Extrinsic Allergic Alveolitis
Pneumoconioses
Pneumothorax
Sarcoidosis
Adult Respiratory Distress Syndrome
BACKGROUND
Adult respiratory distress syndrome (ARDS) is a condition in which the pulmonary system is affected as a result of more generalized, multiorgan capillary damage. 14 The pathogenic sequence appears to be related to inappropriate activation of the complement cascade, 32,18 resulting in increased capillary permeability and pulmonary edema. Eventually fluid spills into the alveolar spaces, leading to hemorrhaging, reduced surfactant levels, and a resultant smaller functional area for gas exchange. A wide range of factors and conditions is associated with the development of ARDS (Box 26-1).
BOX 26-1
• Amniotic fluid embolism
• Arterial embolism
• Aspiration
• Drug abuse
• Eclampsia
• Fat embolism
• Fractures
• Heat stroke
• High-altitude pulmonary edema
• Pancreatitis
• Pulmonary contusions
• Radiation pneumonitis
• Shock
• Smoke inhalation
• Transplantation
IMAGING FINDINGS
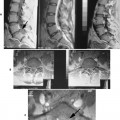
No changes are detectable radiographically during the initial stage of ARDS unless it is caused by pneumonia, aspiration, or another pulmonary condition, in which case the pulmonary findings of the concurrent disease may be noted. The latter stages of the disease are marked by alveolar filling. Patchy areas of incomplete lung consolidation are noted at first (Fig. 26-1), which eventually become more uniform, generalized, and homogenous. The radiographically detectable features gradually resolve during the ensuing weeks. Pleural effusion is rare.
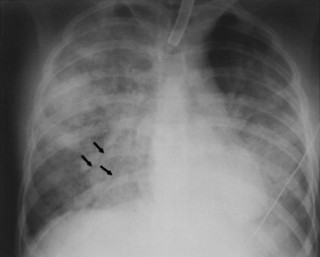 |
| FIG. 26-1 Diffuse pulmonary consolidations with air bronchograms (arrows) are the result of adult respiratory distress syndrome after viral pneumonia. This appearance is radiologically indistinguishable from pulmonary alveolar edema and diffuse pneumonia. (From Reed JC: Chest radiology: plain film patterns and differential diagnoses, ed 5, St Louis, 2003, Mosby.) |
CLINICAL COMMENTS
ARDS is characterized by rapidly progressing respiratory distress. 2,12 Alveolar filling is followed by acute respiratory failure that necessitates mechanical ventilation and oxygen administration. The eventual clinical outcome depends heavily on whether the patient develops a nosocomial infection, hemorrhage, sepsis, lung barotrauma, or another major complication. 18
• Adult respiratory distress syndrome (ARDS) involves increased capillary permeability that is caused by a wide variety of systemic and pulmonary insults.
• The radiographic features are related to excessive fluid accumulation in the alveolar spaces and present as varying degrees of lung consolidation.
Extrinsic Allergic Alveolitis
BACKGROUND
Extrinsic allergic alveolitis (EAA), also known as hypersensitivity pneumonitis, is a nonatopic, nonasthmatic allergic lung disease. EAA manifests as an occupational lung disease caused by the inhalation of organic dusts, which produces granulomatous and interstitial lung changes. Several etiologic agents are listed in Table 26-1.
| Disease | Provocative agent |
|---|---|
| Bagassosis | Moldy sugar cane |
| Bird fancier’s lung | Avian excreta |
| Farmer’s lung | Moldy hay |
| Humidifier lung | Contamination from humidifying, heating, and air conditioning systems |
| Malt worker’s lung | Moldy malt |
| Maple bark stripper’s lung | Moldy maple bark |
| Mushroom worker’s lung | Mushroom spores |
| Sequoiosis | Redwood dust |
| Suberosis | Moldy cork dust |
IMAGING FINDINGS
The radiographic presentation of EAA is the same regardless of the type of organic dust inhaled, 43 but it varies according to the intensity of the exposure. 30 The early stages of EAA usually are characterized by reversible, multiple, small (1- to 3-mm), nodular radiodensities that are scattered bilaterally throughout the lung zones; although it is less common, the lung apices may be spared (Fig. 26-2). * Repeated exposures may result in a chronic interstitial (honeycomb) pattern3,42 with upper lobe predominance.
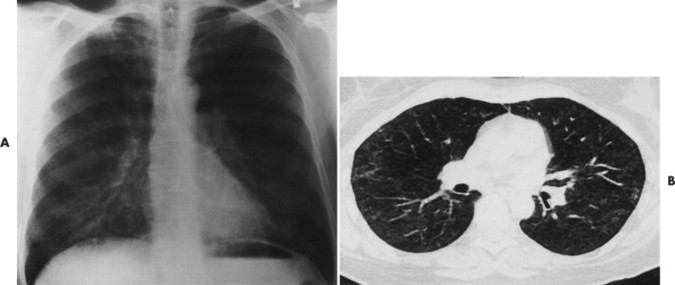 |
| FIG. 26-2 Extrinsic allergic alveolitis presenting with, A, bilateral diffuse infiltrate and, B, small pulmonary nodules on a computed tomogram after exposure to pigeon droppings. (From Swensen SJ: Radiology of thoracic diseases: a teaching file, St Louis, 1993, Mosby.) |
CLINICAL COMMENTS
Acute EAA is characterized by the sudden onset of malaise, chills, fever, cough, dyspnea, and nausea within hours after exposure to the offending agent. Subacute and chronic forms are characterized by a persistent cough and slowly progressing dyspnea, anorexia, and weight loss. The patient’s history of exposure preceding the clinical symptoms is important for a proper diagnosis.
• Extrinsic allergic alveolitis (EAA) comprises a group of diseases caused by the inhalation of organic dusts.
• The radiographic appearance is marked by the presence of small radiopaque nodules scattered throughout the lung fields.
• Chronic forms of the disease often develop a chronic interstitial pattern.
Pneumoconioses
BACKGROUND
Pneumoconioses are a group of diseases caused by inhalation of inorganic dust and its accumulation in the lung. 30 The dust deposits cause a nonneoplastic lung reaction that is often seen on radiographs. Asbestos, silicon, and coal dust incite a fibrogenic tissue reaction throughout the lung. Tin, barium, iron, and other inert particles do not incite fibrogenic changes but do cause particle-laden macrophages to accumulate in the lung. 4 These reactions are called benign pneumoconioses (even though their radiographic appearance can be dramatic) because they are less aggressive.
IMAGING FINDINGS
The chest radiograph is the primary means of determining the presence and extent of pneumoconiosis. 45 The International Labour Office (ILO) has established a classification system for the radiographic appearance of pneumoconioses20,39 that focuses on the size and shape of the lung nodules. The classification also includes a detailed categorization of pleural thickening.
The radiographic appearance of pneumoconiosis depends on the type and amount of dust inhaled and individual immunologic lung reactions (Table 26-2). 5,22 In general nonfibrogenic pneumoconioses show nodular opacities. A fibrogenic lung response is associated with lymphadenopathy; interstitial parenchymal patterns; and pleural thickening, calcification (FIG. 26-3FIG. 26-4 and FIG. 26-5), and effusion.
| Condition and causative agent | Comments |
|---|---|
| Nonfibrogenic (benign) | |
| Stannosis: tin | Stannosis is caused by deposits of tin in the lung that lead to formation of opaque nodules. |
| Baritosis: barium | Baritosis is caused by inhalation of barium sulfate, which produces small, rounded opacities that exceed the attenuation of calcium. |
| Siderosis: iron | Siderosis develops in workers who inhale fumes containing iron oxide particles, which produce scattered radiopacities in the lung fields. |
| Fibrogenic | |
| Asbestosis: asbestos | Construction workers, insulation workers, pipe fitters, ship builders, and asbestos miners may be exposed to asbestos fibers of varying levels of pathogenicity (e.g., crocidolite > amosite > anthophyllite > chrysotile), causing interstitial lung disease (asbestosis), pleural thickening (asbestos-related pleural disease), and malignancies. Asbestosis appears as linear radiopacities in the lung bases progressing to the apex. Asbestos-related pleural disease may be focal (plaques) or diffuse and usually appears in a posterolateral location. It is assumed to be the result of asbestos fibers that have pierced the visceral pleura. 29 Asbestos exposure increases the risk of developing mesothelioma1,7 and lung cancer. 6,23 |
| Silicosis: silicon dioxide | Silicosis results from exposure to silicon dioxide, 40 which is abundant in the earth’s crust and commonly encountered in mining, quarrying, sandblasting, and ceramic work. Small, radiopaque nodules are seen throughout the perihilar and apical regions. The nodules coalesce to form large (>2 cm) conglomerate masses that progressively migrate toward the hilum in a bilateral but asymmetric pattern known as progressive massive fibrosus (PMF). Occasionally hilar lymphadenopathy with possible peripheral “eggshell” calcifications of the hilar lymph nodes is present. |
| Coal worker’s pneumoconiosis (CWP): coal |