16 Skull Base and Cranial Nerves
16.1 Introduction
The cranial nerves have a critical role in neurologic function, and have an intimate relationship with the skull base. Abnormalities in one can affect the other. The cranial nerves have characteristic functions, and dysfunction in them may present with specific or nonspecific clinical signs. Knowledge of the anatomy of the cranial nerves and the skull base can aid in determining a cause for many neurologic conditions. The function of each cranial nerve may involve a combination of afferent (sensation), special sensation (taste), efferent (motor), and parasympathetic function.
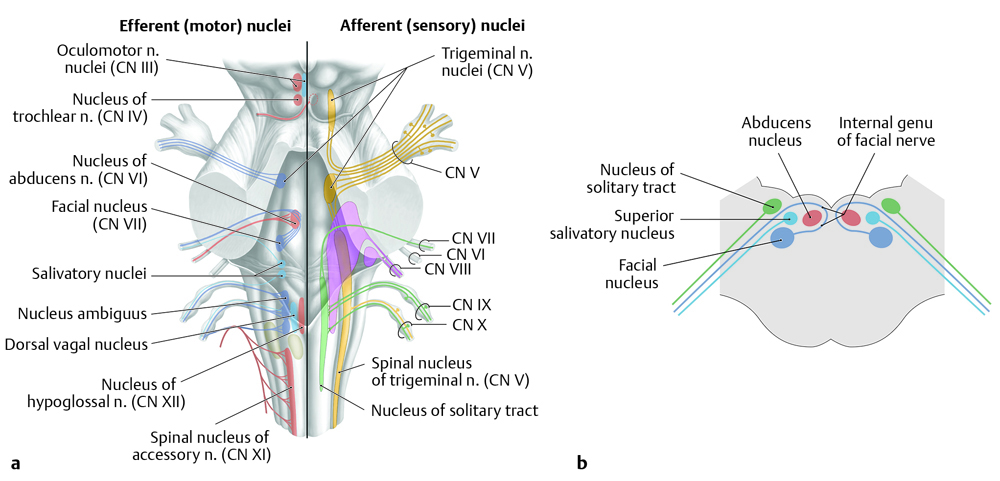
On a segmental basis (with minor variations), each cranial nerve has a nucleus (Fig. 16.1), an intra-axial (fascicular) segment, a cisternal segment, an interdural segment, a foraminal segment, and an extraforaminal segment (Fig. 16.2). 1, 2, 3 Some pathologic processes uniquely affect certain cranial nerves, whereas others are more nonspecific in the nerves they involve. This chapter discusses the function and anatomic features of each of the 12 cranial nerves together with characteristic pathologic conditions affecting them, and reviews conditions that affect the cranial nerves without specific predilections for one or another. The chapter begins with a brief review of the anatomy of the skull base.

16.2 Skull-Base Anatomy
The skull base is variably defined and comprises several bones, most prominently the sphenoid and temporal bones, with additional involvement of portions of the occipital and frontal bones (Fig. 16.3). 4 ,? 5 ,? 6 ,? 7 ,? 8 The anterior skull base includes the cribriform plate (consisting of portions of the frontal and ethmoid bones), which is perforated by branches of the olfactory nerve (cranial nerve [CN] I) and roofs of the orbits (formed from portions of the frontal and sphenoid bones). The central portion of the sphenoid bone, the basisphenoid, contains the sella turcica. The basisphenoid and basiocciput are joined by a spheno-occipital synchondrosis, which eventually fuses and forms a structure known as the clivus. Between the basisphenoid and the lesser wing of the sphenoid bone is the optic canal (carrying CN II), and between the basisphenoid and the greater wing of the sphenoid is the superior orbital fissure (carrying CN III, IV, V1, and VI). Within the greater wing of the sphenoid bone is an anteriorly directed canal known as the foramen rotundum (carrying V2), and an inferiorly directed canal known as the foramen ovale. Posterolateral to the foramen ovale is the foramen spinosum, which carries the middle meningeal artery.
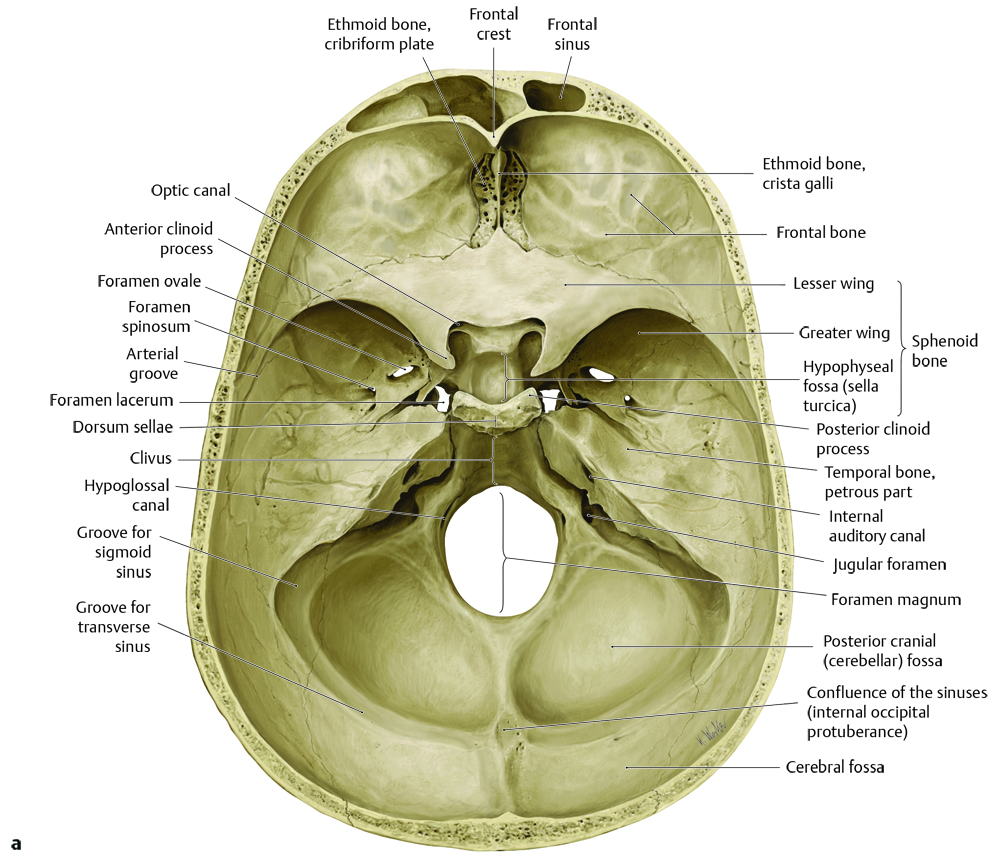
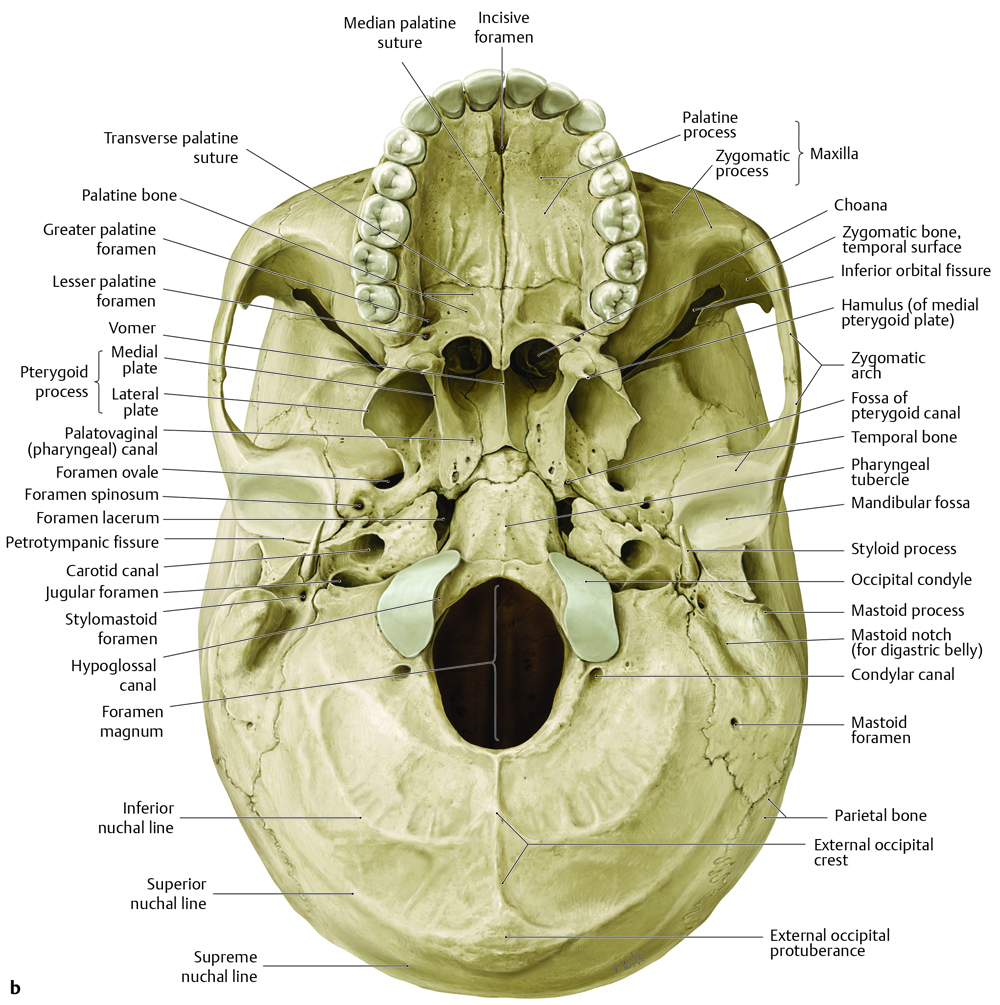
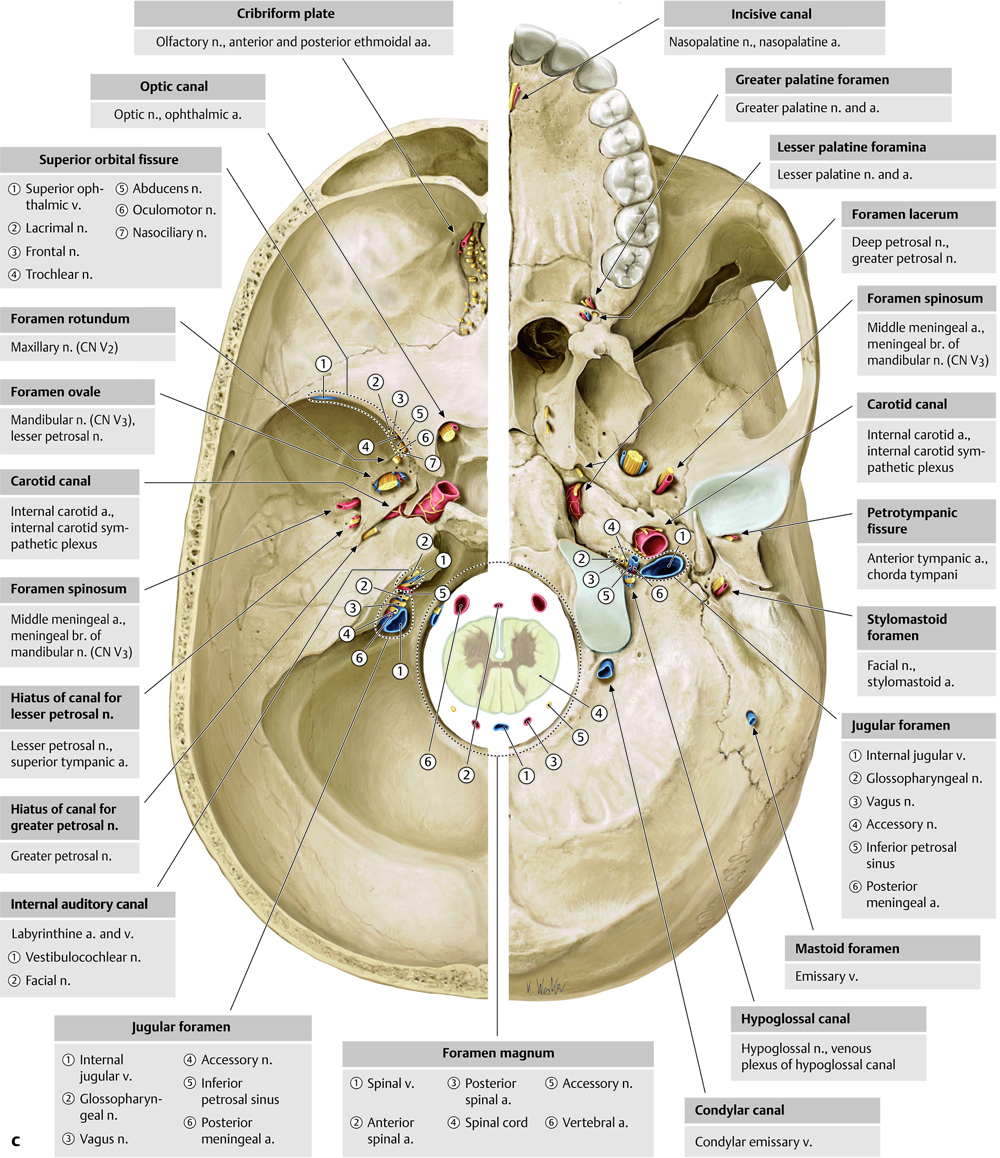
Within the petrous temporal bone is the internal auditory canal, which carries CN VIII to the structures of the inner ear and acts as a conduit for the facial nerve (CN VII). Between the portion of the temporal bone containing the inner ear and the clivus is the apex of the petrous temporal bone, a structure that can occasionally be pneumatized, with the possible development of an infectious/inflammatory process known as petrous apicitis (see Gradenigo’s syndrome in the section of this chapter on CN VI). The pneumatized portion of the temporal bone can also, in the case of a cholesterol granuloma, contain a chronic accumulation of obstructed fluid and debris. On magnetic resonance imaging (MRI), asymmetric penumatization of the petrous apex can be mistaken for an enhancing lesion of the skull base because the marrow on the nonpneumatized side will appear bright on T1 weighted (T1 W) imaging as compared with precontrast imaging and fat-saturated imaging. When available, a CT scan can help confirm the diagnosis of a pseudolesion of the petrous apex and prevent unnecessary surgical intervention. The petrous temporal bone also contains the carotid canal.
The jugular foramen is located between the petrous and mastoid portions of the temporal bone and the occipital bone, and carries the jugular bulb, which is the transition between the sigmoid sinus and the internal jugular vein. The jugular foramen is parcellated into the posterior pars vascularis (carrying CN X and XI), and the smaller anteromedial pars nervosa (carrying CN IX). Within the exoccipital portion of the occipital bone are the hypoglossal canals, carrying the right and left hypoglossal nerve (CN XII).
16.2.2 Cavernous Sinus
The cavernous sinus is a network of venous structures along the lateral margins of the sella turcica bilaterally, and portions of the internal carotid artery course through this venous network. Along the lateral margins of the cavernous sinus course segments of CN III, IV, and the ophthalmic and maxillary branches of CN V. The abducens nerve (CN VI) courses within the cavernous sinus (Fig. 16.4).

16.2.1 Pterygopalatine Fossa
An area of the skull base worthy of specific discussion is the pterygopalatine fossa, which is located between the greater wing of the sphenoid bone and the pterygoid process of the sphenoid bone (Fig. 16.5). This is an area through which multiple nerves and vessels pass, and it can be involved in the perineural spread of disease to distant parts of the face, skull base, and brain. The pterygopalatine fossa has two posterior access points, consisting of foramen rotundum, which carries CN V2, and the vidian canal, which carries the vidian nerve. The vidian nerve is a combination of preganglionic parasympathetic fibers from the greater superficial petrosal nerve (GSPN) from CN VII, and postganglionic sympathetic fibers from the deep petrosal nerve. The parasympathetic fibers synapse in the pterygopalatine ganglion, with the postganglionic fibers ascending through the inferior orbital fissure into the posterior orbit. The anterior outlet of the pterygopalatine fossa is the infraorbital canal, which carries the infraorbital branch of CN V2. Inferiorly are two canals for nerves innervating the palate, the greater and lesser palatine nerves, which traverse the greater and lesser palatine canals, respectively. Lateral access to the pterygopalatine fossa is from the pterygomaxillary fissure, through which the internal maxillary artery enters the pterygopalatine fossa. Medially is the sphenopalatine foramen, which is the communication between the pterygopalatine fossa and the sinonasal cavity, and where distal branches of the internal maxillary artery extend to supply the nasal mucosa. The sphenopalatine foramen is also the location of the origin of a particular tumor known as a juvenile nasal angiofibroma, a highly vascular tumor that presents in adolescent males with recurrent unilateral epistaxis.

16.3 Anatomy and Nerve-Specific Pathology
16.3.1 Cranial Nerve I–Olfactory Nerve
The olfactory nerve is an afferent nerve involved in the sensation of smell. In formal terms, it is a tract and is part of the central nervous system (CNS), with its myelination produced by oligodendrocytes. The olfactory nerve courses within the olfactory groove along the superior aspect of the cribriform plate (Fig. 16.6). The nerve is subject to traumatic injury in the case of fractures of the central skull base. Congenital absence of the olfactory nerve results in anosmia (inability to smell), and can be associated with hypogonadotropic hypogonadism in Kallman’s syndrome. Hypoplasia of the olfactory nerve can be seen in patients with septo-optic dysplasia. Abnormalities in the olfactory pathway can present with dysgeusia (abnormality or loss of the sensation of taste).

16.3.2 Cranial Nerve II–Optic Nerve
The optic nerve carries afferent fibers involved in sight (Fig. 16.7). The nerve begins in the optic disc in the posterior aspect of the globe of the eye, courses posteriorly in the orbit of the eye, passes through the optic canal, and reaches the optic chiasm. Within the chiasm, fibers of the optic nerve from the nasal retinal field (temporal visual field) of one eye decussate and join with fibers from the temporal retinal field (nasal visual field) of the contralateral eye, which do not decussate. At the optic chiasm, the tracts consisting of temporal retinal fibers of one eye and nasal retinal fibers of the contralateral eye extend posterolaterally as the right and left optic tracts, respectively, which then continue to the right and left lateral geniculate nuclei.

The optic nerve is formally a part of the CNS, with its myelination produced by oligodendrocytes rather than Schwann cells. Therefore, tumors of the optic nerve are gliomas rather than optic nerve schwannomas. Additionally, the optic nerve is susceptible to inflammatory and demyelinating processes (optic neuritis) that affect the CNS (e.g., multiple sclerosis, acute disseminated encephalomyelitis [ADEM], neuromyelitis optica [NMO]). A sellar/suprasellar mass like a pituitary macroadenoma or craniopharyngioma that impinges the optic chiasm will affect visual fibers decussating in the chiasm, resulting in a bitemporal hemianopsia.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree