Diagnosis: Retroperitoneal hematoma
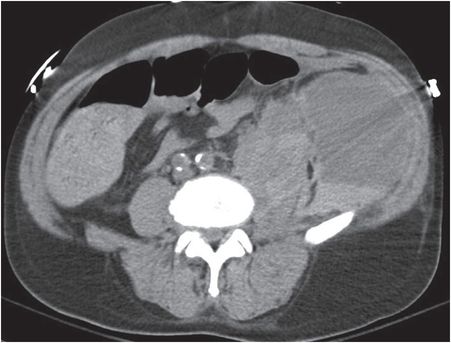
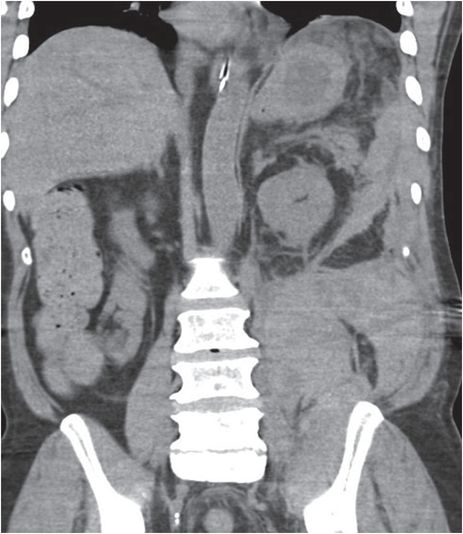
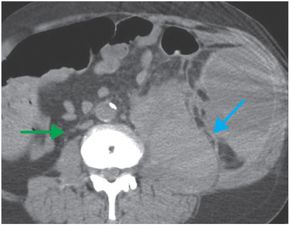
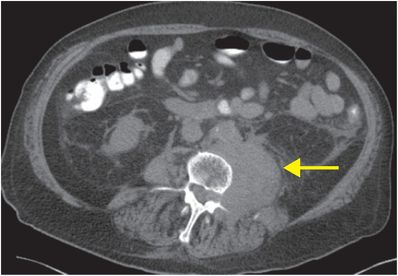
Axial (left and middle images) and coronal (right image) unenhanced CT images demonstrate a large fluid collection with a hematocrit level (yellow arrow). There is hyperdense blood tracking along the posterior pararenal space (red arrow) and into the left iliopsoas muscle (blue arrow). The IVC is flattened (green arrow), indicating hypovolemia.


Discussion
Overview of retroperitoneal hematoma (RPH)
A retroperitoneal hematoma (RPH) is a collection of blood in the retroperitoneum. It may be due to trauma, aortic pathology, or coagulopathy.
In particular, RPH is an important complication of anticoagulation therapy. The patient may present with acute anemia or dropping hematocrit, which may or may not be accompanied by pain.
Coagulopathy is often characterized by formation of a “hematocrit level” on CT, a term describing the separation of blood into lower-density serous and more dependent, higher-density cellular components.
Physical exam may be misleading since the retroperitoneum cannot be directly examined. Thus, imaging is critical to establishing the diagnosis.
Treatment for bleeding is managed with correction of any coagulopathy, intravenous fluids, and administration of blood products if necessary.
If RPH is contiguous with an abdominal aortic aneurysm (AAA), then the diagnosis of aortic rupture should be strongly considered.
Identifying aortic rupture as the cause of RPH is essential, since aortic rupture requires emergent surgery.
Most patients with atraumatic aortic rupture have an underlying AAA.
Contiguity of RPH with the aortic wall over a distance of >3 cm is both a sensitive and specific sign for ruptured AAA.
Identification of a site of active extravasation of IV contrast can help to differentiate ruptured AAA from RPH due to coagulopathy. In ruptured AAA, active extravasation is contiguous with the aorta, whereas in RPH, the site of active extravasation is typically noncontiguous. Unless the patient has a known AAA, however, CT for suspected RPH is generally performed without intravenous contrast.
Clinical synopsis
This patient was initially evaluated at an outside hospital, and given left thigh erythema and positive d-dimer, the diagnosis of deep vein thrombosis was presumed despite negative lower extremity ultrasound. Elevated creatine kinase and acute renal failure raised concern for rhabdomyolysis. He was treated with therapeutic doses of low molecular weight heparin (LMWH), after which he developed altered mental status and hypovolemic shock. Renal failure caused delayed drug clearance and prolonged effect of LMWH. The patient’s hematocrit dropped to 16%, but his condition improved with reversal of anticoagulation, aggressive fluid resuscitation, and transfusion.
Self-assessment
Spectrum of retroperitoneal hematoma
Psoas hematoma
The psoas (or iliopsoas) muscle is not an uncommon site for bleeding. Over time, secondary infection may occur, which may require percutaneous drainage. Axial CT with enteric contrast demonstrates expansion and hyperattenuation of the left psoas muscle (arrow) with haziness and stranding in the adjacent fat.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








