Diagnosis: Splenic infarction
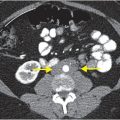
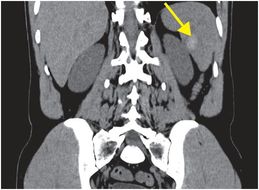
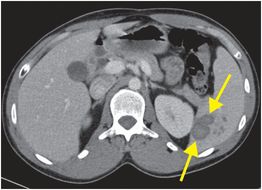
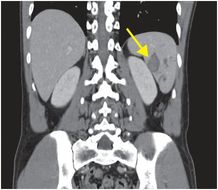
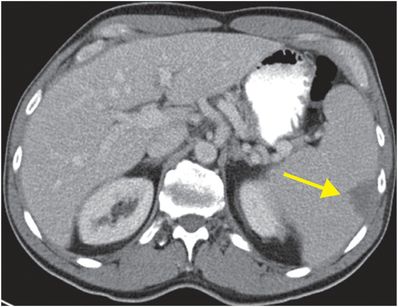
Initial unenhanced coronal CT (left image) demonstrates a hyperdense lesion (arrow) in the medial spleen, consistent with hemorrhage. Subsequent contrast-enhanced axial (middle image) and coronal (right image) CT images demonstrate a corresponding peripheral, slightly lobular, wedge-shaped, hypoenhancing region (arrows). Multiple smaller, round, hypoenhancing areas are seen adjacent. The splenic capsule remains smooth in contour. Taken together, these findings indicate acute, hemorrhagic splenic infarction.
Discussion
Splenic pathology is often clinically unsuspected until diagnosed by imaging.
The spleen is a vascular organ that is best evaluated with intravenous contrast. Unlike most other solid organs, the normal spleen demonstrates heterogeneous enhancement in the arterial phase; thus, the portal venous or parenchymal phase of contrast is optimal for splenic imaging.
CT is sensitive for splenic infarction, and is the diagnostic modality of choice when splenic pathology is suspected. In one study, only 18% of 48 patients with CT-demonstrated splenic infarction had corroborating sonographic findings.
Splenic infarcts may be hemorrhagic because the spleen is inherently vascular.
Different types of splenic lesions may have similar CT appearances, so a detailed clinical history is essential to differentiate among them. Because patients with splenic infarction may have fever (27%) and leukocytosis (58%), it can be difficult to exclude superimposed infection. Multiplicity of infarcts suggests the possibility of an infectious etiology.
Splenic infarction should be considered in the differential diagnosis of both left upper quadrant and left flank pain.
80% of patients with splenic infarction present with either left upper quadrant or left flank pain.
70% of patients with splenic infarction have an identifiable predisposing factor. The most common of these is atrial fibrillation, found in about one quarter of patients with splenic infarct. Rapid enlargement of the spleen is another important risk factor for infarction, germane to patients with viral mononucleosis or hematologic disease. Less common causes include hypercoagulable states, hemoglobinopathies such as sickle cell disease, and splenic vein thrombosis secondary to pancreatitis.
Clinical synopsis
This 20-year-old man with a long history of intravenous drug abuse presented with left flank pain. He also had a history of nephrolithiasis, so an unenhanced CT was initially performed to evaluate for renal stones. The diagnosis of hemorrhagic splenic infarction was posited, and more definitely characterized following contrast administration on a subsequent study. Given the patient’s history of IV drug abuse, a biopsy was performed and cultures were sent for microbiology. There was no growth and the patient was managed conservatively.
Self-assessment
|
|
|
|
|
|
Spectrum of splenic infarction
Non-hemorrhagic splenic infarct
The index case demonstrated a hemorrhagic splenic infarct, but splenic infarction may also present without internal hemorrhage. Axial enhanced CT demonstrates a classic wedge-shaped region of hypoattenuation of the peripheral spleen (arrow), consistent with a splenic infarction. No hyperattenuating focus is seen to suggest hemorrhage.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree