As an initial imaging procedure, plain film radiography of the abdomen can be useful in evaluating serious and even life-threatening conditions. Even though it may not reveal abnormalities shown by diagnostic ultrasonography and computed tomography (CT), this imaging modality can be a cost-effective method for use in diagnosing and managing abdominal pathosis. The recognition of key diagnostic features (seen incidentally on spine radiographs or noted on abdomen views used in the initial investigation of abdominal complaints) on plain film can be critical to patient management.
LIMITATIONS
A caveat to keep in mind is that the diagnostic yield of plain film of the abdomen is low in the absence of signs and symptoms; therefore an abdomen radiograph usually is not recommended as a survey tool. Box 28-1 lists many conditions for which plain film radiographs are not indicated because roentgenographic findings rarely occur.
BOX 28-1
Appleton & Lange
Limitations of Abdominal Plain Film
Conditions in which diagnosis is rarely aided by abdominal plain films
Gastrointestinal bleeding
Hepatobiliary disease other than calcified gallstones
Acute cholecystitis, better diagnosed by ultrasonography or technetium-99m cholescintigraphy
Cholangitis
Acute hepatitis
Liver masses except when intrahepatic calcifications or hepatosplenomegaly is present
Acute pancreatitis
Ulcers
Inflammatory bowel diseases
Pyelonephritis
Modified from Baker SR, Kyunghee CC: The abdominal plain film with correlative imaging, ed 2, Stamford, CT, 1999, Appleton & Lange.
INDICATIONS
Common conditions for which abdominal plain films may be of value, especially if the patient presents with moderate to severe pain or if significant abdominal tenderness is present, are listed in Box 28-2. Other indications for plain film radiography of the abdomen include trauma, abdominal distention or pain, vomiting, diarrhea, and constipation (Box 28-3).
BOX 28-2
Appleton & Lange
Indications for Abdominal Plain Films
Conditions that may be diagnosed with plain film radiography
Perforated viscus
Intestinal obstruction
Adynamic ileus
Abdominal abscess
Bowel infarction
Fat versus ascitic fluid in obese patients
Emphysematous cholecystitis and colitis
Gallstone ileus
Urinary tract calculi
Abdominal aortic aneurysm
Preliminary films for contrast studies of urinary tract
Modified from Baker SR, Kyunghee CC: The abdominal plain film with correlative imaging, ed 2, Stamford, CT, 1999, Appleton & Lange.
BOX 28-3
Indications for Abdominal Films in the Adult Patient
Abdominal pain is moderate to severe
Abdominal pain is of any severity accompanied by significant abdominal tenderness
TECHNICAL CONSIDERATIONS
When clinically indicated, obtaining a single radiograph showing a recumbent anteroposterior (AP) view of the abdomen is the first step. Upright or decubitus views may add valuable information about gas and fluid patterns, free air, abnormal calcifications, masses, and abnormal organs. Oblique views may aid in further localizing abnormal findings. The entire abdomen should be visualized from the hemidiaphragms to the pubic symphysis. An upright, posteroanterior (PA) view of the chest may reveal valuable information about the presence of infiltrates in the lung bases, pleural fluid, or free peritoneal air that could explain the abdominal symptoms. Without the aid of contrast, abdominal contents generally are seen only if they contain gas or are surrounded by fat.
Before selecting the kilovolt peak (kVp), the patient’s size and clinical problem should be considered. Although a high peak kilovoltage is correlated with a low x-ray dose, the higher the peak kilovoltage, the less is the contrast. Often a peak kilovoltage of 80 to 90 kV is optimal, depending on what type of x-ray generator is being used (e.g., single phase, three-phase, high frequency). To minimize motion artifact, lower the exposure time and use a higher milliamperage (mA) setting.
Complete evaluation of abdominal pathosis usually requires additional imaging, which may include barium-filled bowel or intravenous contrast studies, ultrasonography, CT, magnetic resonance imaging (MRI), angiography, and nuclear medicine (Table 28-1). Some portions of the gastrointestinal (GI) tract can be visualized directly via fiberoptic scoping. Because the uterus is within the primary beam for abdominal imaging, pregnancy should be ruled out before conducting any imaging study that uses x-rays or radioactive material. Alternative imaging such as ultrasound should be considered if a patient is pregnant.
| Imaging modality | Technology | Advantages | Limitations |
|---|---|---|---|
| Ultrasound | Uses a combined transducer and receiver head to produce images based on the difference in tissue impedance or echogenicity to sound waves. | Noninvasive and has no notable risks or side effects; No ionizing radiation; Equipment purchase and maintenance is relatively low; Highly available; Examination time is relatively short; Capable of imaging most abdominal organs (except gas-filled bowel); Capable of identifying and measuring masses; Can determine the internal architecture of most masses (cystic, solid, complex); Can provide significant information about blood flow in masses or organs; Dynamic study allowing the investigator to pursue further questions that may arise as information is obtained. | Diagnostic ultrasound is highly operator dependent; Cannot image gas-filled bowel; Detail hampered in obese patients. |
| Computed tomography (CT) | Relies on contrast between radiographic densities as plain film does. It produces significantly greater resolution by using thin, fan-shaped beam and computer analysis to produce images of thin “slices” of anatomy. | Provides significantly greater detail than either plain film or ultrasound of the abdomen; Most organ architecture is well represented; Addition of contrast material to the vessels, renal collecting system, bowel, or other hollow structures provides better differentiation of those tissues from surrounding structures; Addition of intravenous contrast agents can provide information about the functional activity of masses and structures. | Uses ionizing radiation, so care must be taken to keep dosages down, especially in children; Availability may be an issue; Technology is reducing examination time, but time may still be somewhat prohibitive for seriously ill or uncooperative patients. |
| Magnetic resonance imaging (MRI) | MRI uses magnetic resonance technology to differentiate tissues by their cellular and extracellular contents. This provides important anatomic and functional information. The addition of intravenous contrast materials can provide further information about tissue metabolism. | Provides diagnostic information about solid, immobile organs such as the liver and kidney parenchyma. | Presence of gas in the bowel limits the usefulness of MRI in the abdomen; The mobility of abdominal contents also degrades MR images; Less available than CT. |
| Plain film with contrast | The use of barium- or iodine-based contrast agents greatly improves the value of radiography in evaluating the abdomen. Contrast agent is administered to fill a hollow structure such as the gastrointestinal (GI) tract (e.g., barium swallow, upper GI with small bowel follow-through, barium enema); the collecting system of the kidneys (intravenous pyelogram, retrograde pyelogram); the uterine body and fallopian tubes (hysterosalpingogram). Video fluoroscopy may be used to allow more complete and specific evaluation. | Lumen of structures can be evaluated for filling defects, mass effects, and irregularity of the lumen wall such as ulceration; Timed studies using contrast agents can give functional information regarding the motility of the bowel, contractibility, distensibility, and the ability of the kidney to concentrate urine. | Three-dimensional information is not available as it is with CT; Limited detail is provided regarding filling defects, mass effects, and constrictions. |
| Fiber optic exams | Fiber optics may be used to directly evaluate the lumen of accessible areas of the GI tract such as the esophagus, stomach, and colon, as well as the bladder and uterine cavity. | Direct visualization provides information about the lumen of hollow structures such as filling defects, constrictions, and mass effects; Direct observation also can detail subtle changes in the tissue lining the lumen that may not be available through other indirect studies. | Wireless endoscopy (a swallowable camera with transmitter) is still in the early stages of introduction to the field of diagnostic imaging. |
OTHER CLINICAL CONSIDERATIONS
When evaluating patients with musculoskeletal pain, it is imperative that the clinician be aware that many organ diseases refer pain. The more common sites of pain referral are listed in Table 28-2.
| Diseased organ or disease process | Site of pain referral |
|---|---|
| Aorta | Lumbar spine |
| Colon | Midlumbar spine |
| Gallbladder | Inferior scapula, interscapular, right shoulder |
| Gynecologic disorders | Lumbar spine; rarely above L4, pelvis |
| Kidneys, ureters | Groin, flank |
| Pancreas | Lower thoracic spine |
| Peptic ulcer | Midthoracic spine, heart area |
| Rectum | Sacral region Left lumbar paraspinal region |
| Sigmoid colon | Sacral region |
Plain Film Anatomy
GENERAL
Interpretation of abdominal radiographs is aided by knowledge of basic anatomic relationships. The location and relative mobility of abdominal organs are important factors in the evaluation of radiographic signs (Fig. 28-1). Whether a viscus is solid or hollow also can be important. Gas in the stomach, portions of the small bowel, and most of the colon and rectum usually makes identification of these structures possible. Fat surrounding the renal capsules, along the psoas muscle edges, and abutting the inferior aspect of the liver aids in their visualization.
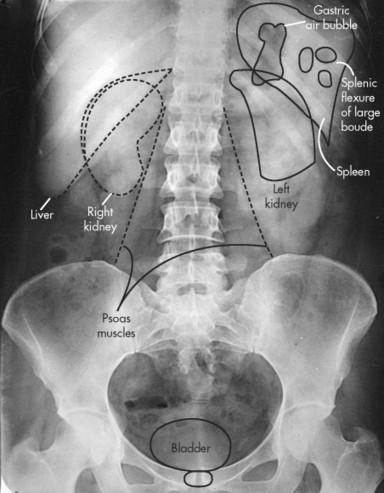 |
| FIG. 28-1 Normal radiographic anatomy of the abdomen. (From Ballinger PW: Merrill’s atlas of radiographic positioning and radiologic procedures, vol 2, ed 8, St Louis, 1995, Mosby.) |
Retroperitoneal structures are relatively fixed in position, which increases their potential for traumatic injury, among other factors. Consistently retroperitoneal structures include the kidneys and adrenal glands, third portion of the duodenum, ascending and descending portions of the colon, psoas muscles, pancreas, and abdominal aorta. Fascial planes provide channels for the spread of fluids, cells, and pathogens. Processes affecting the psoas muscle may follow the fascial sheath as far as the lesser trochanter of the femur.
Intraperitoneal structures can be categorized by their location within conceptual quadrants of the abdomen. The liver location is fixed in the right upper quadrant (RUQ). The liver shadow generally is well outlined inferiorly by intraperitoneal fat. Basic guidelines indicate that the liver should have a homogenous density and should not extend below the level of the iliac crest (although some normal anatomic variants do this) or past the midline. The lower liver margin may be delineated by gas in the adjacent small and large bowel. Although the gallbladder almost always is in the RUQ, closely opposed to the anteroinferior aspect of the liver, it is mobile in some patients and may be found in any quadrant. Much of the ascending colon is found in the RUQ. The transverse colon is mobile and its position may vary greatly, from running crosswise in the upper abdomen to dipping well into the pelvic area.
STOMACH
Most of the stomach is located in the left upper quadrant (LUQ), although its distal part does cross the midline into the RUQ and may extend ptotically into the lower abdomen. The stomach is identified on plain film by the gas it contains, especially the magenblase (stomach bubble) seen superiorly in the fundus on upright views (although gas may be seen throughout the stomach on supine views). The stomach is relatively fixed proximally at the gastroesophageal junction, with the remainder of the stomach being relatively mobile. A spatial relationship of the stomach with the transverse colon exists from attachment of the gastrocolic ligament. If distention or displacement affects one, the other’s position is affected as well.
SMALL BOWEL
The duodenum is primarily a fixed retroperitoneal structure, making it more vulnerable to injury in cases of blunt abdominal trauma. Although the duodenal bulb frequently contains some air, contrast material such as barium generally is necessary to visualize the duodenum adequately. The descending, or second, portion of the duodenum is associated closely with the head of the pancreas and is the emptying site of the pancreatic and common bile ducts. Processes affecting these structures may be identified by secondary changes involving the duodenum.
The jejunum often does not contain enough gas to serve any diagnostic purpose for plain film radiography and requires contrast material for optimal visualization. Mucosal folds tend to be fine and “feathery.” This portion of the small bowel is mobile; its mesenteric attachment to the posterior abdominal wall may serve as an axis for torsion.
The ileum also has the potential to be mobile, except when it is obstructed, involved with infiltrating diseases, or paralyzed. Like other portions of the small bowel, the ileum usually contains too little gas to be used for diagnostic purposes on plain film radiography except when obstructed or paralyzed. Differentiation between the jejunum and ileum can be difficult. The distal end of the ileum is connected to the colon at the ileocecal junction. Several diseases, including Crohn’s disease and tuberculosis, tend to develop in this region.