33 Incidental Solitary Sclerotic Bone Lesion
33.1 Introduction
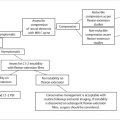
Detection of a solitary sclerotic bone lesion on CT or plain radiograph often creates a diagnostic dilemma. In this chapter, we will discuss key imaging features that strongly indicate the lesion is benign and those that warn further evaluation is warranted. The differential diagnosis of bone lesions that result in bony sclerosis will be given. Finally, we conclude with a case of an incidentally presenting sclerotic vertebral body lesion.
33.2 Case Presentation
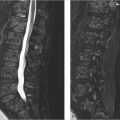
A 30-year-old woman underwent a CT of the pelvis for endometriosis and an incidental lesion was found in the sacrum. Therefore, MRI and bone scan were performed. Physical examination and past medical history were normal and noncontributory respectively.
33.3 Imaging Analysis
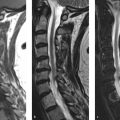
MRI of the sacrum: axial T1-weighted (T1w; ▶ Fig. 33.1a) and sagittal short tau inversion recovery (STIR; ▶ Fig. 33.1b), CT scan axial images (c), and bone scintigraphy (d). A T1w/T2-weighted (T2w) hypointense nonexpansile lesion is seen involving the sacrum (asterisk). Density measurements on CT scan revealed greater than 1,000 HU throughout the lesion. The lesion shows increased uptake of the tracer in the bone scan (arrow in ▶ Fig. 33.1d). This solitary, uniformly high-density lesion with neither edema in the surrounding bone marrow nor extension into the surrounding soft tissue most likely represents a giant bone island. Increased uptake on bone scan has been reported in bone islands, especially giant ones, but warrants imaging follow-up.

33.4 Clinical Evaluation and Management
In this case, because of the increased uptake on bone scintigraphy, a follow-up MRI was recommended at 6 and 12 months. Even though plain X-ray and CT would typically be used to follow a suspected bone island, MRI was chosen as the follow-up modality because the sacrum is an area not well seen on plain films due to overlying bowel gas and concern regarding radiation dose from multiple CT scans to the pelvis of a 30-year-old woman.
At the 1-year follow-up, the lesion was completely stable and no additional follow-up was recommended in the absence of symptoms.
33.5 Imaging Differential Diagnosis
Bone island:
Incidentally discovered, benign lesions also called enostoses, which are islands of cortical bone located in the cancellous bone.
Hyperdense oval-shaped lesions with spiculated or “paintbrush” margins, without distortion of the adjacent bony trabeculae.
A “cold” bone scan is helpful in distinguishing the bone island from a sclerotic metastasis, whereas a warm bone scan is nondiagnostic. (see diagnostic imaging pearls)
Osteoblastic metastatic disease (see ▶ Table 33.1):
More often multiple with increased uptake on bone scan.
Halo of increased signal on T2 W images about the low signal central lesion is suggestive of metastatic disease.
Less dense on CT and more heterogeneous than bone islands.
Sclerosing variant of osteosarcoma:
More heterogenous and irregular with bony trabecular destruction and possible extension beyond the confines of the cortex.
Edema often present in the surrounding bone marrow.
Osteoid osteoma:
Lucent nidus is present.
It favors posterior elements.
It classically presents with nocturnal pain in young patients, painful scoliosis, and marked relief from NSAIDs (nonsteroidal anti-inflammatory drugs).
Fibrous dysplasia:
Less dense than a bone island.
Classic ground glass appearance of the bone.
Prostate cancer (most common) |
Breast cancer (usually mixed lytic/sclerotic) |
Transitional cell carcinoma |
Carcinoid |
Medulloblastoma |
Neuroblastoma |
Colon, gastric cancer |
Lymphoma |
Treated lytic lesions |
33.6 Distinguishing a Bone Island from a Solitary Sclerotic Metastasis: Diagnostic Imaging Pearls
Bone islands do not have edema in the adjacent bone marrow or extension into surrounding soft tissue or adjacent bony destruction. 1
The classic bone island has a spiculated or paintbrush border and is much denser on CT than a osteoblastic metastasis. One study, using a mean attenuation of 885 HU and a maximum attenuation of 1,060 HU as cut-off values, distinguished the higher density bone islands from lower density osteoblastic metastases with 95% sensitivity and 96% specificity. 2
The primary utility of the bone scan is that if there is no increased uptake, sclerotic metastatic disease is highly unlikely; therefore, the lesion can be considered most likely a bone island and follow-up radiographic imaging obtained. 3
Increased uptake on bone scan associated with a solitary sclerotic lesion is atypical and therefore more worrisome, but largely unhelpful as there are many reports of bone islands having increased Tc-99 m hydroxydiphosphonate (HDP) uptake. 4 , 5 , 6
The bone scan is also helpful to look for additional sites of increased uptake that may not have been imaged, such as multiple nontraumatic rib, calvarial, or long bone lesions, which would strongly suggest the diagnosis of metastatic disease.
In the cases in which the solitary sclerotic lesion has increased, uptake on bone scan, follow-up CT, or plain film imaging is recommended at 3-, 6-, and 12-month intervals. 5 Biopsy should be considered in atypical cases or in high-risk patients with primary malignancies associated with osteoblastic metastatic disease. 5
In the cases with no known primary malignancy that are being followed with serial imaging, if the lesion increases in diameter by greater than 25% at 6 months or less, or greater than 50% at 12 months, open biopsy has been recommended by Brien et al. 4
Although usually stable in size, bone islands may increase or decrease in size or disappear. Growth has been demonstrated well after skeletal maturity. 7
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree