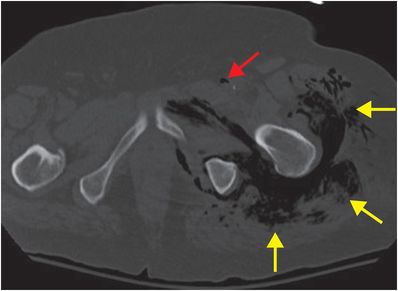
Diagnosis: Necrotizing fasciitis
Unenhanced axial CT of the pelvis demonstrates marked subcutaneous and deep fascial emphysema within the left thigh (yellow arrows) and in the left common femoral vein (red arrow).
Discussion
Necrotizing fasciitis is a rapidly progressive infection that may involve any soft tissue layer.
Immunocompromised and elderly patients are at increased risk. Predisposing factors include diabetes mellitus, superficial injury, cellulitis, surgery, and insect bites.
Infection by a single organism occurs in about 15% of cases, with the remainder of cases caused by multiple aerobic and anaerobic organisms.
Mortality rates range from 30–70%. Patients with severe, uncontrollable infection may die of septic shock with renal or multi-organ system failure.
In addition to the risk of overwhelming systemic infection, affected patients are at risk for extensive soft tissue or limb loss.
Given that necrotizing fasciitis tends to be rapidly progressive, time is of the essence in preventing morbidity and mortality.
Diagnosis may be challenging due to nonspecific and variable clinical presentation, most often with fever and vague pain. Therefore, it is important to have high clinical suspicion in susceptible patients.
The classic clinical examination finding is dusky, “wooden” skin with mottled purple patches; however, this finding often does not develop until late in the course of disease.
Presentations occur along a spectrum, and skin findings may even be normal.
Early in the course of disease, pain may be absent or decreased relative to the extent of injury if there is damage to peripheral nerves. Common early clinical findings include pain and tachycardia. Late findings include severe pain, skin discoloration, and multi-organ system failure.
Although necrotizing fasciitis may affect any part of the body, the extremities, perineum (Fournier gangrene), and trunk are most commonly involved.
Necrotizing fasciitis may progress rapidly in a short period of time – initial radiographs may be normal or show only soft tissue swelling.
The hallmark radiographic finding of soft tissue gas is seen only in a minority of cases.
CT and MRI may be extremely helpful in diagnosis. Findings include edema, soft tissue gas, and fascial thickening and enhancement.
Soft tissue gas can be difficult to detect on MR, but when present, can appear as focal susceptibility effect. Radiographs or CT may be helpful for confirmation.
Ultrasound is more useful in the pediatric population. Findings include distorted fascial planes, subcutaneous edema, and fluid accumulation.
Aggressive and timely surgical debridement, IV antibiotic therapy, and supportive care are key in management.
Clinical synopsis
The patient underwent emergent surgical debridement and was treated with IV antibiotics.
Self-assessment
|
|
|
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








