Common Uses of Radiographs
Criteria for Ordering Radiographs
Image Interpretation
Report Writing
Summary
Sample Radiology Reports
Focus on Radiographs
Since its inception, diagnostic imaging has played a fundamental role in patient evaluation. Diagnostic imaging began more than 100 years previously with plain film radiography, and has progressing to advanced modalities, such as digital radiography, magnetic resonance imaging (MRI), computed tomography (CT), and positron emission tomography (PET). Diagnostic imaging remains an essential tool to recognize, define, identify, and exclude many of the common and not so common pathologies encountered in a health care setting.
For most clinical assessments, the historically dominant modality of plain film radiography continues to be the first step, with more sophisticated specialized imaging systems such as MRI and CT often applied as follow-ups to negative, equivocal, or ambiguous results of the plain film study, or for clinical questions for which plain films are known to be insensitive. Plain film radiology is widely available, relatively inexpensive, and rapidly obtained, predicting it will likely remain as the most common imaging method into the near future.
Plain film radiology represents a common denominator to many health professions. Dentists, podiatrists, chiropractors, medical physicians, and many practitioners in allied heath professions routinely rely on information obtained from plain film radiographs to manage their patients. With this in mind, the present chapter is focused on the interpretation and reporting of plain film radiographs. However, with little modification, the concepts presented here and targeted to plain film radiology equally relate to other more specialized imaging modalities. Therefore the goal of this chapter is to provide the reader with an understanding of issues related to when radiographs should be taken, methods to successfully search radiographs for abnormal findings, the ability to categorize these findings by appearance and location into common patterns, and steps to summarize and report on these findings successfully.
Common Uses of Radiographs
In 2000 an estimated $1.3 trillion was spent on personal health care in the United States. 36 Heath care expenditure was 13.1% of the gross domestic product in 2000, representing a per capita expenditure of $4377. 36 Of the most current data available, in 1990, an estimated 3.5% of these expenditures were for radiologic services, 139,140 much of it directed to nonradiologists.
Diagnostic imaging is common to clinical practice. More than 80% of chiropractors use radiographs as part of their clinical protocol and have the necessary equipment to produce radiographs in their offices. 4 Although national data are not available, a survey of Minnesota medical physicians found that approximately 87% had onsite radiology equipment. 61
Developing film interpretation skills is of obvious interest to radiologists, but developing these skills is also important to nonradiologist medical physicians, chiropractors, and other health care providers who often take and interpret radiographs as part of patient evaluation and management. For instance, most chiropractors do not regularly consult with radiologists to assist their interpretations. 63 In fact, fewer than 20% of hospitals have full-time onsite coverage by a board-certified radiologist. 101 During these off hours, the initial interpretation and related decisions are often done by nonradiologist clinicians, most to be overread by radiologists later. Moreover, of the radiologic services done in a private medical practice setting, 57%139,140 to 70%90,132 are performed and interpreted by nonradiologists.
Questions arise related to the appropriateness of training of nonradiologists to interpret imaging and under what circumstance it is best to consult with a radiologist. The American College of Radiology (ACR) recommends that radiographs be interpreted by certified radiologists or physicians who have documented training in an approved residency, including radiographic training on all body areas. This indicates the basic need for formal training, but does not limit interpretations to radiologists. 5 Literature within the chiropractic profession advocates for greater use of chiropractors who are certified with advanced training in radiology (Diplomates of the American College of Radiology [DACBR]) as a method of limiting liability and enhancing accuracy of image interpretation. 51
Taylor145 found that the degree of training positively influences the ability of medical and chiropractic clinicians and students to correctly identify selected bone and joint pathology. As one might expect, the concordance between the radiographic interpretation of radiologists and nonradiologists is best for extremity bone radiographs (approximately 95%) and lower for more complex studies, such as chest radiographs (generally ranging from 40% to 90%). *
Criteria for Ordering Radiographs
The most effective application of diagnostic imaging for many common clinical presentations is widely debated. The multifaceted and unique clinical presentations of most patients make the formation of common criteria for ordering diagnostic imaging problematic at best. Everyone agrees that all radiographic examinations should follow clear historical and clinical indications because of the examination costs and potentially hazardous effect of ionizing radiation. 96 Unfortunately, there is no general agreement on exactly what these historical and clinical indications should be to satisfy the competing needs of gaining information while limiting cost and radiation exposure.
To date, diverse opinions exist about what constitutes accepted clinical criteria for ordering radiographs for patients with musculoskeletal complaints. Although the literature documents many attempts to develop criteria for ordering radiographs for patients with complaints of the spine, † no system has been generally accepted. As a matter of observation, the use rates of plain film radiographs vary widely. Developing and embedding guidelines seem easier tasks for a narrow-scope presentation of something such as ankle112,134 or knee trauma, 135,136 but are less successful for case presentations of increasing complexity and ambiguity (e.g., back pain) and applied management (e.g., pharmaceuticals versus manual adjustments or manipulation of the spine).
Opinions vary widely about the use of radiographs in the evaluation of patients experiencing back pain. Multiple questions cloud the issue. Should radiographs be taken of patients who are experiencing acute but not chronic back pain? What are the appropriate film-ordering criteria that maximize clinical information yet minimize patient cost and radiation exposure?
Despite the fact that these topics have garnered considerable attention over the past decade, evidence-based guidelines for the use of plain film radiology (or CT and MRI) are not widely used in the clinical setting. 52 In 1987 the Quebec Task Force, and later the United States’ Agency for Health Care Policy and Research (AHCPR), developed guidelines for the use of plain film imaging related to patient presentation of acute low back pain. Similar efforts occurred in other countries. 27,36,122 The premise is that guidelines effectively influence practitioners’ use of plain films, as has been shown to occur in some instances. 42,78 However, guidelines prove less effective as the population and clinical problems become less homogeneous and more complex.
Factors affecting whether radiographs are taken include clinical data, patient expectations, and clinicians’ attempts to reassure patients or themselves. 91,104,157 Also the type of practitioner is very important: The use of radiographs for low back complaints varies from 2% to 48%, depending on the type of practitioner. 52 Chiropractors—who employ a manual approach to patient care—and orthopedic specialists demonstrate increased use of plain film radiographs compared with medical physicians in family practice who manage patients with acute low back pain. 32 This observation may result in part from a bias toward searching for a musculoskeletal derangement as the cause of the patient’s complaint; however, it probably also reflects varying therapeutic approaches to patients’ complaints and the need for structural information related to the delivery of care and patient management.
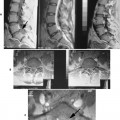
In chiropractic practice, radiographs generally are considered a standard first-step imaging protocol when evaluating degenerative and inflammatory joint disease, fractures, infections, and neoplasms. 57 The hands-on management approach of chiropractors warrants attention to biomechanical influences and potential structural contraindications to intended interventions (Fig. 5-1). Nonchiropractic clinicians, whose management of low back pain centers on exercise, patient education, pharmaceuticals, and other clinician-passive therapies, have less use for the biomechanical or structural information obtained from radiographs. Therefore these practitioners can easily adopt a more conservative approach to taking radiographs for musculoskeletal spine complaints than can chiropractors or other practitioners, who apply manual intervention.
 |
| FIG. 5-1 Three streams of information from the radiograph. In the context of delivering chiropractic care (or other manual approaches to patient care), radiographs provide three types of information: (a) information related to possible structural contraindications or cautions to delivering a corrective force into the demonstrated anatomy; (b) information that may influence the direction or technical approach to delivering a corrective force; and (c) information related to diseases, conditions, or findings that are seen in addition to the chiropractic subluxation, osteopathic lesion, or primary reasons the radiographs were taken. For instance, this radiograph demonstrates osteopenia that will influence the delivery of the chiropractic adjustment (stream A). There may be biomechanical or degenerative features that will cause the chiropractor to adjust one segment over another, thereby influencing the technical approach to the patient (stream B). Last, the compression fractures may result from an underlying aggressive pathology such as metastasis that would be of great concern to the clinician, beyond the issue related to the chiropractic subluxation or the initial concerns of the clinician (stream C). |
Many radiographs taken in a chiropractic setting are interpreted as normal for serious bone pathology, 82 but they may relate biomechanical or structural information that allows the chiropractor to be more successful with technical aspects of formulating and applying the patient’s management plan. However, more research into the reliability, validity, and clinical usefulness of biomechanical and structural information gleaned from radiographs is necessary. Also evidence is needed to clearly justify the added costs, define criteria of patient selection, and facilitate advancements in care delivery.
All clinicians, regardless of therapeutic approach, are concerned with serious pathology masking as routine low back pain. Clinical red flags that suggest the presence of serious pathology have been developed and are helpful to direct patient selection (Box 5-1). In the absence of these red flags, significant spinal pathology is estimated in only 1 of 2500 patients. 152 Deyo and Diehl43 evaluated 1975 walk-in patients at a public hospital to estimate the prevalence of cancer as an underlying cause of the patient’s back pain. Using a developed algorithm that generally reflects the questions listed in Box 5-1, only 22% of these patients would have received x-rays; this proportion includes all those who were later found to have cancer.
BOX 5-1
Clinical Red Flags of Serious Spinal Pathology (e.g., Infection, Tumor, or Fracture)
Unexplained weight loss
Personal history of cancer
Unexplained fever
Age more than 50 years
Intravenous drug use
Prolonged corticosteroid use
Severe, unremitting pain at night
Trauma sufficient to cause fracture or injury
Pain that worsens when the patient is lying down
Features of cauda equina syndrome
Urinary retention
Bilateral neurologic signs or symptoms
Saddle anesthesia
From Deyo RA, Diehl AK: Lumbar spine films in primary care: current use and effects of selective ordering criteria, J Gen Intern Med 1:20, 1986.
It should not be assumed that instituting guidelines, such as those listed in Box 5-1, will lead to less use. For example, Canadian researchers found that if the guidelines listed in Box 5-1 had been applied to their study population of 963 patients in a private medical family practice setting, 44% would have undergone radiography, increasing actual use by 238%. Considering patient follow-up, these researchers concluded that the sensitivity of the guidelines to detect fractures and tumors was higher than the physicians’ use patterns, but their specificity and positive predictive values were low. 138
Parallel and similarly controversial issues surround the application of specialized imaging. (e.g., whether MRI should be ordered for a patient in whom a disc herniation is clinically suspected yet neurologic findings are limited). This is especially true when the literature suggests that approximately 25% of normal adults demonstrate acquired spinal stenosis and 33% have a disc herniation, 44 two key MRI findings.
In the absence of clear guidelines, clinicians must adhere to a logical rule for the use of all diagnostic procedures: If the patient’s diagnosis or management is likely to significantly change from information routinely provided by the diagnostic procedure in question, then the study should be performed; if the necessary information is not routinely provided by the procedure or knowing the information obtained will not change the patient’s management, then the procedure should not be performed.
Image Interpretation
EQUIPMENT AND RESOURCES
Before the skills and knowledge of the interpreter can be brought to task, the images should be clearly displayed and reference material should be close at hand. This is a digital age, but clearly the revolution has not permeated all segments of the population evenly. Although many clinics have moved to filmless methods for acquiring and displaying images, not all are so advanced. Much radiology, particularly plain film, is still accomplished traditionally; this produces radiographs that should be viewed on illuminated light boxes. These view boxes generally are available in two sizes, the standard 14 × 17 inch view box, and a larger 14 × 36 inch view box that accommodates a full spine radiograph, the type often used to assess scoliosis. Standard 14 × 17 inch view boxes are combined in various configurations to create a viewing station (Fig. 5-2).
 |
| FIG. 5-2 View box station. View boxes are arranged in various formats to construct a viewing station. This picture exhibits a simple four over four bank on the right and a two over two bank to the left of it. |
High-volume centers may invest in a viewing system with rotating panels or belts that pass the films in front of a stationary bank of lights, because placing the films on and off the view box can consume a considerable amount of time. This system allows many cases to be stored and viewed quickly, without the need to shuffle through the films of each case as they are put on and off the view box.
A “hot” or “bright” light is another important tool necessary for film interpretation (Fig. 5-3). The hot light produces a controllable high-intensity beam of light that helps the interpreter view the overexposed (dark or radiolucent) areas of the film. The intensity of the light can be controlled with a pedal that allows the interpreter to match the brightness of the light to the darkness of the radiograph. Even radiographs that are executed under the highest technical standard have regions of overexposed anatomy. Some of the more common and significant pathologies often hide in the overexposed areas of the film, making it difficult to recognize them when viewing the films only on a view box. Therefore a hot light is an essential tool to a thorough film interpretation.
 |
| FIG. 5-3 Hot light. The hot light (also known as a bright light) is an essential tool to film interpretation. By using a hot light, the interpreter is able to view the overexposed regions of the film. Some of the most serious pathologies (e.g., lung nodules, aneurysms) are common to the overexposed regions of a radiograph and are more easily seen with the aid of a hot light. |
It has been said that “a radiologist with a ruler is a radiologist in trouble.”97 Although the sentiment underscores the importance of clinical intuition, observation, and training, the reality is that handy access to rulers, protractors, or other measuring devices allows more accurate quantification of structural abnormalities. For instance, the degree of spondylolisthesis is related to the likelihood of its further progression, the rate of growth of a pulmonary nodule is predictive of its malignant potential, the degree of scoliosis is central to the management of the case, and so on.
Reference texts should be close at hand. The usefulness of some radiology books transcend the typical, such as Keats’ Atlas of Normal Roentgen Variants That May Simulate Disease.76 A recent edition of Keats’ atlas should be close to the reading area. As the title describes, this book is a regional atlas of abnormal film findings that are normal variants of anatomy. This book is comprehensive and includes both subtle and grossly abnormal cases. Recognizing that an abnormal finding is a normal variant saves time and examination costs related to erroneous additional evaluation. For example, view the case exhibited in Figure 5-4 of a 12-year-old with a history of trauma. The calcaneus clearly looks fractured, but the radiolucent defect actually represents an unfused secondary growth at the center of the calcaneal tuberosity. A similar case is noted in the third edition of Keats’ book. 76 Recognizing that this is a normal variant and not a fracture ensures that time and expense are not wasted.
 |
| FIG. 5-4 Lateral ankle of a 12-year-old who recently suffered a trauma to the calcaneus. The radiolucent line appearing as a fracture (arrow) actually represents a normal appearance of the secondary growth centers. This case demonstrates how closely some normal findings and variants of normal may simulate a disease state. (Courtesy C. Robert Tatum, Davenport, IA.) |
ERRORS IN FILM INTERPRETATION
Interpreter error may arise from a failure to see, recognize, or understand the significance of a lesion. Although errors rates of 20% to 30% have been reported, 55 the more contemporary literature indicates that approximately 1% to 3% of plain film interpretations done by nonradiologists contain important errors. * Most of these studies are done by emergency department personnel.
Seltzer128 estimates that 8% of interpretations by medical radiology residents contain potentially clinically important errors, which suggests that misinterpretation is increased in interpreters with fewer qualifications. Complex studies (e.g., CT) 2 and studies on pediatric patients129 also increase misinterpretation. Fractures are the most often-missed lesions. 30,118,155 Training is associated with more accurate interpretation, 145 but radiologists are not immune to misinterpretations, as studied with various methods and imaging modalities.656667686993 and 116 Most studies focus on false-negative readings; however, false-positive readings occur among radiologists30 and nonradiologists153 alike. False-positives promote continued patient evaluation, adding to the cost, which is estimated to average $85 per false-positive reading. 153 Unnecessary examinations also result in increased risk of complications associated with imaging.
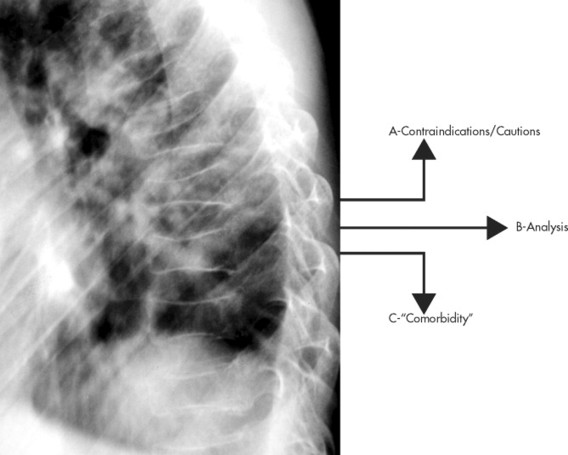
Alleged diagnostic errors account for the majority of legal cases related to radiology departments. 20 However, not every missed lesion constitutes evidence of negligence. Statistics pointing to related rates of missed lesions, limitations of normal human visual perception, image quality, and many other factors influence image interpretation, and may be mitigating factors for image misinterpretation.2021222324 and 130 The conceptual difference between errors in interpretation and those arising from perceptual variations is well described by Robinson. 117 The former assumes the diagnosis is known and generally agreed upon as a lesion; the latter does not (Fig. 5-5).
 |
| FIG. 5-5 Errors in image interpretation. This figure depicts a relationship between the imaging appearance of a lesion (size, shape, etc.) and the probability that the apparent lesion truly is one. (A) At times, their may be an uncertain or mixed interpretation of a grossly abnormal feature (e.g., importance of a lumbosacral transitional segmentation or spondylolisthesis). (B) Easy cases to interpret are defined as those that appear clearly abnormal on imaging and have a high degree of certainty that they are real lesions. Misinterpreting such a case is a clear error. (C) In contrast, difficult cases are those that present with only mild departures from the appearance of normal anatomy and are associated with doubtful conclusions on whether a true lesion is present. Misinterpreting this case may reflect a genuine difference of opinion among experts, representing variation in opinion more than direct error. (D) Last, only a small deviation from normal anatomy may correlates to a certain lesion. For example, a small corner fracture of the phalanx appears subtle, but has a certain interpretation as a lesion. The watershed of acceptable performance represents the line between clear-cut error and the inevitable difference in opinion existing between and among professionals. (From Robinson PJ: Radiology’s Achilles’ heel: error and variation in the interpretation of the Roentgen image, Br J Radiol 70:1085, 1997.) |
The goal of film interpretation is to eliminate as many misinterpretations as possible. There is a substantial literature addressing the topic of radiologic interpretation (see Table 5-1). The literature and conventional wisdom indicate that although it is impossible to eliminate human error, and therefore mistakes of radiologic interpretation, then attention to common principles should prove beneficial (Box 5-2).
| Topic | Article | Summary |
|---|---|---|
| Ambient light | Alter AJ et al3 | Employing low ambient room light, illuminating only films being viewed, and masking the radiograph around areas of interest improves visual performance; however, is cumbersome to implement completely in a clinical setting. |
| Appearance of the lesion | Krupinski EA et al85 | This study found that physical features of pulmonary nodules do not attract attention as measured by “first hit” fixation of the interpreter’s gaze; however, certain features do tend to hold the attention once the nodule has been fixated. The combination of all features influences whether or not it is detected. |
| Experience | Herman PG et al66 | After having several interpreters view a series of chest radiographs, the authors found that, “Once an individual’s radiology education has progressed beyond a fundamental level, individual reader characteristics overshadow experience (and training) in the accuracy of chest film interpretation.” |
| Experience | Nodine CF et al100 | Differences in resident performance resulted primarily from lack of perceptual-learning experience during mammography training, which limited object recognition skills and made it difficult to determine differences between malignant lesions, benign lesions, and normal image perturbations. A proposed solution is systematic mentor-guided training that links image perception to feedback about the reasons underlying decision making. |
| Experience | Qu G, Huda W, Belden CJ114 | Trained observers are superior to untrained observers when assessing characteristics of phantom images. |
| Experience | Krupinski EA, Weinstein RS, Rozek LS86 | There is a positive correlation between years of clinical experience and ability to successfully interpret radiographic images. |
| Experience | Nodine CF, Krupinski EA99 | Performance on two visual search and detection tasks indicate that radiologists do not possess superior visual skills compared with lay people. Radiology expertise is more likely to be a combination of specific visual and cognitive skills derived from medical training and experience in detecting and determining the diagnostic importance of radiographic findings. |
| Experience | Rhea JT, Potsaid MS, DeLuca SA116 | Experienced interpreters exhibited lower rates of false-positive and false-negative readings. |
| Experience | Sowden PT, Rose D, Davies IR131 | Performance of a wide range of simple visual tasks improves with practice. This learning may be a specific function of the eye. |
| Experience | Taylor JAM et al145 | This study demonstrated a significant association between the interpreters (both medical and chiropractic) training and their ability to recognize abnormal radiographs of the lumbosacral spine and pelvis. |
| Eye dwell time and axis of gaze | Carmody DP, Nodine CF, Kundel HL34 | “Our findings indicate that a dwell time of 300 ms was sufficient to detect 85% of the nodules when they were viewed directly. Detection accuracy was reduced by one-half when the tumor was located 5 degrees from the axis of gaze.” |
| Eye gaze durations, scan paths, and detection times | Krupinski EA84 | Readers with more experience tended to detect lesions earlier in the search than did readers with less experience, but those with less experience tended to spend more time overall searching the images and cover more image area than did those with more experience. |
| Confidence level | Mayhue FE et al94 | Prospective interpretations of nearly 1900 emergency room radiographs were performed by multiple interpreters. The concordance of agreement varied by level of confidence, but not training level among the interpreters. |
| Influence of patient history | Berbaum KS et al15 | This study tested whether accompanying patient clinical information would improve perception or simply decision making. The report found that the interpreter’s detection of pathology was significantly better with history provided before film inspection. Detection did not differ for history provided after inspection and inspection without history. The authors concluded, “clinical history affected perception in interpreting radiographs, not simply decision making.” |
| Influence of patient history | Berbaum KS, Franken EA, el-Khoury GY17 | A brief patient history may provide localization clues that improve the ability of interpreters to detect fractures and other features of trauma. When localization clues are withheld or unavailable, radiologists and nonradiologists alike are less successful in finding trauma lesions; although the accuracy of the radiologists suffers less. |
| Influence of patient history | Good BC et al56 | Researchers found that knowledge of clinical history does not affect the accuracy of radiologists’interpretations of chest films for the detection of pathologies such as interstitial disease, nodules, and pneumothoraces. |
| Miss rates | Robinson PJ117 | This is a literature review of strategies for reducing error in radiograph interpretation. Methods include: attention to viewing conditions, training of observers, availability of previous films and relevant clinical data, dual or multiple reporting, standardization of terminology and report format, and assistance from computers. |
| Miss rates | Herman PG et al65 | These authors found that 41% of chest radiograph reports contained potentially significant errors and 56% showed indeterminate disagreement. In addition, 78% of all errors were false-negatives and 22% were false-positives. |
| Perception of the image | Kundel HL, Nodine CF89 | These authors advocate that image perception begins with characterization of the scene integrating data from the retina and memory to form a visual concept. This theory holds that it may be necessary to have seen radiologic abnormalities in the past to be able to form an appropriate visual concept for a current abnormality. |
| Prior studies | Berbaum KS, Smith WL18 | “Old reports add value to current interpretation by providing a form of ‘second reading’ and providing clinical history. Two years is sufficient old report access in 85% of situations.” |
| Satisfaction of search errors | Berbaum KS et al16 | This defines the satisfaction of search phenomenon in diagnostic radiology and the development of statistical methods to measure observer performance. |
| Satisfaction of search errors | Ashman CJ, Yu JS, Wolfman D7 | The satisfaction of search phenomena describes a situation in which the detection of one radiographic abnormality interferes with the detection of others. Satisfaction of search defects of film interpretation is operative in the interpretation of radiographs of the musculoskeletal system. |
| Satisfaction of search errors | Berbaum KS et al14 | It appears that satisfaction of search errors originate from recognition failures more than poor decision making. |
| Satisfaction of search errors | Berbaum KS et al13 | An appropriate history appears to reduce satisfaction of search errors. It is believed that detailed histories direct the interpreter’s perceptual resources to the prompted abnormalities, reducing the satisfaction of search error. |
| Search path | Kundel HL, Nodine CF88 | This experiment quickly flashed the image as a means of negating the ability for observers to visually scan the image, resulting in an overall true-positive rate of 70%. As anticipated, the rate improved to 97% with the addition of a free search of the images. These data support the fact that visual search begins with a global response of the interpreter to the image to establish content and detect gross deviations from normal. |
| Search path | Beard DV et al10 | Radiologists’film interpretation has a typical sequence. Films are mounted in order; radiologists generally start a sequential scan through the entire examination; this is followed by a detailed viewing of two to four clusters of three to six images; and last the findings are dictated or otherwise recorded. |
| Search path | Hu CH et al74 | More systematic scanning patterns were observed for experienced than inexperienced observers. |
| Search path | Carmody DP, Kundel HL, Toto LC33 | Although radiologists are formally trained to search radiographs using a systematic and directive search path with comparison of bilateral features, only 4% of visual activity was accomplished with bilateral comparison when observed. Most radiologists used a flexible search path. |
| Search path | Swensson RG, Hessel SJ, Herman PG143 | Data collected on readings of chest radiographs found that “radiologists could distinguish between normal and abnormal radiographs better when searching the chest films for any abnormal findings than when explicitly evaluating” the radiographs for specific features to which their attention is directed. The authors theorize that “the recognition of abnormal findings may have been augmented by perceptual mechanisms that functioned only during the process of visual search.” |
| Search path | Peterson C107 | The authors found that chiropractic students who employed a flexible but complete search pattern when interpreting radiographs performed significantly better than their peers using any other search pattern approach. |
| Second opinions | Swensson RG, Theodore GH142 | This study involved multiple interpretations of chest radiographs and found that second opinions are more accurate if the second interpreter is not aware of the concerns or findings of the first interpreter. |
BOX 5-2
Suggestions to Reduce Radiologic Interpretation Errors
1. Become familiar with the patient data. The age, gender, and ethnicity of the patient may offer potent predictors of what disease process is represented on the radiographs. For instance, a 2-cm solitary radiodense defect of the L4 vertebral body is likely a bone island in a patient under 30 years of age. By contrast, a metastatic deposit needs to be excluded in a patient more than 40 years of age. Patient demographics directly influence clinical decision making.
2. Become familiar with the clinical context of the study. The clinical rationale for the study should be known before a patient’s images are viewed. The interpreter should have a good idea of what he or she will encounter before the films come out of the processor. For example, are the films done to evaluate the patient for a clinically suspected rib fracture? Knowing the clinical context is essential to a thorough interpretation.
3. Assess technical factors, image quality, and artifacts. The images should be of sufficient quality and the correct area of clinical interest. Film interpretation is directly and negatively influenced by poor technical factors, such as improper patient positioning, patient motion, and many others problems that are more fully discussed in Chapter 1. Faint shadows of pathology may not be visible if the images are underexposed or overexposed. Patient motion is probably the most common technical defect that degrades image interpretation. Also, all of the clinically relevant anatomy must be visible to the degree expected. Images taken when the patient is recumbent may cause some of the anatomy to appear quite different. A case in point is the difference in size of the heart shadow on recumbent and upright films, or inspiration versus expiration patient instructions on upright films. Clothing and other artifacts can form ambiguous presentations on radiographs.
4. Search the images using an intentional, thorough visual path. Image interpretation has a greater chance of being successful if steps are taken to view the entire image in a complete manner. One popular approach to film interpretation involves a review of the alignments (A) of structures, bone (B) elements, cartilage (C) or joint spaces, and soft tissues (S). This is known as the “ABCS” approach to film interpretation and the method ensures that all of the anatomy is viewed completely. However, the interpreter should not be a slave to the ABCS sequence of film interpretation. For some, the ABCS approach may be more naturally applied as a BCAS or CABS sequence. The important point is that all of the anatomy is viewed; the order is less critical.
When an abnormal finding is discovered, a free search path is invoked to follow the features of the disease. Once all of the related findings have been observed, the interpreter returns to a fixed sequence to ensure that all of the anatomy has been viewed. The search path never should be haphazard. It needs to intentionally follow the predetermined path of the anatomy (e.g., alignments, bone, cartilage, soft tissue) or trail of pathologic findings (e.g., observed fracture line, associated angulation, soft-tissue distension).
5. Patients are entitled to more than one problem. As mentioned, the radiographs should be searched completely for defects in the alignment, bones, cartilage joint spaces, and soft tissues. It is especially important to be vigilant to a complete search pattern after a lesion is uncovered. For instance, at times the interpreter may become so preoccupied with the first abnormality detected that a second or third lesion may be overlooked. This is a well-established phenomenon known as a “satisfaction of search error.”7,16 By definition, satisfaction of search errors represent omissions of underreading images. The satisfaction of search phenomenon is more likely to manifest when the first lesion is generally more attention-grabbing than the subsequent, more subtle lesion. 124
Although the causes of satisfaction of search errors are not explicitly defined, these errors may be reduced if interpreters are aware of the tendency to miss subsequent lesions, and hopefully develop a tendency to closely look for a second lesion whenever a first lesion is found, a third when a second is found, and so on until the anatomy is viewed completely. A complete search pattern is the only defense to avoid this well-known pitfall of image interpretation.
6. Compare what is seen with the “mind’s eye of normal.” After a review of the patient’s demographics, the rationale for examination, and technical issues related to the image, image interpretation next begins with a thorough search of the displayed anatomy for any deviations from normal. This step is the most crucial of the film interpretation process. Image interpretation requires an excellent knowledge of normal anatomy. Abnormality quickly catches the eye when normal is understood. 87
7. Common things are commonly seen (or, rare things are rarely seen). This concept underscores the importance of trying to explain the cause of abnormal findings by starting with the common pathologies and working to the less common differentials. For instance, a fragmented, radiodense, small proximal epiphysis appearing on hip radiographs of a 6-year-old boy could signify hypothyroidism, but there is a better chance that it represents traumatically induced avascular necrosis.
8. Be proactive, not reactive. Excluding common pathologic presentations should be proactively attempted; that is, pathologies that are common to some radiographs should be routinely investigated. For example, when an anteroposterior (AP) open-mouth projection is viewed, an odontoid fracture should specifically be looked for. Signs of an aneurysm of the abdominal aorta on a lateral lumbar projection, a femoral neck fracture on an AP view of the pelvis, and so on should be checked. Features of the pathology should not simply be reacted to; common pathologic presentations should be proactively eliminated, especially those suggested clinically.
9. There is no substitute for experience. Critically interpreting large numbers of radiographs will help interpreters develop a strong sense of normal anatomy, and allow subtle abnormal shadows to be more apparent.
10. Consult with someone on difficult or ambiguous cases. The social literature says that two minds are better than one. A group decision generally is more accurate than an individual conclusion. Keeping with this theme, when ambiguous findings are recognized or intuitively suspected, it may be helpful to obtain a second opinion to resolve any controversy and arrive at a valid film interpretation. Interestingly, research suggests that when asking another interpreter to view the film, it is better to blind the second interpreter to the suspicious areas of the film found by the first examiner. Swenson and Theodore142 found that second interpreters of chest films were more accurate if they read the films using a “free search pattern,” unencumbered and independent of the exact prior concerns of the first interpreter. The theory that supports this assertion is described as “superiority of search.” The theory holds that when interpreters review standard radiographic views (e.g., posteroanterior (PA) chest film), they go through a process of skilled perceptual filtering that allows them to recognize abnormal findings. Diagnostic radiology is a visual interpretation reliant on knowledge and visual acuity. It is dependent on the ability to sort information to arrive at clinically meaningful conclusions. Moreover, if the search pattern used by the radiologist is interrupted (in this case, by being tipped off to what to look at), the perceptual mechanisms are bypassed, resulting in a less accurate interpretation. 142 There is empiric evidence that second opinions are helpful to the interpretation of chest radiographs, 67,159 barium enemas, 103 and mammography. 6,25,29
11. Search for links between findings and various views. Cognitively linking related findings together should be attempted in hopes of developing a perceptional flow to the image interpretation. Triangulation between the available views of the region (e.g., PA and lateral chest or AP, AP open-mouth, lateral cervical spine) should be used. Some interpreters embrace the concept that related anatomy should be reviewed together. For instance, when viewing a PA chest film it makes more sense to view all of the ribs separate from viewing the pulmonary tissues, as opposed to viewing the first rib and estimated pulmonary tissues concurrently.
12. Eliminate extraneous light. The ambient room light should be low, and view boxes that are not displaying images should be turned off.
13. Compare current findings with those on past radiographs. Past imaging studies are very useful to aid in the interpretation of current radiographs. 12,156 Berbaum found that normal comparison images were especially helpful for those interpreters who were in the earlier stage of training. 12 This is believed to be related to the perceptual operation in which single perceptions from the old and new film combine to form a common, third, unique perception. Comparison with past radiographs also helps to document the progression of a lesion. The stability of a lesion over time is a key predictor of its aggressiveness. For example, a 1-cm lung nodule not seen on radiographs 6 months previously likely indicates a malignant etiology of the nodule. If the nodule was on an early film and of consistent size on the past images, an etiology of granulomatous infection is likely to explain the nodule. However, caution is necessary. At times the progression of a pathology may be so subtle as to be missed when very recent past radiographs are viewed. Use of multiple comparisons, including old past images, is best to avoid this pitfall.
14. The problem is perception. Image interpretation is a function of perception more than visual acuity. The question is not what can be seen, but identifying what is seen. Interpreters tend to overlay personal bias onto the process of image interpretation. It takes discipline to focus on the objective interpretation of the demonstrated anatomy. Perception is made better by experience and continually correlating what is seen to what is actually present. This is learned best by iterations of comparing one’s interpretation with that of someone more proficient.
15. Is the abnormal finding real? When abnormal shadows are seen on the image, it should first be considered that they may represent nothing more than a presentation of normal anatomy, artifact, or confluence of overlying shadows. It is common for superimposed structures to form a resultant shape. For instance, the pulmonary arteries coursing in multiple directions across the lung may combine to give the appearance of a circular, cystic pulmonary defect. The resulting “virtual image” is termed a subjective image. It is not real; rather, it is an illusion conjured in the mind of the interpreter.
16. Give special attention to the problem areas of the radiograph. Some areas on the film are more likely to contain pathology than others. For instance, attention must be paid to interpret the lung apices on the AP lower cervical radiograph; the atlantodental interval and sella turcica are important areas that are often neglected on the lateral radiograph. Problem areas for various projections are listed in FIG. 5-12FIG. 5-13FIG. 5-14FIG. 5-15FIG. 5-16FIG. 5-17FIG. 5-18FIG. 5-19 and FIG. 5-20. Generally, special attention should be given to the overexposed, radiolucent areas of all projections as common sites for pathology.
17. Be organized. Successful film interpretation requires some attention to detail. The patient’s images should be accompanied by a correlating history and pertinent clinical data, inclusive of any past imaging studies that may assist the interpretation. Resources (e.g., books, rulers, protractors, voice recorders, alcohol to erase pencil lines, dry erase markers for annotating abnormal findings) should be close at hand. Part of being organized involves consistency in how the images are assembled on the view boxes. For instance, many interpreters feel compelled to place the lateral radiographs on the view box so the patients are facing to the interpreter’s reading left, or view the films in a consistent sequence: lateral … AP … oblique, etc.
18. Attention to environment. The film reading environment should be quiet and free of distractions. Maintaining low ambient room light and turning off view boxes without films are both empirically associated with successful image interpretation.
19. What is the clinical impact? The purpose of diagnostic imaging is to gather data to assist clinical decision making. Therefore all abnormal findings should be interpreted in light of their clinical significance with appropriate follow-up imaging or procedures formulated into the report generated from the images.
20. Do not ignore intuition. The largest portion of the variation in film interpretation is unexplained. Sometimes the only predictor of an abnormality is that lingering sense that something is being missed. This feeling often drives extra attention that may eventually reveal a subtle defect. Perhaps the eyes are seeing something that the brain cannot immediately comprehend.
21. Resist overinterpreting the study. No matter how closely they are scrutinized, plain film radiographs do not reliably detail a disc lesion, ependymoma, hydrosyringomyelia, or a host of other defects. The clinical utility of the imaging modality must always be matched to the clinical question, and the modality’s limitations must be considered. The temptation must be resisted to assume that the patient’s problem is illustrated on the imaging study being reviewed. Also, a link must not be assumed between the patient’s clinical problem and radiographic abnormalities that happen to be present. The early literature is replete with assumptive correlations that could not be supported when investigated in greater depth.
22. Confirm findings with other views or studies. If findings are equivocal, further views, contrast, specialized imaging, and so on should be used to increase the certainty about something found.
For example, after careful review of the anteroposterior (AP) and lateral projections of the 56-year-old woman shown in Figure 5-6, it is apparent that the x-ray quality could be better. The patient is a large woman, and the typical problems of this circumstance are exhibited on these radiographs, such as the general “gray” appearance of the images related to excessive beam scatter. The anatomy of the lateral projection appears more radiodense in the lower portion of the lumbar spine and sacrum because the patient is wider at her hips than waist. Also, the overlying osseous shadows of the ilia add radiodensity. A skin fold creates a radiolucent transverse band at the level of the L3 disc space on the lateral projection. A degenerative spondylolisthesis is noted at L4 on L5. Multiple metallic clips are noted incidentally on the anteroposterior (AP) projection positioned along the periphery of the pelvis. The clips are related to a surgical procedure the patient underwent months earlier to remove a uterine carcinoma. Unfortunately, the surgical removal was not curative, and pulmonary metastasis is evidenced by the large mass appearing immediately superior to the apex of the diaphragm adjacent to the gastric air bubble, as seen on the lateral projection (Fig. 5-6, A). The presentation of the lung mass at the periphery of the film could cause it to be missed during initial review of the radiograph. Lesions appearing on the periphery of the film are not as evident as those appearing in the center. Remembering to give equal attention to the periphery of the image and adhering to the other principles of film interpretation (many listed in Box 5-2) reduces the rate of missed lesions.
 |
| FIG. 5-6 A, Lateral and, B, anteroposterior projection of the lumbopelvic skeleton (see text for description of the findings). |
Perceptual variations are more likely to occur when the lesion is subtle and its clinical interpretation is unknown or undecided. There are also limitations in the visual process. Two such limitations (ambiguous images and Mach bands) are discussed in the following.
Ambiguous image.
When it comes to plain film radiography, our visual systems are constrained by interpreting two-dimensional representations of three-dimensional anatomy. The mental image formed may represent assumptions made of the depth of every point in the image. These assumptions may change over time, yielding dramatically different anatomic interpretations. This phenomenon can be self-demonstrated by viewing ambiguous images (Figs. 5-7 and 5-8). Ambiguous images cause perceptional vacillation, although the optical input remains constant. Fluctuations in perception are thought to reflect ambiguous information about the nature of an object at a given location in visual space. The brain reacts to uncertainty by fluctuating between different neural states over time. 8,80 Ambiguous images and other pitfalls of image perception and interpretation are possible. Generally, the film interpreter is cautioned not to assume that perception is reality.
 |
| FIG. 5-7 Ambiguous image. An ambiguous image has the potential for more than one interpretation. For example, notice that the white cup can also be interpreted as the profile of two dark gray opposing faces. |
 |
| FIG. 5-8 Ambiguous image. A classical ambiguous image was developed by E.G. Boring, and inspired by earlier renditions of the image that appeared on postcards and advertisements. The image depicts a young woman from the perspective of looking over her left shoulder as she wears a large boa and hat with a posteriorly directed feather. If you look at the image long enough, instead of a young woman, you will see an old woman from her left anterior perspective. The jaw line of the young woman becomes the lower margin of the nose of the old woman, the young woman’s ear becomes the old woman’s left eye, and the young woman’s necklace becomes the old woman’s month, partially open. Ambiguous images arise from difficulties in interpreting three-dimensional structures from two dimensional imaging modalities. The film interpreter is cautioned to consider the impact of ambiguous images on their perceptions during image interpretation. (From Boring EG: A new ambiguous figure, Amer J Psychol 42: 444, 1930.) |
Mach bands.
A Mach band illusion is another common source of radiographic misinterpretation (Fig. 5-9). The human visual system may accentuate an abrupt change in brightness of an image so that regions of constant brightness appear to have varying brightness. This appearance is an illusion caused by the brain trying to enhance the contrast between slightly different hues of color (or gray scale). For example, in an AP open-mouth projection of the upper cervical spine, there may appear to be a transverse fracture of the odontoid process immediately adjacent to the overlapping anterior arch of the atlas. This illusion is caused by a perceived change in the radiodensity of the odontoid process (Fig. 5-10). A band of perceived (but not real) contrast enhancement is termed a Mach band. 49 A Mach band appears as a thin bright band on the lighter side and a thin dark band on the darker side of the gray scale, or color, gradient. Verification of a Mach band can be performed by a densitometer; the meter will not fluctuate across the perceived contrast enhancement.
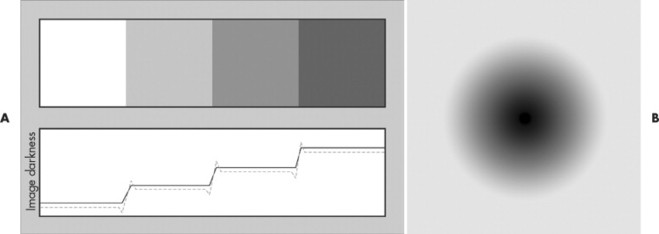 |
| FIG. 5-9 Mach bands. The human visual system may accentuate an abrupt change in brightness of an image so that selected regions of constant brightness appear to have varying brightness. A, For example, the gradient above has three even steps, but there is a perception of a brighter strip immediately before each gradient change and darker strip immediately after the gradient change. This phenomenon can be graphically represented by the solid black line indicating the three steps in brightness that occur between each of the four shades of gray scale. The human visual system will accentuate the actual (black line) change in brightness to give the illusion of darker stripes parallel to and just before the gradient change and brighter line running parallel to and immediately after the gradient change. This perceived gradient change is depicted by the dashed blue line. B, Another example is this circular gradient change. Notice how there appears to be a white halo around the black (center) to white (periphery) gradient. In this example, the white halo is a mach band. |
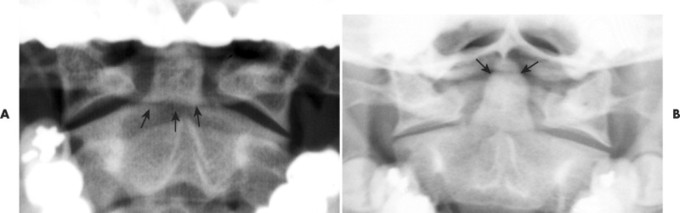 |
| FIG. 5-10 Mach bands across the odontoid process. A, Notice the radiolucent line across the base of the odontoid process (arrows). The radiolucent line is not real, but rather is caused by the overlapping posterior arch of the atlas above. The overlapping posterior arch changes the density gradient of the image and promotes the interpretation of a radiolucent line adjacent to the radiodense shadow. The odontoid is not really fractured. B, The overlapping inferior margin of the skull causes the appearance of a separated tip of the odontoid process (arrows). As in A, the odontoid is not really fractured. At times, it is difficult to separate a Mach band from a true fracture. When in doubt, the projection could be retaken with a slightly different head tilt. On the repeat radiograph, the Mach band should move; the fracture will not. |
APPEARANCE OF THE RADIOGRAPH
A typical family photograph is a positive image. Everything that is white appears white; everything that is black appears black; and so on. A radiograph is a negative image. In reference to subject density, dense structures (a function of mass and volume), such as metal and bone, appear whiter than do less dense structures, such as fat or water. In this sense, the radiograph is a shadow of anatomy. Dense structures impede more of the x-ray beam from striking the radiographic film; therefore after chemical development, the area appears white (or light gray) when the radiograph is back-lighted on a view box. Less dense anatomy appears dark gray or black on the film. The term radiopaque describes dense structures that block most of the x-ray beam and consequently appear white on the radiograph. The term radiolucent describes less dense structures that block little of the x-ray beam and consequently appear dark gray or black on the radiograph. In distinction to subject density, film density describes the film’s ability to stop light passing through the film.
The final appearance of the radiograph is a function of the summation of many superimposed structures. It may be that several superimposed structures of medium to low density appear on the radiograph as a lighter gray shadow than a single dense object. An x-ray beam that traverses a thin bone may appear more radiolucent (sometimes termed less dense) than when the same x-ray beam traverses a medium-sized organ (e.g., water density). In general, five radiographic densities are listed—metal, bone, water, fat, and air—from most radiolucent (black) to most radiopaque or radiodense (white) (Fig. 5-11). Of course, metal does not occur in the body naturally but may be present after surgery, dental work, or foreign body intrusion; or reflect the presence of overlying artifacts (e.g., necklaces or earrings).
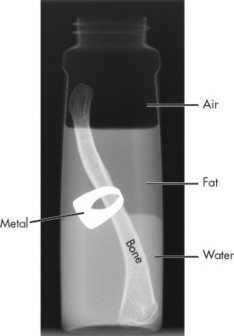 |
| FIG. 5-11 Five radiographic densities. This is the radiograph of a baby’s bottle in which the lower third of the bottle is filled with water, the middle third is filled with with oil (fat), and the upper third is left open to air. A clavicle and ring are inserted into the beaker. The constituents resemble each of the five radiographic densities of air, oil, water, bone, and metal, listed from black (radiolucent) to white (radiodense). |
Image interpretation involves gathering visual information to produce specific perceptions. The attitudes, beliefs, biases, and expectations of the examiner influence both what is observed during visual assessment and what is concluded from those observations. Although film interpretation is truly an art, generally accepted sequential steps define the process of image interpretation (Box 5-3). The first step is for the interpreter to become familiar with the study’s clinical rationale. Is a fracture suspected? Does the 65-year-old patient with unrelenting low back pain have a history of night pain, unexplained weight loss, or past malignancy? Next the images should be viewed completely with a thorough visual search path. A complete search path is used to ensure that all of the anatomy has been observed. The best search path is a unique one developed by the interpreter over time, which compensates for the interpreter’s inherent weaknesses in observation. For instance, if an interpreter has difficulty remembering to look at the sella turcica on a lateral radiograph of the cervical spine, the search path should be altered to emphasize that region; this will compensate for the interpreter’s inherent tendency to underinterpret that portion of the film.
BOX 5-3
Steps in Radiographic Interpretation
1. Understand the clinical rationale for the study.
2. Search the images for abnormal findings.
3. List and define any abnormal findings.
4. Summarize any abnormal findings by either concluding on an obvious diagnosis (an Aunt Minnie) or attempting to identify a general pattern or gamut described by the abnormal findings. Selected radiologic patterns of abnormality are listed in Box 5-13.
5. Integrate the radiologic findings and list of possible diseases that may explain these findings with pertinent data obtained from the history, clinical examination, laboratory testing, and further or past diagnostic imaging. The goal is to follow a systematic, rational process that narrows the list of radiologic and clinical considerations to identify a definitive diagnosis that will assist in successful patient management.
ABCS of film interpretation.
The ABCS of film interpretation describes a commonly taught generic search path for film interpretation. “ABCS” is a learning aid to prompt the interpreter to review all of the imaged anatomy by concentrating on four components in a fixed sequence: alignment, bone, cartilage (joint spaces), and soft tissue separately. By deconstructing the search path into manageable components (e.g., alignment and bone), the interpreter is less likely to omit aspects of the anatomy from the search path. Instead of following the ABCS format in direct sequence, some interpreters prefer to inspect the areas in other sequences, such as BCAS (bone, cartilage, alignment, and soft tissue) or ACBS (alignment, cartilage, alignment, and soft tissue).
Alternatively, some interpreters like to employ a “free” search pattern that allows interpreters’ gaze to scan the anatomy in any sequence that grabs their visual attention. Regardless of the method (fixed or free), the search path must be comprehensive for reasons of accuracy, and concise for reasons of practicality.
Use of checklists in film interpretation.
Some interpreters, especially beginners, are helped by consulting checklists of structures to assist in film interpretation. In a general sense, the ABCS approach to film interpretation is a brief checklist, reminding and sequencing the visual path of the interpreter through the presenting alignment, bone, cartilage (joint space) and soft tissues. All of the visualized anatomy needs to be closely scrutinized for possible defects.
BOX 5-4BOX 5-5BOX 5-6BOX 5-7BOX 5-8BOX 5-9BOX 5-10BOX 5-11 and BOX 5-12 present developed checklists to ensure a comprehensive review of selected radiographic projections. Developing a truly all-inclusive checklist for each radiographic projection listed is not feasible. Instead the checklists enumerate the major technical considerations and anatomy (ABCS approach discussed in the preceding), and list problem areas that require extra attention.
BOX 5-4
Interpretation Checklist for a Lateral Cervical Radiograph
Patient information
▪ Review and verify the date of examination and patient information.
Image quality
▪ Evaluate photographic properties: density, contrast, and noise factors (quantum mottle, fog, etc.).
▪ Evaluate geometric factors: size, shape, detail, and distortion.
Patient positioning and technical defects
▪ Are there signs of positioning errors, motion artifact, static marks, or other technical defects?
▪ Are the films done recumbent or upright?
Field of view
▪ Does the vertical field of view extend from the base of the occiput to below the C7 vertebra?
▪ Does the horizontal field of view include angles of the mandible to the C7 spinous process?
Common artifacts
▪ Are there stems of eyeglasses, earrings, necklaces, clothing, and so on?
Common foreign bodies
▪ Are there any dental fillings?
Alignment
▪ Is the cervical lordosis maintained?
▪ Is the tip of the odontoid vertically centered over the C7 body?
▪ Are the articular pillars offset, suggesting facet dislocation, or do they closely overlap as usual?
▪ Are the posterior borders of the rami of the mandible generally overlapped? (Projectional distortion causes them not to be directly overlapped.)
▪ Are the seven vertical lines maintained?
Line 1: along posterior tips of spinous processes
Line 2: along spinal laminal lines
Line 3: along posterior margins of posterior joints
Line 4: along anterior margins of posterior joints
Line 5: along posterior margins of bodies C2 to C7 (George’s line)
Line 6: along anterior margins of bodies C2 to C7
Line 7: along posterior margin of pharynx and tracheal air shadows
Bones
▪ Are radiodensity, size, shape, and configuration of each vertebra normal?
• Vertebral body
• Transverse process
• Pedicle
• Lamina
• Spinal laminar junction line
• Spinous process
• Odontoid process of C2
▪ Do the mandible, maxilla, and teeth appear normal?
▪ Are the radiodensity, size, shape, and configuration of the base of the skull normal?
▪ Is the sella turcica normal?
▪ Is the spinal canal maintained?
Joint spaces
▪ Is the atlantodental interval increased (>3 mm in adults or 5 mm in children)?
▪ Are the intervertebral disc spaces well maintained?
▪ Are cervical disc spaces wedged to the anterior?
▪ Are the posterior joint surfaces parallel with visible joint spaces from C3 to C7?
▪ Is the intervertebral foramen maintained?
▪ Is the space between the occiput and the atlas, and the interspinous spaces from C2 to C7 maintained?
Soft tissue
▪ Is the retropharyngeal space less than 5 mm at C2 and the retrotracheal space less than 20 mm at C6? (An in situ nasogastric tube will invalidate these measures.)
▪ Do the paranasal sinuses appear radiolucent?
▪ Is there physiologic calcification of the laryngeal cartilages?
BOX 5-5
Interpretation Checklist for an Anteroposterior Lower Cervical Radiograph
Patient information
▪ Review and verify the date of examination and patient information.
Image quality
▪ Evaluate photographic properties: density, contrast, and noise factors (quantum mottle, fog, etc.).
▪ Evaluate geometric factors: size, shape, detail, and distortion.
Patient positioning and technical defects
▪ Are there signs of positioning errors, motion artifact, static marks, or other technical defects?
▪ Are the films done recumbent or upright?
Field of view
▪ Does the vertical field of view extend from the angles of the mandible to the apices of the lung?
▪ Does the horizontal field of view include several centimeters of soft tissue on either side of the spine?
Common artifacts
▪ Are there eyeglasses, necklaces, hairpins, hair braids, clothing, and so on?
Common foreign bodies
▪ Are there any dental fillings, surgical staples from carotid enterectomy, and so on?
Alignment
▪ Is there a right or left cervical list or head tilt?
▪ Is there a right or left lateral curvature?
▪ Are the spinous processes generally aligned vertically?
▪ Is there a right or left laterolisthesis of any vertebrae?
Bones
▪ Are the radiodensity, size, shape, and configuration of each vertebra normal?
• Vertebral body
• Uncinate processes
• Transverse processes
• Pedicles
• Laminae
• Articular pillars
• Spinous processes
• Odontoid process of C2
▪ Are the radiodensity, size, shape, and configuration of the ribs normal?
▪ Are the radiodensity, size, shape, and configuration of the clavicle normal?
▪ Are the mastoid processes normal?
▪ Is the superior margin of the sternum normal?
Joint spaces
▪ Are the intervertebral disc spaces well maintained?
▪ Are the uncinate joint spaces well maintained?
▪ Are the costotransverse joints normal?
Soft tissue
▪ Is the piriform sinus, rima glottis, and tracheal air shadow midline?
▪ Does the paranasal sinus appear radiolucent?
▪ Are the apices of the lung clear of mass, infiltrate, or other defect?
▪ Is the aortic knob of normal configuration?
▪ Is there carotid artery calcification?
▪ Are the paraspinal tissues clear of mass or defect?
BOX 5-6
Interpretation Checklist for an Anteroposterior Open-Mouth Cervical Spine Radiograph
Patient information
▪ Review and verify the date of examination and patient information.
Image quality
▪ Evaluate photographic properties: density, contrast, and noise factors (quantum mottle, fog, etc.).
▪ Evaluate geometric factors: size, shape, detail, and distortion.
Patient positioning and technical defects
▪ Are there signs of positioning errors, motion artifact, static marks, or other technical defects?
▪ Are the films done recumbent or upright?
Field of view
▪ Does the vertical field of view extend from above the tip of the odontoid to below the C2 spinous process?
▪ Does the horizontal field of view extend laterally to the tips of the transverse processes of the atlas?
Common artifacts
▪ Are there artifacts such as tongue jewelry, hairpins, and so on?
Common foreign bodies
▪ Are there any dental fillings, and so on?
Alignment
▪ Are the widths of the lateral masses bilaterally comparable?
▪ Are the paraodontoid spaces symmetric?
▪ Does the lateral mass extend laterally beyond the margin of the superior articular processes of C2?
▪ Is the center of the C2 spinous process vertically aligned with the center of the odontoid process?
Bones
▪ Are the radiodensity, size, shape, and configuration of the atlas normal?
• Lateral masses
• Transverse processes
• Transverse foramen
• Anterior arch
• Posterior arch
▪ Are the radiodensity, size, shape, and configuration of the C2 segment normal?
• Odontoid process
• Body
• Pedicles
• Superior articular processes
• Spinous process
▪ Are the radiodensity, size, shape, and configuration of the base of the occiput normal?
▪ Are the occipital condyles normal?
▪ Are the rami of the mandible normal?
Joint spaces
▪ Is the occipitoatlantal joint space maintained?
▪ Are the atlantoaxial joints maintained?
▪ Is the C2-C3 disc space maintained?
Soft tissue
▪ Is there ossification of the stylohyoid ligaments?
BOX 5-7
Interpretation Checklist for a Lateral Thoracic Radiograph
Patient information
▪ Review and verify the date of examination and patient information.
Image quality
▪ Evaluate photographic properties: density, contrast, and noise factors (quantum mottle, fog, etc.).
▪ Evaluate geometric factors: size, shape, detail, and distortion.
Patient positioning and technical defects
▪ Are there signs of positioning errors, motion artifact, static marks, or other technical defects?
▪ Are the films done recumbent or upright?
Field of view
▪ Does the vertical field of view extend from above T1 to below T12?
▪ Does the horizontal field of view extend from near the sternum to include the posterior angles of the ribs?
Common artifacts
▪ Are there necklaces, hair braids, clothing, and so on?
Common foreign bodies
▪ Are there any sternal wires, pacemaker, valve prosthesis, and so on?
Alignment
▪ Is the thoracic kyphosis maintained?
▪ Is there any vertebral retrolisthesis or spondylolisthesis?
▪ Are the spinous processes generally aligned vertically?
Bones
▪ Are the radiodensity, size, shape, and configuration of each vertebra normal?
• Vertebral body
• Pedicles
• Spinous process
▪ Are the radiodensity, size, shape, and configuration of each rib normal?
▪ Is the spinal canal maintained?
Joint spaces
▪ Are the intervertebral disc spaces maintained?
▪ Is the intervertebral foramen of normal size?
Soft tissue
▪ Is the tracheal air shadow centrally located?
▪ Is the heart shadow generally of normal size and configuration?
▪ Are the lung tissues clear of mass, infiltrate, or other defect?
▪ Are the ascending, transverse, and descending segments of the aorta normal?
▪ Are the aortic-pulmonary window and hila defined and clear?
▪ Is the diaphragm of normal position?
▪ Is the gastric air bubble of normal size and location below the diaphragm?
BOX 5-8
Interpretation Checklist for an Anteroposterior Thoracic Spine Radiograph
Patient information
▪ Review and verify the date of examination and patient information.
Image quality
▪ Evaluate photographic properties: density, contrast, and noise factors (quantum mottle, fog, etc.).
▪ Evaluate geometric factors: size, shape, detail, and distortion.
Patient positioning and technical defects
▪ Are there signs of positioning errors, motion artifact, static marks, or other technical defects?
▪ Are the films done recumbent or upright?
Field of view
▪ Does the vertical field of view extend from above T1 to below T12?
▪ Does the horizontal field of view include about 7 cm of soft tissue on either side of the spine?
Common artifacts
▪ Are there necklaces, hair braids, clothing, and so on?
Common foreign bodies
▪ Are there sternal wires, pacemaker, valve prosthesis, and so on?
Alignment
▪ Is there a right or left lateral curvature?
▪ Are the spinous processes generally aligned vertically?
▪ Are there any right or left vertebral translations?
Bones
▪ Are the radiodensity, size, shape, and configuration of each vertebra normal?
• Vertebral body
• Transverse processes
• Pedicles
• Laminae
• Articular processes
• Spinous process
▪ Are the radiodensity, size, shape, and configuration of the ribs normal?
▪ Are the radiodensity, size, shape, and configuration of the medial segments of the clavicles normal?
▪ Are radiodensity, size, shape, and configuration of the sternum normal?