5 Variable Imaging Presentations of Lung Cancer
Summary
This chapter reviews the most common location and imaging characteristics of missed lung cancers as well as the variable imaging presentations of lung cancers. The newly revised classification system for adenocarcinoma of the lung is also discussed. Illustrative examples of adenocarcinoma in situ, minimally invasive adenocarcinoma, and invasive adenocarcinoma are provided. The concept of malignancy rate based on lesion morphology and doubling times is also presented.
Keywords: missed lung cancers, adenocarcinoma, classification, atypical adenomatous hyperplasia, minimally invasive adenocarcinoma, adenocarcinoma in situ, invasive adenocarcinoma, lepidic, mucinous, solid, subsolid, ground glass, doubling time
5.1 Introduction
On conventional chest radiography, the variable manifestations of lung cancer may be broadly characterized as indirect or direct. Indirect radiographic manifestations include atelectasis, often related to an endobronchial lesion or extrinsic compression of the airway by adjacent lymphadenopathy and nonresolving pneumonia-airspace disease. Direct radiographic manifestations of lung cancer may include a nodule(s) (< 3.0 cm diameter), mass (≥ 3.0 cm diameter), and parenchymal consolidation (▶ Table 5.1).
Indirect signs | Direct signs |
Atelectasis | Nodule |
Nonresolving pneumonia-airspace disease | Mass |
Focal consolidation |
5.2 Location and Imaging Characteristic of Missed Lung Cancers
As stressed earlier, conventional radiography is not the optimal screening tool for the early detection of lung cancer. Austin et al reported the vast majority of missed bronchogenic cancers on retrospective review occur in an upper lobe (81%) (3 upper lobe: 2 lower lobe), and in the right upper lobe in particular (56%) (3 RUL: 2 LUL). More missed lung cancers occurred in women (67%) than in men (33%). Other problematic radiographic regions where missed lung cancers occurred included the perihilar and paraspinal regions (▶ Fig. 5.1). The mean diameter of the missed lung cancer was 1.6 ± 0.8 cm (range: 0.6–3.4 cm). Shah et al revisited this topic in 2003 and again found that most missed potentially resectable primary lung cancers were located in the upper lobes (right: 45%; left: 28%; total: 72%), especially the apical and posterior segments or subsegments (60%). The clavicle obscured visualization of 22% of the missed cancers. The missed cancers had a median diameter of 1.9 cm. The high percentage (54–90%) and large average size (1.3–1.6 cm) of missed primary lung cancers on conventional chest radiographs have been reported in numerous additional studies. Potential contributing causes for failed radiographic detection include obscuration of the lesion from superimposed intrathoracic and extrathoracic structures such as the ribs, clavicles, hilar vessels, and the heart.

In 2002, Li et al reported 83 primary lung cancers were found during an annual low-dose computed tomography (LDCT) screen and confirmed at either biopsy or surgery. Thirty-two (38.6%) of these lung cancers were missed on 39 initial CT scans: 23 scans due to detection errors and 16 scans from interpretation errors. All of the missed lung cancers were intrapulmonary. Of these missed cancers, 88% were stage IA. All detection error cases involved adenocarcinomas. Eighty-five percent were well-differentiated lesions and 55% were in nonsmoking women. The mean size of missed cancers in this patient population was 9.8 mm. The mean size of missed lung cancers due to interpretation error was 15.9 mm. Ninety-one percent of the missed nodules in the detection error group were ground glass. In the detection error group, 83% of the missed lung cancers overlapped with or were obscured by similar-appearing adjacent normal structures such as pulmonary vessels. In all, 87.5% of CT scans with interpretation errors were associated with a background of concomitant complex disease. Most missed cancers tended to be central or endobronchial, adjacent to scars or vessels and of low attenuation.
On LDCT, lung cancers may have a variable appearance. Lesions may appear as well-defined, solid noncalcified nodules, subsolid pure ground-glass, and as part-solid nodules. Additional morphologic features may include lobulation, concave notching, desmoplasia, pleural retraction, internal lucencies, and pericystic nodularity. These varying morphologic appearances will be illustrated in the remainder of this textbook.
5.3 Revised Adenocarcinoma Classification
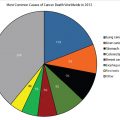
Non–small cell lung cancers (NSCLC) account for about 85% of all newly diagnosed lung cancers. Adenocarcinoma is the most common variety. The prevalence of adenocarcinoma is increasing and it presents more frequently in asymptomatic women, and often in nonsmokers. Recently, the International Association for the Study of Lung Cancer/American Thoracic Society/European Respiratory Society (IASLC/ATS/ERS) introduced new terminology and diagnostic criteria to better reflect our understanding of the heterogeneous pathology, imaging features, and clinical behavior of peripheral lung adenocarcinomas (formerly known as bronchioloalveolar cell carcinoma). The new classification system clearly distinguishes between preinvasive, minimally invasive, and frankly invasive lung lesions (▶ Table 5.2).
The imaging spectrum of these precancerous and cancerous lesions ranges from pure ground-glass nodules to part-solid nodules to solid nodules and masses (▶ Fig. 5.2). A pure ground-glass nodule manifests as a focal area of increased attenuation that does not obscure visualization of the underlying lung parenchyma (e.g., bronchovascular bundles; ▶ Fig. 5.3 a; ▶ Fig. 5.4). A subsolid nodule is an opacity that is less dense than solid and is further subdivided into part solid and pure ground glass (▶ Fig. 5.2). A part-solid nodule contains both solid high-attenuation elements and ground glass (▶ Fig. 5.5). A solid nodule manifests as a focal region of increased attenuation through which normal bronchovascular structures cannot be seen or are completely obscured (▶ Fig. 5.6).





Noguchi et al demonstrated that those patients with ground-glass nodular opacities identified on screening LDCT have a better prognosis than patients with solid nodules.
Histopathologically, the ground-glass opacities show a lepidic growth pattern. More specifically, the cancer cells use the normal pre-existing alveolar septa as a “scaffold,” growing along it without invading the stroma, pleura, or vessels. The lung cancer–screening literature also shows a higher rate of malignancy in incidental part-solid nodules compared to incidental solid nodules.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree