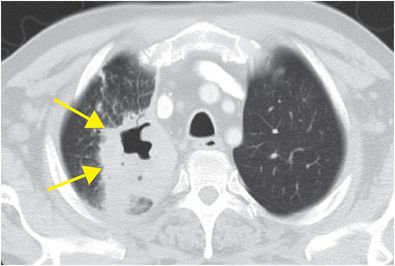
Diagnosis: Lung abscess
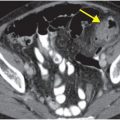
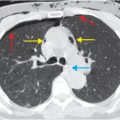
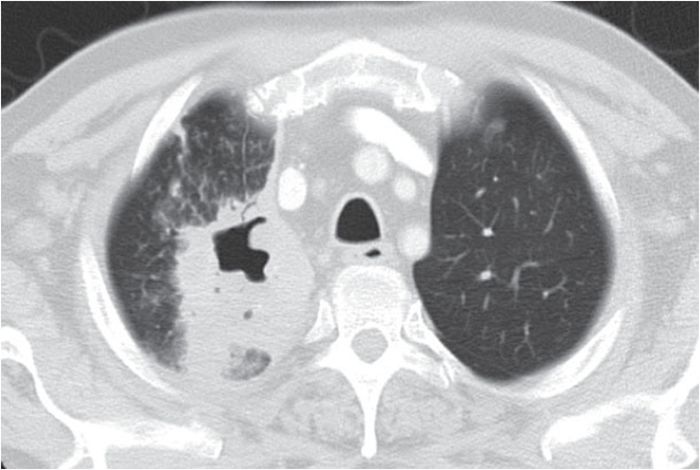
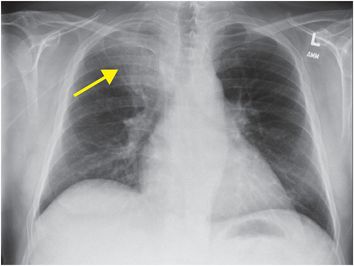
PA chest radiograph shows a consolidative opacity in the right upper lobe (arrow). Axial enhanced CT scan obtained 7 days later shows a right upper lobe consolidative opacity (arrows) with central cavitation, consistent with lung abscess.
Discussion
Lung parenchymal abscess is defined by central necrosis and diameter greater than 2 cm.
Abscesses most commonly result from aspiration or necrotizing pneumonia, and less commonly complicate infarcts or contusions.
In aspiration, causative organisms include mixed anaerobic and aerobic gingival flora (e.g., Bacteroides, Fusobacterium, Klebsiella, Staphylococcus, Pseudomonas). Fungi (e.g., Aspergillus, Candida) and parasites (e.g., Entamoeba) are also sometimes implicated.
Symptoms often have a subacute onset over weeks.
Typical, nonspecific signs and symptoms include fever, production of foul-smelling sputum, leukocytosis, and hemoptysis.
Elderly patients and others at risk for aspiration are more vulnerable. 70 to 80 percent of affected patients are smokers.
Immunocompromised patients are at greater risk.
Prognosis is poor without early diagnosis and treatment.
Image-guided aspiration is avoided for lesions >4 cm in the acute phase because of risk of spillover of infected contents into normal lung.
Treatment with antibiotics for an extended period is required; drainage is seldom needed, in contradistinction to abscesses in other organ systems.
Interventions are generally reserved for non-resolving abscesses or when the abscess abuts the chest wall.
The typical imaging appearance is a thick-walled cavitary lesion with surrounding consolidation, containing debris or gas–fluid levels. Abscesses are more common in dependent portions of the lung.
Chest radiography is the modality of choice for initial evaluation of any patient with a clinical presentation concerning for pulmonary infection.
Additional uses of chest x-ray in the management of pulmonary abscess include:
Monitoring of response to therapy
Detection of important complications such as pneumothorax, empyema, bronchopleural fistula, and pulmonary hemorrhage
Identification of additional or alternative diagnoses
CT may be needed for further diagnostic clarification in some cases, and to guide therapeutic interventions.
Abscess may sometimes be difficult to distinguish from empyema on chest x-ray or CT. Imaging findings that distinguish abscess from empyema are summarized in the following table:
| Abscess | Empyema |
|---|---|
| Intermediately thickened (4–15 mm) walls | Thin walls |
| Spherical | Lenticular |
| Surrounded by consolidation | “Split pleura” sign (CT) |
| Equal-length air-fluid levels on frontal and lateral radiographs | Different-length air fluid levels on frontal and lateral radiographs |
| Narrow interface with chest wall (CT) | Broad contact with chest wall |
| Bronchovascular markings extend to abscess | Adjacent compressed lung |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree