6 Choroid Fissure Cyst
6.1 Case Presentation
6.1.1 History and Physical Examination
A 5-year-old girl with a 1-year history of occasional mild occipital headache admitted to the ER (emergency room) because of a facial laceration from a fall.
The patient had a small facial laceration but was otherwise normal with no neurological deficits.
6.1.2 Imaging Findings and Impression
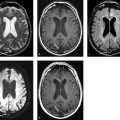
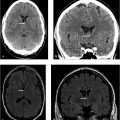
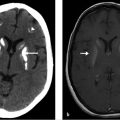
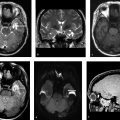
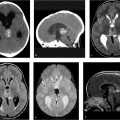
Axial (▶ Fig. 6.1a) and coronal (▶ Fig. 6.1b) CT scans of the head without contrast demonstrate a well-circumscribed cerebrospinal fluid (CSF) density lesion (white arrows) measuring approximately 10 × 10 mm in the choroidal fissure. The lesion has an imperceptible wall with no evidence of a solid component within the cyst.

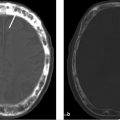
However, MR was performed to exclude the less likely possibility of a small cystic lesion. The cyst follows CSF signal intensity on axial T1-weighted (black arrow on ▶ Fig. 6.1c), axial fluid-attenuated inversion recovery (FLAIR; ▶ Fig. 6.1d), and coronal high-resolution fast spin-echo (FSE) T2-weighted (▶ Fig. 6.1e) images (white arrows). Coronal image (▶ Fig. 6.1e) clearly shows that the 10-mm cyst lies within the choroidal fissure. The distinctive spindle shape of the lesion is best seen in the T1-weighted sagittal plane (asterisk on ▶ Fig. 6.1f). The lesion does not show restriction on diffusion-weighted and ADC (apparent diffusion coefficient) map images (arrows on ▶ Fig. 6.1g,h).
6.2 Differential Diagnosis
Choroid fissure cysts:
Choroid fissure cysts are a normal variant occurring in the choroidal fissure and follow the CSF signal intensity on all sequences, with the absence of nodular enhancement.
Mesial temporal sclerosis:
This is rarely an incidental finding but rather a common cause of epilepsy.
The hippocampus (uni- or bilateral) is atrophic with abnormal signal intensity on FLAIR images and with loss of normal internal architecture on T2-weighted images.
The ipsilateral fornix is also often noted to be small.
This atrophy may result in ipsilateral widening of the temporal horn and choroidal fissure.
The primary abnormality of the hippocampus and secondary widening of adjacent CSF spaces should distinguish this from a choroid fissure cyst in which the adjacent brain is displaced due to mass effect but is otherwise normal. 1
Epidermoid cysts:
They are more commonly found in the CPA (cerebellopontine angle) cistern.
Epidermoid cysts do not suppress on FLAIR images completely and are bright on diffusion-weighted images, unlike choroid fissure cysts.
Parasitic cysts (neurocysticercosis):
They are more common in tropical countries.
Typically, they are parenchymal but can be present in the subarachnoid space.
The vesicular stage of neurocysticercosis (tapeworm infection) can look similar, but the cysts are most often multiple.
Nonenhancing T2 hypointense/T1 hyperintense scolex can be identified within the cysts.
They evolve into colloidal vesicular, granular nodular, and nodular calcified stages over time.
Hippocampal sulcus remnants:
They are multiple tiny cysts within the hippocampus itself and are therefore seen just medial to the temporal horn of the lateral ventricle but between the dentate gyrus and subiculum.
They are incidental findings and follow the CSF signal intensity on all sequences.
DNETs (dysembryoplastic neuroepithelial tumors):
Intra-axial mass/masslike abnormalities as opposed to a choroid fissure cyst that may compress adjacent brain but is extra-axial in location.
They often occur in the temporal lobes and have a pseudocystic/bubbly appearance.
They do not suppress on FLAIR sequences and often have a bright rim, which should help distinguish them.
Calcification and cortical remodeling may be seen.
Contrast enhancement is unusual. 2
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree