22 Temporal Bone
22.1 Introduction
The temporal bone has a complex anatomy and varied functions, and its cross-sectional imaging tends to be an intimidating endeavor. It is to be hoped that a basic understanding of the anatomy of the temporal bone, and a systematic approach to the various pathologic entities that can affect it, can reduce the anxiety associated with, and improve the diagnostic yield of, its imaging.
Imaging of the temporal bone in children is done for several reasons. First and foremost is hearing loss. Additional reasons for imaging the temporal bone include infection, trauma, and facial nerve pathology. The mainstay modalities for imaging the temporal bone are computed tomography (CT) and magnetic resonance imaging (MRI).
22.2 Anatomy
The temporal bone is a bone of complex anatomy located within the skull base. Its main parts include its petrous portion, tympanic portion, and mastoid portion, all of which are parts of the skull base, and its squamous and zygomatic portions (Fig. 22.1). The tympanic portion of the temporal bone contains the middle ear cavity, also known as the tympanic cavity. The petrous temporal bone can be subdivided into the labyrinthine portion and the petrous apex (pathologic processes involving the petrous apex are further discussed in Chapter 16). The external auditory canal leads to the middle ear, which is separated from the outer ear by the tympanic membrane.
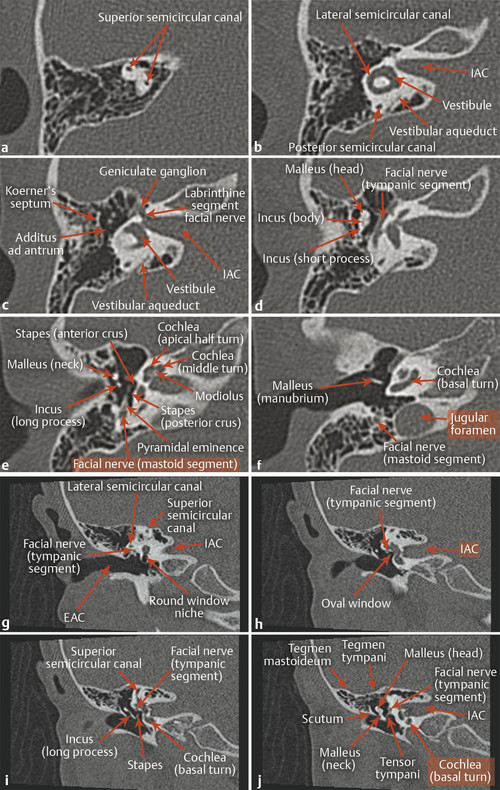
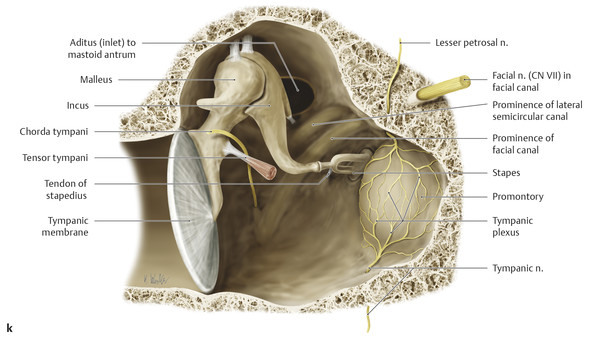
Within the middle ear are three ossicles: the malleus, incus, and stapes (Fig. 22.1d,e,f,i,j), which span from the tympanic membrane to the oval window. The structures of the inner ear include the cochlea, vestibule, and three semicircular canals (Fig. 22.1e,f). The cochlea has approximately from two-and-a-quarter to two-and-a-half turns, and at its center is a small osseous structure known as the modiolus, which contains the spiral ganglion, or ganglion for the cochlear nerve. The cochlear nerve passes through the cochlear aperture, traverses the internal auditory canal (IAC) and cerebellopontine angle cistern (CPA), and projects to the brainstem.
The IAC and CPA also contain the facial nerve and two vestibular nerves (Fig. 16.13b). The facial nerve travels between the cochlea and vestibule of the inner ear (labyrinthine segment), with nearly all of its fibers synapsing in the geniculate ganglion. The fibers then course along the superior aspect of the middle ear (tympanic segment) and descend between the middle ear and mastoid air cells (mastoid segment) before exiting the stylomastoid foramen.
The main portion of the middle ear cavity is the mesotympanum, above which is the epitympanum (Fig. 22.1b,c,h,i,j). The epitympanum communicates with the mastoid air cells through the aditus ad antrum, an opening bounded laterally by Koerner’s septum (Fig. 22.1c), and which communicates posteriorly with the mastoid antrum and air cells and anteriorly with the nasopharynx through the eustachian tube. The lateral aspect of the epitympanum contains a sub-area sometimes referred to as Prussak’s space, which is bounded laterally by the scutum (Fig. 22.1h,i,j).
22.3 Embryology Basics
The middle and external ear arise from the first and second branchial (pharyngeal) apparati. Accordingly, an abnormality in one of these areas has a high degree of association with abnormalities in these two parts of the ear. Thus, for instance, abnormalities of the external ear tend to be associated with ossicular malformation.
22.4 Hearing Loss
Hearing loss is one of the most common indications for dedicated temporal bone imaging in children. Hearing loss is characterized audiologically and otologically as being conductive, sensorineural, or mixed. Knowledge of the type and duration of hearing loss and side of the head on which it occurs is important, and for acquired hearing loss it is important to know whether the loss was abrupt or progressive and if there were associated symptoms, such as infection or cranial neuropathy. This information helps in determining the ideal modality for imaging the ear in a case of hearing loss, and whether to use intravenous contrast material in such imaging.
Conductive hearing loss is typically related to problems affecting the external auditory canal or middle ear, including the ossicular chain. Computed tomography is the gold standard for evaluating conductive hearing loss, with an estimated sensitivity for detecting a pathologic cause of such loss of approximately 90%. Accordingly, rescrutinization of images is warranted before concluding that a computed tomographic examination done for conductive hearing loss is normal. (n.b. this is for true, audiology confirmed conductive hearing loss. Conductive hearing loss identified by physical examination with a tuning fork will have a lower incidence of pathologic findings on CT).
22.4.1 Sensorineural Hearing Loss
Although adult-onset sensorineural hearing loss (SNHL) is best evaluated with contrast-enhanced MRI for seeking tumors like vestibular schwannoma, both CT and MRI can be effective techniques for evaluating congenital sensorineural hearing loss. Computed tomography can provide excellent bony detail about developmental abnormalities of the inner ear. Although CT has a high diagnostic yield for conductive hearing loss, both CT and MRI may be normal in patients with SNHL. This is the case in approximately 50% of cases, and pediatric SNHL is often idiopathic without an identifiable cause.
The labyrinthine structures can fail to develop completely, with effects ranging from complete labyrinthine aplasia (i.e., Michel aplasia) to incomplete partition of the middle and apical turns of the cochlea with an enlarged vestibular aqueduct (incomplete partition type II, originally described as the Mondini malformation) (Fig. 22.2). 1 ,? 2

The gradation between the most severe and milder forms of cochlear and vestibular dysplasia includes multiple additional abnormalities with characteristic features, which are described in s. Tab. and are covered in greater detail in dedicated articles on this topic. 3
Malformation | Gestational age of occurrence of developmental abnormality | Findings |
Labyrinthine aplasia (Michel deformity) | Third week | Agenesis of the cochlea, vestibule, and semicircular canals |
Cochlear aplasia | Third to fourth week | Agenesis of the cochlea. Vestibule present; semicircular canals likely to be dysplastic |
Common cavity deformity | Fourth week | Confluent cystic cavity, without separation or differentiation of structures, rather than normal cochlea and vestibule |
Cystic cochleovestibular anomaly (incomplete partition type I) | Fifth week | Cystic cochlea without modiolus or appreciable internal partitioning. Cystic vestibule without semicircular canals of normal appearance |
Cochlear hypoplasia | Sixth week | Cochlea and vestibule are distinctly formed but hypoplastic |
Incomplete partition type II (Mondini malformation) | Seventh week | There is a bulbous appearance of the middle and apical turns of the cochlea due to incomplete partitioning, resulting in 1.5 turns. Vestibular aqueduct typically enlarged. Vestibule and semicircular canals may be normal. |
Enlarged vestibular aqueduct | Unclear | Enlargement of the vestibular aqueduct in the absence of definable abnormality in the cochlea, vestibule, or semicircular canals |
The mildest abnormality seen, if any is present, is an enlarged vestibular aqueduct (Fig. 22.2), which is thought to transmit pressure from cerebrospinal fluid pulsations from the subarachnoid space into the inner ear. Accordingly, an enlarged vestibular aqueduct in a patient without hearing loss is felt to be a factor that increases the risk of eventual development of SNHL, which in turn is often instigated by a traumatic event. For this reason, an enlarged vestibular aqueduct is sometimes considered to be a contraindication to contact sports.
Some patients have absence or hypoplasia of the cochlear nerve. This will result in a narrow cochlear aperture (cochlear aperture stenosis), of typically less than 1mm diameter (Fig. 22.3). When this finding is made, MRI should be suggested, to permit differentiation between cochlear nerve aplasia and hypoplasia. A patient with cochlear nerve aplasia is typically not a candidate for an ipsilateral cochlear implant device.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree