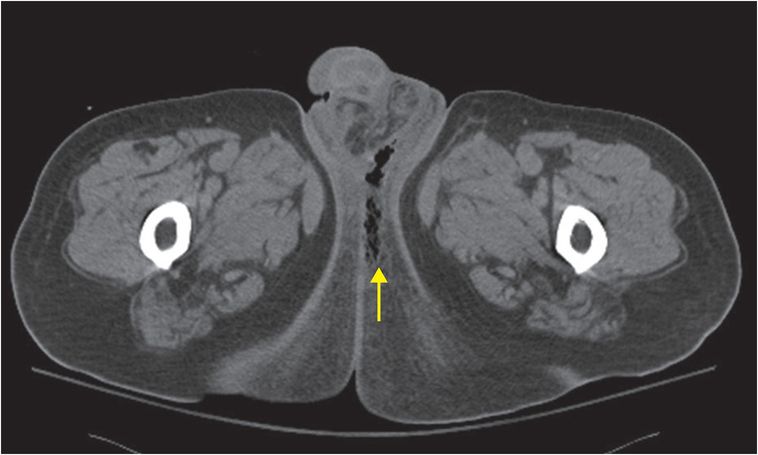
Diagnosis: Fournier gangrene
Contrast-enhanced axial CT demonstrates fat stranding and gas (arrow) extending to the perineum and left medial gluteal region via Colles’ fascia.
Discussion
Fournier gangrene has a high mortality rate and is considered a surgical emergency.
Patients may present with scrotal swelling, abdominal pain, pruritus, crepitus, and fever.
The most important predisposing factors include diabetes mellitus and alcohol abuse. Other risk factors include localized trauma, indwelling catheters, HIV infection, and radiation or chemotherapy.
Common causal organisms are aerobic bacteria such as E. coli and Streptococcal species, and anaerobes such as B. fragilis.
Treatment includes intravenous antibiotics and immediate surgical debridement.
Understanding perineal anatomy including the fascial planes is important in recognizing spread of infection.

The perineum is divided into the urogenital triangle (bordered by the ischial rami laterally and pubis anteriorly) and anal triangle (bordered by the coccyx posteriorly and sacrotuberous ligaments laterally).
Disease arising from the anal triangle may spread along Colles’ fascia into the ischiorectal fossa and then into the buttocks and thighs.
Disease may also spread anteriorly via the Dartos fascia to involve the scrotum and penis.
Although Fournier gangrene is often diagnosed clinically, imaging can play a key role in diagnosis and assessment of extent.
Radiographs may demonstrate subcutaneous gas before crepitus is evident on physical exam (though the absence of radiographically apparent gas does not exclude the diagnosis).
Ultrasound may show scrotal wall thickening with edema, dirty shadowing from subcutaneous gas, and reactive hydroceles.
CT findings include thickening of the fascial planes, fluid collections, abscesses, and subcutaneous gas; CT may help differentiate Fournier gangrene from cellulitis and soft-tissue edema.
Clinical synopsis
The patient was treated with IV antibiotics and underwent emergent surgical debridement.
Self-assessment
|
|
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








