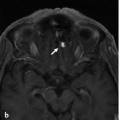
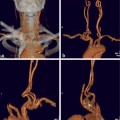
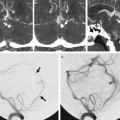
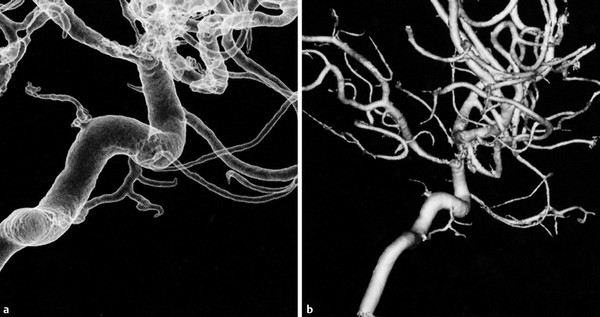
The Inferolateral and the Meningohypophyseal Trunk A 53-year-old woman presented with left ptosis 4 months before admission and subsequently developed swelling of the left eye and proptosis. Investigation demonstrated a dural arteriovenous fistula involving the cavernous sinus region on the left side with drainage toward the superior ophthalmic vein on the left. Arterial supply was through the inferolateral trunk (ILT) from the left internal carotid artery (ICA). A previous transvenous attempt to treat this fistula was unsuccessful, as the compartment that harbored the shunt and opened into the superior ophthalmic vein could not be reached. See ▶ Fig. 5.1. Fig. 5.1 Left ICA angiogram in lateral view (a) and 3D rotational reconstruction (b) demonstrates the left cavernous sinus dural AV fistula. The sole arterial supply identified was through an enlarged left ILT from the left ICA. There was early venous drainage through the left superior ophthalmic vein, as well as some early filling of the proximal aspect of the inferior ophthalmic vein. Although the superior ophthalmic vein filled early, flow through the vein was slow, with delayed emptying and contrast stasis. A microcatheter was advanced into the proximal portion of the left ILT. Microcatheter injection (c) confirmed stable position proximally in the left ILT and demonstrated filling of the fistula. Flow through the fistula was slow, presumably as the microcatheter was partially occlusive in the ILT. Despite multiple attempts with different microcatheter and microguidewire combinations, no distal position of the microcatheter could be obtained. As the security margin was perceived to be small, no liquid embolic material was used, and instead, the single low-flow fistulous-type dural arteriovenous fistula was treated with a transarterial ligation approach, using electrolytically detachable coils that were deployed via the ILT (d) into the distal fistulous segment of the ILT, which led to angiographic obliteration of the fistula. Control angiographies obtained 1 year later in both the ECA and the ICA (e) did not demonstrate fistula recurrence. Dural arteriovenous fistula of the cavernous sinus fed by the ILT. A variable number of arterial branches arise from the cavernous ICA, the most consistent of which are the meningohypophyseal trunk (MHT) and the ILT. The MHT projects posteriorly and laterally from its origin at the posterior genu of the cavernous ICA and subdivides into four branches: the tentorial marginal artery (or artery of Bernasconi and Cassinari), the dorsal meningeal artery (also known as the dorsal or lateral clival artery), the basal tentorial artery, and the inferior hypophyseal artery. The tentorial artery courses posteriorly along the roof of the cavernous sinus, toward the free margin of the tentorium. The dorsal meningeal artery runs superolateral to the abducens nerve into Dorello’s canal and supplies the dura of the clivus, where it anastomoses with the clival branches of the ascending pharyngeal artery. The basal tentorial artery runs along the roof of the petrous bone laterally along the border between the tentorium and the petrous ridge. The inferior hypophyseal artery supplies the medial wall of the cavernous sinus. The ILT arises from the horizontal segment of the cavernous ICA and also harbors three major branches: a superior, anterior, and posterior branch (▶ Fig. 5.2). Fig. 5.2 ICA angiogram 3D rotational reconstruction images (a,b) demonstrate the three major branches of the ILT: the superior, anterior, and posterior branches that extend toward the roof of the cavernous sinus, to the foramen rotundum, and to the foramen ovale, respectively.
5.1 Case Description
5.1.1 Clinical Presentation
5.1.2 Radiologic Studies

5.1.3 Diagnosis
5.2 Anatomy
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree