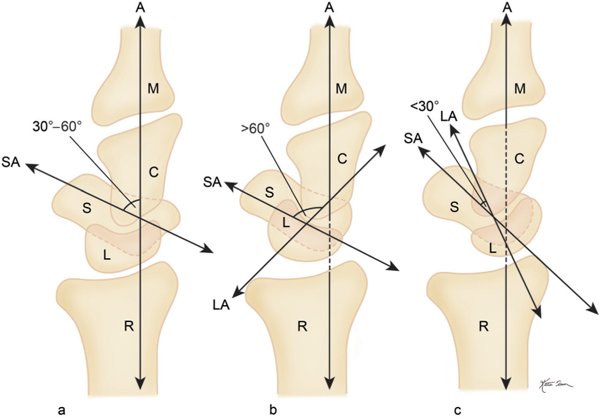

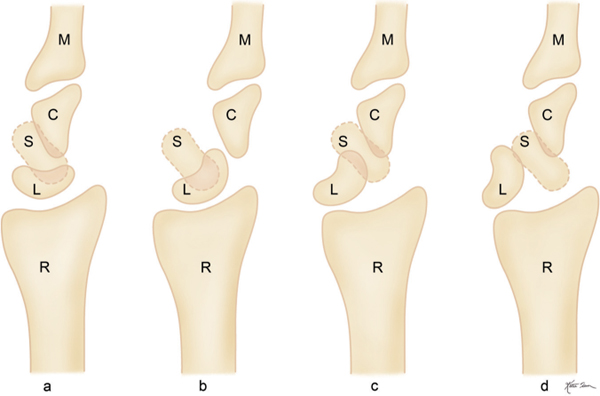
C | capitate |
L | lunate |
M | third metacarpal |
R | radius |
S | scaphoid |
Scaphoid dislocation is rare. An isolated radiovolar dislocation of the scaphoid with intact distal carpal row has to be differentiated from the same scaphoid dislocation associated with disruption of the distal carpal row evident by proximal migration of the radial half of the carpus including radial dislocation in the capitolunate joint.
The majority of first carpometacarpal injuries are fracture dislocations rather than pure dislocations, which are almost always dorsoradial. Bennett and Rolando fractures are intraarticular fractures of the base of the first metacarpal frequently associated with dorsoradial subluxation/dislocation of the shaft. In the noncomminuted Bennett fracture, a small fragment on the volar and ulnar aspect of the base of the first metacarpal remains in articulation with the trapezium, whereas the remaining first metacarpal is dorsally and radially displaced. The Rolando fracture (Fig. 15.33) is a comminuted Bennett fracture, often with a Y, V, or T configuration that is not infrequently associated with small, loose intra-articular bony fragments that are readily appreciated by CT and almost impossible to diagnose with conventional radiography. Dislocation in the second through fifth carpometacarpal joints are rare high-energy injuries, almost always dorsal, and usually associated with fractures of the adjacent carpal and metacarpal bones.
Metacarpal fractures can be differentiated according to their anatomical location in head, neck, shaft, and base fractures. A boxer fracture is a metacarpal neck fracture with apex dorsal angulation. It may occur in any metacarpal with the exception of the thumb but is most common in the fifth. Residual angular deformity with apex dorsal is of less serious consequence in the metacarpals of the fourth and fifth finger, in which there is some mobility at the carpometacarpal joints, than in the second and third fingers, where there is no mobility in the corresponding joints, resulting in protrusion of the metacarpal heads in the palm that may be associated with a painful grip.
Gamekeeper’s (skier’s) thumb is an injury to the ulnar collateral ligament of the first metacarpophalangeal joint with or without a bony avulsion from the base of the proximal phalanx resulting from a violent abduction of the thumb, most often a skiing accident. A sesamoid fracture must be differentiated in the presence of volar tenderness. Dorsal dislocations are the most common in metacarpophalangeal joints 2 to 5. They are really subluxations, as some contact remains in these joints. The volar plate stays volar or distal to the metacarpal head.
Phalangeal fractures are classified based on their anatomical location within the bone (head, neck, shaft, and base) and further modified by the direction of the fracture plane (transverse, oblique, spiral, or comminuted) and the measurable degree of displacement and angulation. Dorsal base fractures include a mallet fracture, in which an avulsion injury at the base of the dorsal aspect of the distal phalanx is associated with damage to the extensor mechanism, producing a flexion (mallet) deformity in the distal interphalangeal joint. The most common volar plate fracture represents an intra-articular avulsion fracture in the base of the middle phalanx at the volar plate attachment site, usually secondary to dorsal dislocation of the proximal interphalangeal joint.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree