26 Tarlov’s Cyst
26.1 Introduction
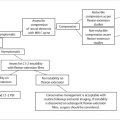
Tarlov’s cysts (TCs) are one of the most common incidental findings on MRI examinations of the spine. The vast majority of these cysts do not cause symptoms and will not need treatment. We review the imaging characteristics of TCs and discuss imaging features that allow their distinction from cystic tumors and other types of meningeal cysts of the spine. In the rare case in which the TC is determined to be symptomatic, treatment options and their risks and benefits are discussed.
26.2 Case Presentation
26.2.1 History and Physical Examination
A 45-year-old woman with a history of lower back pain and bilateral lower extreme (LE) numbness and tingling. Her past medical history was significant for obesity and diabetes.
There was patchy, nondermatomal decrease in sensation in her lower extremities bilaterally in a “stocking-type” distribution.
26.2.2 Imaging Analysis
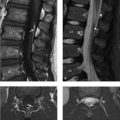
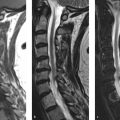
Parasagittal T1-weighted image (T1WI; ▶ Fig. 26.1a) and T2WI (▶ Fig. 26.1b) reveal a small, 1-cm cyst associated with the left S1 nerve root (arrowhead in ▶ Fig. 26.1a,b). There is a smaller cyst associated with the exiting left L3 nerve root (arrow in ▶ Fig. 26.1a,b). The cysts’ signal intensity is identical to cerebrospinal fluid (CSF) on both T1 W and T2WIs.

The axial T2WI reveals the left S1 neural foramen is smoothly expanded by the cyst (arrow in ▶ Fig. 26.1c).
The Tarlov cyst, or type II perineural cyst in the Nabors classification scheme, is a common incidental finding.
26.3 Clinical Evaluation
The vast majority of TCs are incidental findings. Even if there are radicular complaints, alternative explanations for the patient’s symptoms should be sought as these cysts are rarely symptomatic. In this case, the bilateral nature of the patient’s complaint, which was primary stocking-type sensory loss, was felt secondary to a peripheral neuropathy due to her diabetes. No further investigation or surgical intervention was warranted.
26.4 Differential Diagnosis
TC (Nabors’ type II spinal meningeal cyst):
Intraspinal cysts that are most commonly found in the lower lumbar, sacral, and coccygeal regions.
Nerve fibers are present within the wall of a TC and are intimately associated with a spinal nerve.
They are often located off the midline and may enlarge the neural foramen.
Juxta-articular, synovial facet joint cyst:
They arise from fluid-filled, hypertrophic facet joints.
They often have thickened walls and septations that may be dark on T2WIs due to synovial hypertrophy and/or prior hemorrhage.
Intrasacral meningocele (Nabors’ type Ib spinal meningeal cyst):
Intrasacral meningoceles are frequently midline. Although they may cause bony pressure remodeling, this is less commonly seen than with TCs.
Epidermoid:
Unlike spinal meningeal cysts, epidermoids will not precisely mimic CSF on all pulse sequences. Importantly, they cause restricted diffusion and therefore appear high in signal on diffusion-weighted images. Similar to spinal meningeal cysts, they will not enhance with gadolinium. Epidermoids are usually midline, within the thecal sac, near the level of the conus.
Cystic schwannoma:
Fluid contents do not precisely follow CSF on all sequences.
A solid, nodular, enhancing component is most often present.
26.5 Diagnostic Pearls
Although TCs have signal intensity similar to CSF on all pulse sequences, their signal intensity on T2WIs is often slightly higher than CSF due to lack of pulsatile flow that causes some normal dephasing of CSF signal within the thecal sac.
Original literature suggested that TCs would not fill with oil-based myelographic contrast. After water-soluble contrast media were used, they were shown to fill although often in a very delayed fashion. It is now known that both type I and II spinal meningeal cysts may fill with aqueous myelographic contrast media.
Cysts that do not fill readily with myelographic contrast may fill slowly via a “ball-valve mechanism.” These cysts may be more likely to become symptomatic and create pressure erosions of the sacrum and neural foramen.
26.6 Essential Information about Spinal Meningeal Cysts
The Nabors classification system of spinal meningeal cysts:
Type I: extradural meningeal cysts without spinal nerve root fibers:
Ia: extradural spinal arachnoid cyst.
Ib: sacral meningocele.
Type II: extradural meningeal cyst with spinal nerve root fibers (e.g., TC).
Type III: spinal intradural arachnoid cysts.
26.7 Companion Case
26.7.1 History and Physical Examination
A 35-year-old woman with a history of buttock pain.
The patient was neurologically normal.
26.7.2 Imaging Analysis
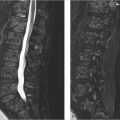
Initial images from a CT myelogram reveal a mass that is compressing the caudal most portion of the thecal sac, which does not fill with contrast (▶ Fig. 26.3a,b).
A midline sagittal reformation of the CT scan performed after the myelogram (▶ Fig. 26.3c) reveals that contrast did enter the sacral cyst although in a delayed fashion as is often the case.
These findings are consistent with large sacral TCs causing bony remodeling of the sacrum.


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree