Cardiac catheterization can also be a relatively common cause of pneumothorax; its incidence after subclavian vein puncture is between 0.3% and 3%, but it almost never occurs after internal jugular puncture.
Air outside the alveolus may have little clinical significance or may be a potentially life-threatening situation requiring immediate intervention. One must recognize air outside the alveolus, decide which anatomic compartment it is in, and (it is hoped) determine its cause.
Air accumulates in the least dependent portion of the hemithorax.59 With the patient in the supine position, recognition of a pneumothorax is often difficult.60 Air collects in the anterior inferior aspect of the thorax adjacent to the diaphragm. This produces a deep sulcus sign, an abnormal lucency replacing the diaphragmatic sulcus with air over the upper quadrant of the abdomen (Fig. 5.2).61
Figure 5.2 A patient with respiratory failure and chronic obstructive pulmonary disease has developed right-sided chest pain. Note the classic appearance of a deep sulcus sign on the left.

Detection of a pneumothorax is generally simple; one simply looks for the thin line of the visceral pleura. Other findings, however, may mimic a pneumothorax. Lines and tubes projecting over the lung can be confused with the visceral pleural surface. Skinfolds are a common problem, mimicking a pleural line and suggesting a pneumothorax. A gradual increase in opacity up to the questionable pneumothorax line is quite characteristic of a skinfold, and often one can follow skinfolds outside the thorax, thereby excluding the diagnosis. Pulmonary vessels peripheral to the visceral line can ensure that you are not dealing with a pneumothorax.62
A small pneumothorax can be seen on an upright film and is often missed on a supine film. Whenever a pneumothorax is suspected, an upright expiratory chest x-ray should be obtained.63 Otherwise a cross-table lateral or decubitus view may be helpful. The decubitus view, with the side of interest being highest and nondependent, is perhaps the most helpful in detecting a small pneumothorax. This view may even be superior to the erect view because it permits a higher degree of contrast between the air collection, the hemidiaphragm, and the lateral aspect of the ribs. Here also, careful attention must be paid to entities that may mimic pneumothorax, such as skinfolds, bandages, and other artifacts. Of course if there is a doubt, CT is excellent in demonstrating a pneumothorax, especially in emergency conditions, but getting an ICU patient to the CT room is always a difficult undertaking.
The characteristic radiologic features of a pneumothorax include the presence of a thin, opaque linear structure, beyond which there is an absence of vascular markings. This structure is the visceral pleura bordered on one side by air in the lung and on the other side by the air in the pleural cavity.
Mechanical ventilation can produce adverse effects, generally due to the overinflation of the alveoli, subsequent rupture, and escape of air into the interstitial septa.64
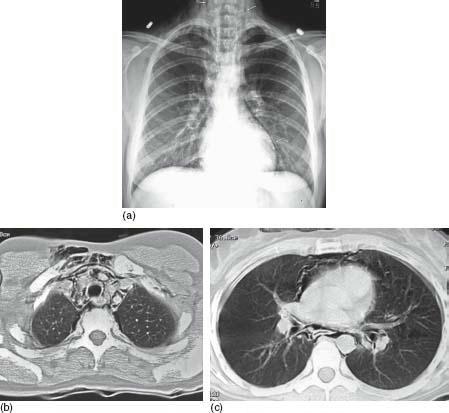
Most ventilator-induced barotrauma begins with interstitial pulmonary emphysema, which occurs when the intraalveolar pressure of the alveolus exceeds the pressure of the adjacent interstitium, permitting air to dissect into the interstitial tissues from the alveoli (Fig. 5.3).65 Radiologically, one can occasionally see radiolucent streaks radiating from the hila into the peripheral lung. It is extremely important to recognize extra-alveolar air, which can lead to either sudden or progressive respiratory and cardiovascular collapse. In mechanically ventilated patients, a simple pneumothorax can rapidly become a life-threatening tension pneumothorax.66
Figure 5.3 A The film of a patient with chest pain reveals air tracking along the mediastinum up into the neck and along the left cardiac border. This is the classic appearance of mediastinal emphysema. B A CT study of this patient’s neck reveals the classic appearance of interstitial and mediastinal air tracking up into the neck and then into the soft tissues, anteriorly of the neck. C Another CT study reveals the classic appearance of air dissecting back into the mediastinum and the interstitial tissues of the chest. A small pneumothorax is seen anteriorly in the least dependent portion of the chest.
PEEP also carries with it the possibility of severe adverse cardiopulmonary effects. There is often a reduction in cardiac blood flow due to PEEP or PPV, which is thought to be due to several factors, including an increase in intrathoracic pressure, which results in decreased venous return.67 Distention of the alveoli can also cause compression of the alveolar capillary wall, leading to an increase in pulmonary vascular resistance. Depending on peak expiratory pressure and the duration of its use, PPV can also cause pulmonary edema and damage to the lung itself.68
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree