15 Trauma and Fractures: Spine
Cervical (C) spine injuries are caused by hyperflexion (e.g., anterior wedge or compression fracture, teardrop fracture, anterior subluxation, and bilateral jumped facets with anterior subluxation of the superior vertebra), hyperextension (e.g., avulsion anteroinferior corner of a vertebral body, typically at C2, or C3, and hangman’s fracture), hyperrotation (e.g., rotary atlantoaxial subluxation), hyperflexion and rotation (e.g., unilateral jumped facet), lateral hyperflexion (e.g., unilateral pillar fracture), and vertical compression (e.g., Jefferson fracture and burst fractures C3–C7). Differentiation between stable and unstable cervical spine injuries is of utmost importance (Table 15.5).
Occipital condyle fractures were classified into three types by Anderson and Montesano. Type 1 is an impacted comminuted condylar fracture with minimal displacement secondary to axial loading. It is usually stable. Type 2 injuries are potentially unstable injuries caused by a shear mechanism that results in an oblique fracture extending from the condyle into the skull base. Type 3 fractures are unstable avulsion injuries secondary to rotation and lateral bending, presenting with a transverse fracture line through the occipital condyle (Fig. 15.78). Any occipital condylar fracture associated with craniocervical dissociation is unstable.
Craniocervical dissociation is considered unstable with translation or distraction > 2 mm in any plane. Occipitocervical dislocations can be classified according to the direction of displacement of the occiput with regard to C1 in anterior (type 1), vertical (distraction, type 2), and posterior (type 3) plane. The degree of instability may be underestimated with CT, as spontaneous reduction occurs, and the vast majority of lesions are ligamentous involving the three main craniocervical stabilizers, that is, the alar ligaments (occipital condyles to dens), the tectorial membrane (clivus to C2 portion of the posterior longitudinal ligament), and the transverse ligament crossing behind the dens between the lateral masses of the atlas. MRI is the imaging modality of choice for these injuries.
Fractures of the atlas (C1) may be classified into (1) stable posterior arch fractures caused by hyperextension; (2) isolated anterior arch fractures ranging from minimally displaced to comminuted, which may be unstable; (3) unilateral comminuted or lateral mass fractures caused by rotation or lateral flexion forces, which are frequently unstable; and (4) burst (Jefferson) fractures, which are unstable. In the Jefferson fracture (Fig. 15.79), the axial load resulting from a blow to the vertex of the head drives the lateral masses outward, resulting in bilateral symmetrical fractures of the anterior and posterior arches of C1, which are invariably associated with disruption of the transverse ligament.
Stable injuries: |
Fracture of posterior arch of C1 |
Rotary subluxation C1–C2 |
Odontoid fracture (type 1) |
Extension teardrop fracture |
Compression fracture (anterior two thirds of vertebral body) |
Laminar fracture |
Transverse process fracture |
Spinous process fracture (including clay shoveler’s fracture) |
Unilateral perched or locked facet |
Subluxation (≤ 2 mm) |
Stable or unstable injuries: |
Occipital condyle fracture |
C1 anterior arch or lateral mass fractures |
Atlantoaxial subluxation |
Odontoid fracture (type 3) |
Facet and pillar fractures |
Subluxation (3 and 4 mm) |
Unstable injuries: |
Jefferson fracture |
Odontoid fracture (type 2) |
Hangman’s fracture |
Flexion teardrop fracture |
Hyperextension fracture-dislocation |
Burst fracture (C3–C7) |
Occipitocervical subluxation (> 2 mm) |
Bilateral jumped (perched or locked) facets |
Subluxation (≥ 5 mm) |
Dislocation |


Atlantoaxial subluxations may be rotational or transitional and are frequently nontraumatic (e.g., rheumatoid arthritis and Down syndrome [trisomy 21]). Rotational injuries range from mild subluxation to complete dislocation of the atlantoaxial lateral masses. Anterior C1–C2 subluxation is diagnosed when the distance between the anterior arch of C1 and the dens measures 3 mm or more in adults and 5 mm or more in children. Distraction atlantoaxial injuries are considered to be a variant of craniocervical dissociation. A distraction injury in either the occiput–C1 or C1–C2 joint is present when the vertical separation is > 2 mm. At times cranial traction is required for the proper diagnosis.
Injuries to the axis (C2) include fractures of the odontoid process (dens) and traumatic spondylolisthesis of C2 (hangman’s fracture). Dens fractures are classified based on the anatomical location of the fracture line (Fig. 15.80). Type 1 is an oblique fracture near the tip of the dens representing an avulsion at the insertion of the alar ligament. This fracture must be differentiated from an unfused ossification center at the tip of the dens (ossiculum terminale of Bergman), typically separated from the dens by a transverse lucent line. Type 2 injuries are unstable transverse fractures through the base of the dens and carry a high risk of nonunion. An unfused dens (os odontoideum) characteristically has a rounded inferior border with a smooth, thin cortical margin. Nonunion of a dens fracture may present in a similar fashion. Type 3 fractures extend from the base of the dens into the vertebral body and have a wider fracture surface (Fig. 15.80). These fractures tend to be stable but are not invariably so. Hangman’s fractures (Fig. 15.81) occur most commonly in motor vehicle accidents, when the face strikes the wind-shield, forcing the neck into hyperextension. Type 1 injury is a nondisplaced fracture through the pedicles (interarticular pars) of C2 extending between the superior and inferior facets. Type 2 fracture is a displaced interarticular pars fracture without (2A) or with (2B) disruption of the discoligamentous complex at C2–C3. Type 3 injury is a type 2 fracture with dislocation of the C2–C3 facet joints (Fig. 15.82).
Subaxial (middle and lower cervical spine) injuries are classified based on injury mechanism, anatomical location, or a combination thereof. There are four basic types of injury mechanism in the subaxial spine: hyperflexion, compression, hyperextension, and lateral hyperflexion. Depending on the severity of the trauma, stable and unstable injuries occur with each of the four aforementioned injury mechanisms. Combination injury patterns, such as compression (axial loading) with either hyperflexion or hyperextension, however, are common. Hyperflexion injuries are typically associated with some degree of compression in the anterior column (anterior aspect of the vertebrae) and some degree of distraction in the posterior column, whereas the opposite applies for hyperextension injuries. Anterior or posterior translation may further complicate these injury patterns.
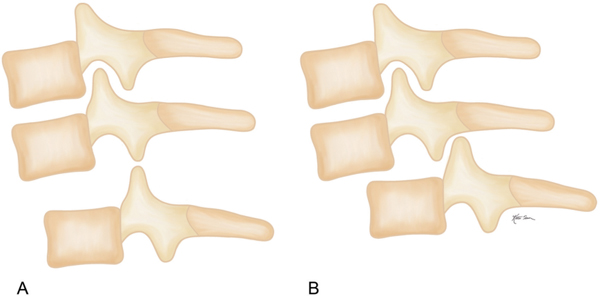
In the subaxial cervical spine, stable hyperflexion injuries include compression (anterior wedge) fractures and clay shoveler’s fractures, predominantly unstable injuries, such as subluxations and dislocations of the facet joints, and highly unstable injuries, such as teardrop fractures (Fig. 15.83). In a compression (anterior wedge) fracture, there is anterior compression of the vertebral body, and although the posterior ligament complex is stretched, it remains intact (Fig. 15.84a). The highly unstable flexion teardrop fracture in the middle and lower C spine most commonly involves C5. The vertebral body is split into a smaller anteroinferior tear-drop fragment and a larger posterior fragment that is displaced posteriorly into the spinal canal. The anterior and posterior longitudinal ligaments, ligamentum flavum, and interspinous ligaments are all disrupted, resulting in widening of the facet joints (“facet gapping”), and fractures of the posterior elements, most frequently of the spinous process, are associated (Fig. 15.84b). Subluxed (perched) and dislocated (locked) facet joints are unilateral or bilateral hyperflexion (distraction) injuries with tearing of the corresponding joint capsules and ligamentous complex (Fig. 15.85). An isolated hyperflexion sprain evident by widening of both the interspinous distance and the posterior aspect of the facet joints can be considered the mildest form of a posterior column distraction injury. In bilateral interlocking (jumped) facets, the inferior articular facets of the upper vertebra are positioned either on top (perched facets) or in front (locked facets) of the superior facets of the lower vertebra (Fig. 15.86). This condition is associated with anterior subluxation of the involved upper vertebra and extensive injuries of all spinous ligaments at that level. In a unilateral locked facet, a rotational force component is also present besides the hyper-flexion. In the absence of disk space widening or anterior subluxation, this injury is considered mechanically stable. A clay shoveler’s fracture is an oblique or vertical avulsion fracture of the spinous process of C6 or C7 (less commonly, T1 to T3) caused by a sudden load on the flexed spine. Occasionally, more than one spinous process is involved.







Compression (axial loading) injuries in the subaxial cervical spine vary from stable compression fracture to unstable burst fractures (Fig. 15.87). Compression fractures resulting from axial loading are similar in appearance to compression (anterior wedge) fractures secondary to hyperflexion, although the latter may demonstrate more anterior wedging. Burst fractures characteristically demonstrate extensive vertebral body comminution, varying degrees of height loss, and, most importantly, posterior vertebral involvement with retropulsion, preferentially of the posterosuperior aspect of the fractured vertebral body.
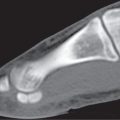
Hyperextension injuries in the middle and lower C spine result in distraction injuries in the anterior column and compression fractures of the posterior elements (Fig. 15.88). They occur most commonly during motor vehicle accidents involving rear-end collisions (whiplash injuries). An extension teardrop fracture (Fig. 15.89) is a stable avulsion fracture arising from the anteroinferior corner of a vertebral body and is typically located in the upper C spine (e.g., C2 and C3). The vertical height of this teardrop fracture fragment usually exceeds its horizontal dimension. No other fracture or subluxation is associated with this injury. hyperextension fracture-dislocation injuries may be highly unstable injuries despite the fact that they may produce only very subtle bony abnormalities. These injuries with torn anterior longitudinal ligaments may present with an anteriorly widened disk space and small avulsion fractures at the insertion site of the anulus fibrosus. Retrolisthesis of the vertebra above the discal injury is frequently also present, but it may be only minimal. Other manifestations include unilateral or bilateral arch fractures (pedicle, facet, and lamina), which may be associated with varying degrees of anterolisthesis. Involvement may be at multiple levels.
Lateral hyperflexion injuries occur by compression of one side of the spine. With further energy, the contralateral side may fail under tension. The most common fracture produced is unilateral wedging of the vertebral body and its associated lateral mass. Fractures of the arch similar to those occurring in hyperextension injuries are also present in the majority of cases that may result in lateral translation of the fracture fragments (floating lateral mass).
Fractures in the thoracolumbar spine can be classified based on the injury mechanism in compression fractures, burst fractures, Chance fractures (distraction fractures or seat-belt injuries), and fracture-dislocations. To assess fracture stability, Denis introduced the concept of the three columns in the thoracolumbar spine (Fig. 15.90). The anterior column comprises the anterior two-thirds of both the vertebral body and the disk and the anterior longitudinal ligament. The middle column consists of the posterior third of both the vertebral body and the disk, the posterior longitudinal and the pedicles. The posterior column includes the posterior portion of the neural arch (lamina) with all its appendices (transverse process, superior and inferior articular process, and spinous process) and the ligamentum flavum, the supraspinous and interspinous ligaments, and the capsule of the facet joints. It is the opinion of the author of this chapter, however, that reducing the middle column from the posterior third of the vertebral body to its posterior cortex is more appropriate for the differentiation between stable and unstable injuries. Any fracture involving the middle column defined in this way must be considered unstable, as an isolated fracture involvement of the middle column is not possible. In the original three-column classification system, one-column fractures are considered stable and three-column fractures unstable, whereas two-column fractures may be stable or unstable (Table 15.6).



A | anterior column |
AF | anulus fibrosus |
AL | anterior longitudinal ligament |
IL | interspinous ligament |
LF | ligamentum flavum |
M | middle column |
NP | nucleus pulposus |
P | posterior column |
PL | posterior longitudinal ligament |
SL | supraspinous ligament |
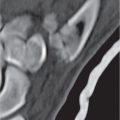
Compression fractures (Fig. 15.91) occur from anterior or, less commonly, lateral flexion with axial loading. Typically, the compression fracture is a stable injury with involvement limited to the anterior column. Buckling of the cortex near the upper end plate (rarely the lower end plate or both end plates) or an arc of irregular bony fragments displaced circumferentially around the vertebral body may be the only finding. However, a loss of height of the anterior vertebral body ranging from minimal to < 50% is the typical presentation. Preferential involvement is the superior aspect of the vertebral body (Fig. 15.92). Severe compression fractures may extend into the middle column, and distraction injuries in the posterior ligamentous complex may be associated, resulting in unstable compression fractures. The most common site of involvement is the lower thoracic and upper lumbar spine, in order of frequency affecting L1, L2, T12, T7, and L3.


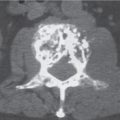
All burst fractures (Fig. 15.93) should be considered unstable, although this assessment is not unanimously shared in the orthopedic literature. They result from axial loading that may be associated with flexion. The thoracolumbar junction with T12, L1, and L2 is the most common site of involvement. The burst fracture is a comminuted fracture with centrifugal fragment displacement, resulting in an increased vertebral body diameter (especially in the sagittal plane), increased interpedicular distance, and splaying of the facet joints. The anterior vertebral wedging is similar to a compression fracture, but the burst fracture differs from the latter by the characteristic retropulsion of the posterosuperior corner of the fractured vertebral body into the spinal canal. Posterior column fractures may be associated with burst fractures and include vertical fractures of one or both laminae and the spinous process (Fig. 15.94).

Chance fractures (distraction fractures, seat-belt injuries) are hyperflexion injuries subjecting the posterior and middle vertebral columns, or all three columns, to distraction forces (Fig. 15.95). Such injuries occur most frequently at the thoracolumbar junction, particularly at L1 or L2. They rarely occur through bone alone and are most commonly the result of osseous and ligamentous failure beginning posteriorly and propagating anteriorly. The imaging findings depend on whether the injury is predominantly osseous or ligamentous. Horizontal fractures originating in the spinous process or lamina with or without involvement of the transverse processes, extending through the pedicles into the vertebral body without significant damage to ligamentous structures, is a typical presentation of a primarily osseous manifestation. Its constant feature is transverse fracture without dislocation or subluxation. Occasionally, there is also mild compression of the anterior aspect of the vertebral body. A primarily soft tissue injury presents with disruption of the posterior ligamentous complex, resulting in interspinous widening and increased height of the intervertebral foramina; widening, superior subluxation, perching, or locking of the facet joints may be evident. With disruption of the posterior fibers of the anulus fibrosus, widening of the posterior portion of the disk space may be apparent. In a two-level injury, distraction of the posterior ligamentous complex occurs at one level, while the disk involvement affects the next level farther down (Fig. 15.96).
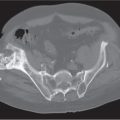
Fracture-dislocations of the thoracolumbar spine are highly unstable injuries involving all three columns (Fig. 15.97). Transitional deformity, which can occur in the sagittal and/or coronal planes, is the hallmark of this injury. This intervertebral subluxation or dislocation is typically not associated with loss of height of a vertebral body. The spinal distribution of the injury is bimodal, with one peak at the T6–T7 level and the second peak at the thoracolumbar junction. Fracture-dislocations result from various forces, including shear, rotation, and distraction (Fig. 15.98). In shear injuries, anterior, posterior, and/or lateral subluxation/dislocation of the spine is associated with severely comminuted fractures in the posterior column, including the facet joints, transverse and spinous processes, and laminae, which may be free-floating. Rotational injuries are associated with a slice fracture of the vertebral body, multiple rib and/or transverse process fractures, dislocations of the costotransverse joints, usually unilateral displaced fractures of the articular facets, and rotary malalignment of two vertebrae located above and below the injury. The rotational slice fracture is a horizontal fracture involving the superior end plate. This fragment is displaced as a unit together with the adjacent intervertebral disk and upper vertebra pivoting relative to the caudal vertebra below the slice fracture. A fracture-dislocation of the distraction type differs from a Chance fracture (seat-belt injury) by the fact that the entire disk is torn, allowing the vertebra above to translate on the vertebra below. A traumatic spondylolisthesis can be considered a manifestation of a fracture-dislocation injury, but it is rare when compared with other nontraumatic conditions, such as degenerative changes in the disk and facet joints and chronic defects of the pars interarticularis (spondylolysis). These conditions are dealt with in greater detail in the spine section.



Isolated transverse process fractures in the lumbar spine result from lateral hyperflexion injuries or, less commonly, from a direct blow. They may be multiple, most commonly involve the levels of L3 and L4, and are stable. L5 transverse process fractures are frequently associated with unstable pelvic fractures.
Traumatic fractures of the spine have to be differentiated from subacute or chronic compression fractures associated with osteopenia (insufficiency fractures). These fractures are frequently located in the midthoracic spine, whereas traumatic fractures are preferentially located in the thoracolumbar region. A narrow zone of increased density below the fractured end plate, produced by impacted trabeculae and/or attempted fracture healing, is commonly present in compression fractures associated with osteoporosis (Fig. 15.99).



Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree