2 Arachnoid Granulations
2.1 Case Presentation
2.1.1 History and Physical Examination
A 17-year-old girl with a past medical history of migraine headaches since the age of 14 years presents with a severe headache.
On neurological examination, CNs II–XII were intact. There was no evidence of papilledema on fundoscopy examination.
2.1.2 Imaging Findings and Impression
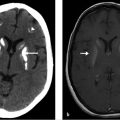
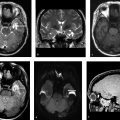
MRI of the brain with contrast shows an oval lesion (white arrows; ▶ Fig. 2.1a,b) in the distal left transverse sinus, which is isointense to cortex on T2-weighted imaging (T2WI) and on fluid-attenuated inversion recovery (FLAIR; ▶ Fig. 2.1c) and hypointense on T1-weighted imaging (T1WI). The lesion is seen as a filling defect on postcontrast T1WI (▶ Fig. 2.1d) and does not show any susceptibility on susceptibility weighted imaging (SWI; ▶ Fig. 2.1e) to suggest a venous clot. An intralesional vein (black arrow) is seen draining the area. All these features are consistent with an arachnoid granulation.

2.2 Differential Diagnosis
Arachnoid granulation:
Represent enlarged arachnoid villi and are seen as nonenhancing filling defects within venous sinuses causing scalloping of the inner table when large.
Often seen is a superficial cortical vein draining into the arachnoid granulation.
Absence of susceptibility on gradient echo (GRE) images.
Venous thrombosis:
Usually involves an entire segment of one sinus or multiple sinuses.
May be associated with mastoid inflammation.
Can extend into cortical veins and may involve the distal sigmoid sinus and jugular vein, which does NOT occur with arachnoid granulations.
Unlike arachnoid granulations, acute thrombus is hyperdense to the brain on CT, hyperintense on T1WI, and hypointense on FLAIR sequences and shows susceptibility artifact on GRE/SWI.
Intrasinusal tumor:
Enhances with gadolinium administration.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree