|
|
| Variant/Artifact |
Comments |
| Atlas |
| Agenesis of the anterior arch of the atlas (Figs. 7-16 and 7-17) |
Agenesis of the anterior arch of the atlas has been reported extremely rarely. Hypoplasia of the anterior arch is relatively more common but remains rare. |
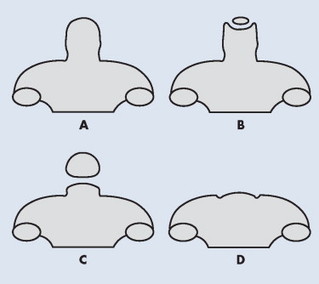
| Agenesis of the posterior arch of the atlas (Figs. 7-18 and 7-19) |
The posterior arch of the atlas begins to form from a secondary center of ossification during the second year of life, completely forming by the age of 3 or 4. Although typically viewed as a normal variant, there is a question of an associated defect of the transverse atlantal ligament, warranting flexion-extension radiographs in those affected. Enlargement of the C2 spinous process (megaspinous of C2) or enlargement of the anterior tubercle of atlas may be accompanying defects of agenesis of the posterior arch of the atlas. The latter is believed to be a stress response to the undeveloped portion of the atlas. |
| Atlantoaxial pseudojoint |
Uncommonly the posterior tubercle of the atlas approximates the superior margin of the spinous process of C2. The resulting frictional sclerosis has been referred to as a pseudojoint or Baastrup disease of the cervical spine. Baastrup disease is more common to the lumbar spine associated with degenerative reduction of the disc height with resulting approximation of the spinous processes. |
| Down syndrome |
Approximately 6% to 20% of those with Down syndrome demonstrate laxity of the transverse atlantal ligament and the ligaments from the lateral masses of the atlas to the occipital condyles, 109 jeopardizing the stability of the upper cervical spine and possibly resulting in irreversible spinal cord damage. Further discussion of this presentation is provided in Chapter 8. |
| Epitransverse process (Figs. 7-20 and 7-21) |
An epitransverse (supratransverse) process arises from the superior aspect of the transverse process of the atlas and extends superiorly to or near the occiput. 49,64 It is of little clinical significance unless significance synostosis between the atlas and occiput exists that limits range of motion across the occipitoatlantal joint. It is opposite to a paracondylar process, which arises near or at the occipital condyle and extends inferiorly to the transverse process of the atlas. |
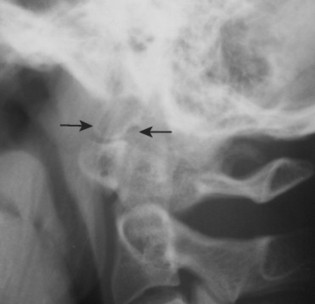
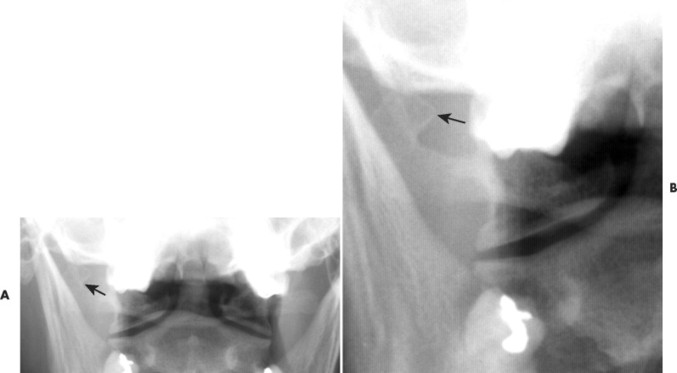
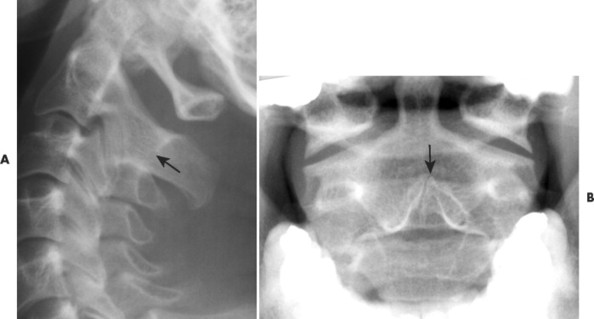
| Increased atlantodental interval (Figs. 7-22 and 7-23) |
The atlantodental interval (ADI) defines the joint space created by the posterior surface of the anterior tubercle of the atlas and the anterior margin of the odontoid process. Normally the space measures less than 3 mm in adults, and less than 5 mm in children because of their greater joint laxity. Enlargement of the ADI indicates joint instability secondary to trauma, inflammatory joint disease, congenital defect, and so on. (See Chapter 17 for a more detailed differential list.) As a normal variant, the ADI may appear V-shaped, opened superiorly. In such cases the lower margin of the joint should be used as a reference to measure the joint space. Sagittal plane flexion-extension radiographs may be used to stress the joint on equivocal cases of instability. |
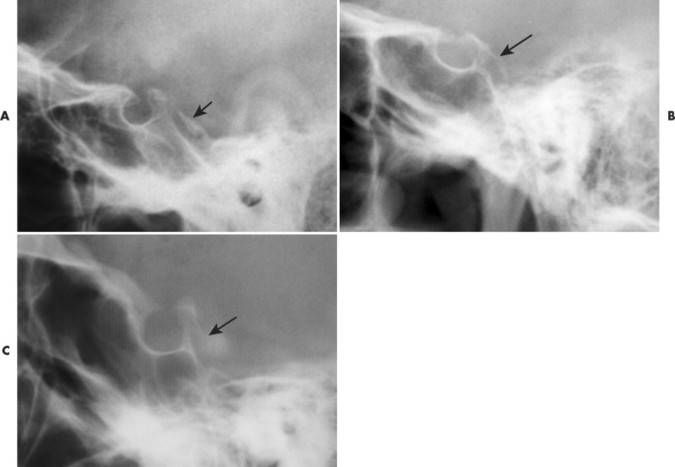
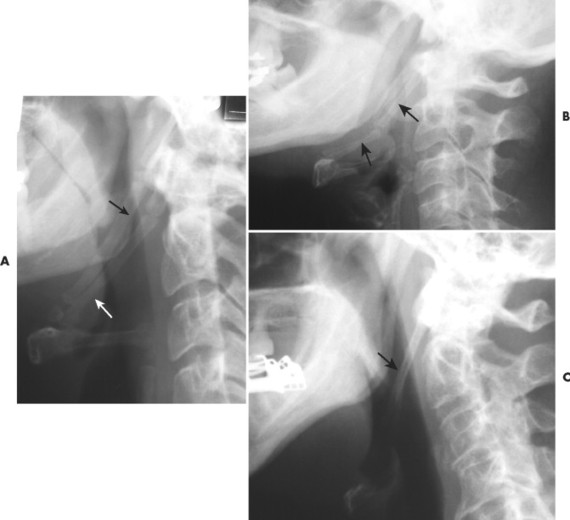
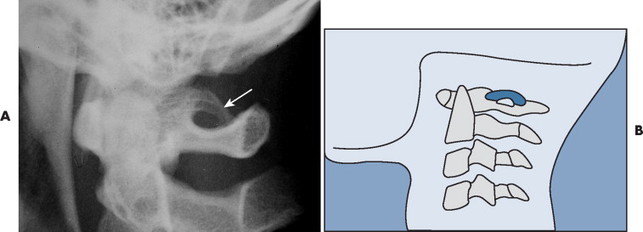
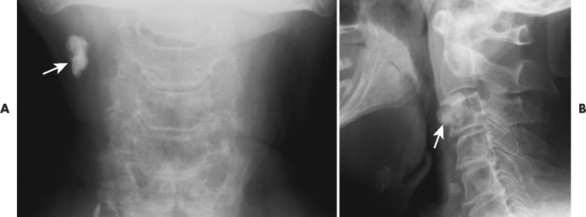
| Posterior ponticle of the atlas (Figs. 7-24 and 7-25) |
A posterior ponticle (also known as ponticulus posticus, foramen arcuale, Kimmerle anomaly, or Kimmerle variant) represents a small bridge of bone arching over the arcuate rim of the atlas (forming an arcuate foramen). Although traditionally attributed to ossification of the anterior margin of the atlantooccipital membrane, some believe it to represent well-organized bone formed from a distinct ossification center. 86 It is seen in approximately 15% of the general population and often is bilateral. It is more common among women when it presents as a partial bridge of bone, and more common in men as a complete bridge of bone between the lateral mass and posterior arch. 104 Although controversial, it is generally felt to be a variant of normal. Associations with headaches, Barr-Liéou syndrome, photophobia, and migraine have been reported. 4,16 Also, given that the vertebral artery passes through the defect, there is some concern for ischemia of the posterior cerebral circulation. Posterior ponticles are visualized on lateral or oblique cervical projections. Rarely a lateral variation, known as lateral ponticle, is seen on the anteroposterior open-mouth projection as an osseous bridge from the superior-lateral margin of the lateral mass of atlas to the lateral portion of the transverse process of the atlas. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Spina bifida occulta (Fig. 7-26) |
Spina bifida is a generalized term for congenital posterior midline defects of spine, alternatively known as spinal dysraphism, spondyloschisis, posterior rachischisis, or neural tube defects. Approximately 5% to 10% of the general population may have spina bifida occulta, the mildest form of midline defect. Spina bifida occulta usually is clinically insignificant; however, rarely (<0.1%) it may be associated with symptoms and other anatomic findings such as spinal lipomas, syringomyelia, and diastematomyelia. Rarely spina bifida occulta is associated with cervical spondylolisthesis, usually at C6. Spina bifida occulta is most common to the posterior arch of atlas or vertebral arch of S1, presenting as missing spinolaminar lines on lateral radiographic projections and as incomplete fusion of the posterior arch on the frontal projections. A complete discussion of this condition is found in Chapter 8. |
| Axis |
| Odontoid process agenesis (Fig. 7-27) |
Rarely a defect of ossification of the odontoid will result in an absent (agenesis) or small (hypoplasia) odontoid process of C2. Resulting instability of the atlantoaxial joint causes concern for spinal stenosis and spinal cord insult. Sudden death has been reported secondary to minor trauma. Atlantoaxial instability is more common among those with Down syndrome, Klippel-Feil syndrome, and skeletal dysplasias. The defect is well visualized on anteroposterior open-mouth projections. Computed tomography offers definitive evaluation. |
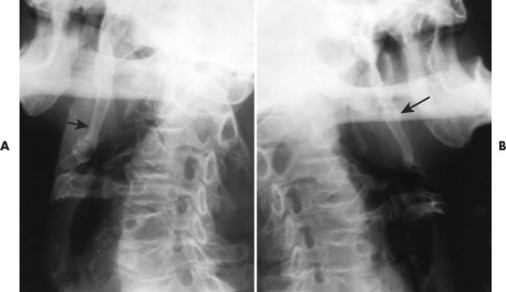
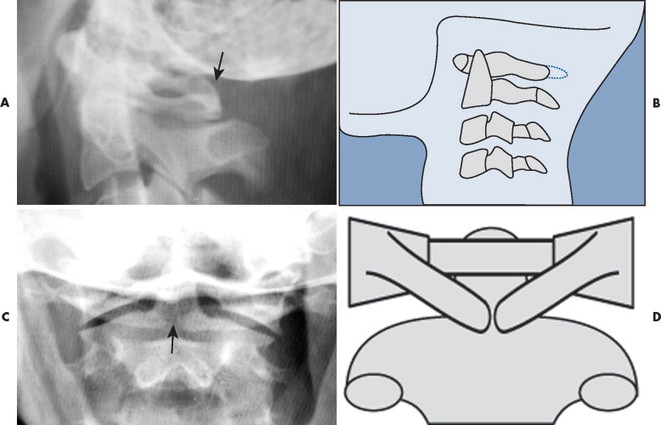
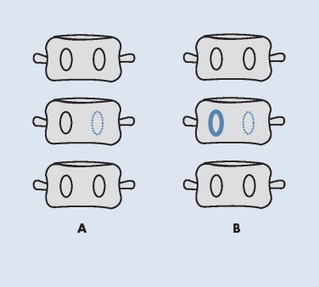
| Os odontoideum (FIG. 7-28FIG. 7-29FIG. 7-30 and FIG. 7-31) |
Persistence of the odontoid synchondrosis leads to the formation of a separate odontoid bone (os odontoideum) instead of a normally united odontoid process. The underlying mechanism of the defect is disputed, with both developmental57 and acquired36 etiologies proposed. It is a clinically significant defect, potentiating cord pressure related to atlantoaxial instability. The defect is well visualized on the anteroposterior open-mouth projection, and noted to a lesser extent on the lateral cervical projection. See Chapter 8 for complete discussion of the os odontoideum. |
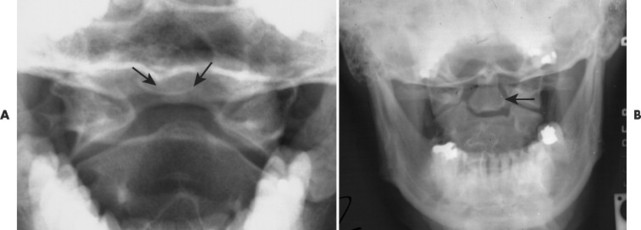
| Os terminale (Figs. 7-32 and 7-33) |
The tip of the odontoid process forms from a secondary center of ossification that presents at 3 years of age and fuses to the odontoid process by 12 years. Rarely the tip of the odontoid fails to unite, creating an os terminale (also known as a Bergmann defect). It should not be mistaken for a fracture, which demonstrates irregular margins, or an os odontoideum, which occurs lower. On the anteroposterior open-mouth projection, the os terminale appears as a smooth-bordered round, oval, diamond-shaped ossicle separated from and cephalic to the odontoid process. |
| Pseudosubluxation of C2 |
Typically, significant vertebral misalignment raises concerns for trauma, advanced degeneration, and instability. However, in children and teenagers under the age of 15 it is common to see significant anterolisthesis of 2 mm or more at C2 on C3 (and less common at C3 on C4) without any signs of trauma or degeneration. The finding is believed to be the result of immature muscles and other connective tissues present in the young. Pseudosubluxation of C2 is seen only on lateral cervical projections that demonstrate a neutral or flexion position of the cervical spine. Pseudosubluxations tend to resolve with cervical extension. This helps differentiate a pseudosubluxation from a true injury of the upper cervical spine with resulting anterior displacement of C2 (e.g., hangman fracture). However, caution should be applied to avoid patient extension among those demonstrating significant indicators of fracture. Computed tomography is most helpful in such cases. Also, a Swischuk’s line may be useful to differentiate pseudosubluxation from true injury. This line is drawn along the anterior margin of the posterior tubercle of C1 to the posterior aspect of the posterior arch (spinal laminar line) of C3. The posterior aspect of the posterior arch (spinal laminar line) of C2 should be within 1 to 2 mm of Swischuk’s line. A true subluxation is indicated by posterior deviations of more than 2 mm and pseudosubluxation by deviation less than 2 mm. 105 |
| Spina bifida occulta (Fig. 7-34) |
Spina bifida occulta is a small midline defect, sometimes occurring at C2. Spina bifida occulta is described in greater detail in the atlas or lumbar entries of this chapter, as well as in Chapter 8. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| C3-L5 |
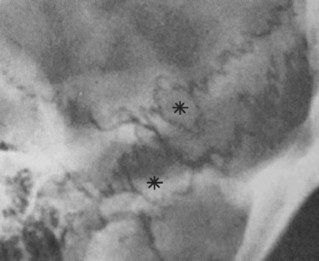
| Agenesis of the pedicle (FIG. 7-35FIG. 7-36FIG. 7-37FIG. 7-38FIG. 7-39 and FIG. 7-40) |
Aplasia of the pedicle is uncommon, and represents a unilateral developmental defect of the cartilage anlage dedicated to forming one half of the posterior arch of the vertebrae. Empiric evidence suggests that congenital absence is more common among males and at the L4 vertebrae. 103 In the cervical spine it is seen in decreasing prevalence at C6, C5, C4, and C7. Because aplasia interrupts the structural integrity of the posterior arch, spondylolisthesis may result from this defect. This is a classic finding at C6. The missing pedicle shadow is best seen radiographically, on the oblique projection, but is well demonstrated on the frontal radiograph. In adults, congenital agenesis often presents with an enlarged, radiodense contralateral pedicle, an appearance specific to the condition of aplasia. This is not typically the case among infants and children. If present, the enlarged radiodense contralateral pedicle may provide sufficient proof that the missing pedicle is associated with a congenital etiology as opposed to the more clinically relevant possibility of osteolytic bone disease. Metastasis or multiple myeloma (“winking owl” sign) should be of immediate concern in adult patients. Pathologic destruction of the pedicle by tumor, infection, or erosion seen with neurofibromatosis is not typically associated with hypertrophy or sclerosis of the opposite pedicle. If both pedicles are missing (“blind vertebra”), aggressive bone disease is clinically assumed until proved otherwise. Also, the vertebrae and lamina generally are not affected by developmental aplasia of the pedicle, where aggressive bone disease often has associated bone changes. Wilkinson syndrome describes a sclerotic pedicle with a contralateral pars defect. |
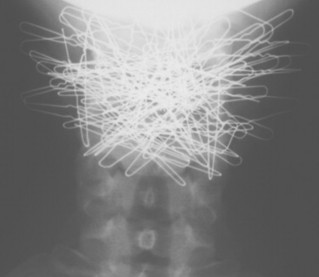
| Artifacts (Figs. 7-41 and 7-42) |
Miscellaneous radiodense foreign objects, surgical implantations, and other features may be present in the field of view. Some of these may include: central venous port, tantalum mesh/hernia repair, portal stents, Pepto-Bismol in the stomach, gastric bypass staples, umbilical rings, gall bladder surgery, renal surgery, abdominal aorta surgery, Greenfield-Kinney filter, and so forth. Overlying anatomy may also mimic the appearance of disease. |
| Baastrup phenomenon (kissing spines) (Figs. 7-43 and 7-44) |
Baastrup phenomenon, also known as kissing spines, refers to the approximation and resulting pseudoarthrosis of two or more spinous processes. It occurs secondary to intervertebral disc and posterior joint arthrosis but is also related to increased lumbar lordosis. The pseudoarthrosis is marked by a radiodense sclerotic zone subadjacent to the articulating portion of the spinous processes. In some patients it is postulated to be a source of regional pain. Although it is most common in the lumbar spine, a similar frictional sclerosis has been noted between the posterior tubercle of the atlas and the spinous process of C2. |
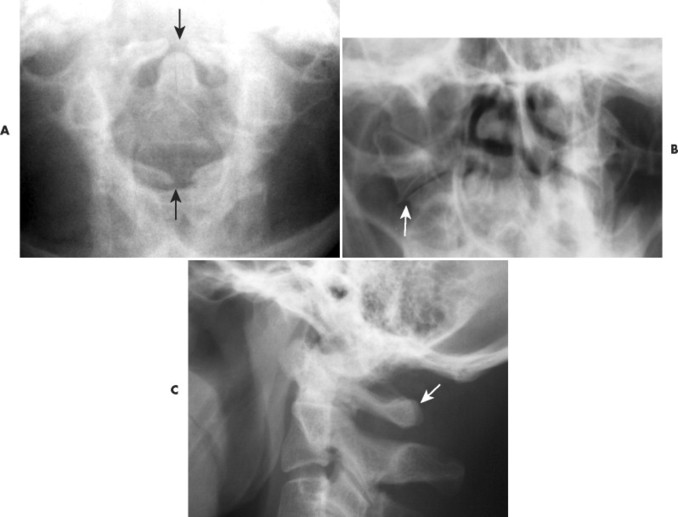
| Block vertebra (FIG. 7-45FIG. 7-46FIG. 7-47FIG. 7-48FIG. 7-49FIG. 7-50FIG. 7-51FIG. 7-52FIG. 7-53FIG. 7-54 and FIG. 7-55) |
Block vertebra describes a union between adjacent segments. It can be the result of congenital nonsegmentation of vertebral somites during the third to eighth fetal week of life or acquired causes such as infections and surgery. A congenital block vertebra can occur anywhere in the cervical, thoracic, or lumbar region, but is most common to the C2-3 and C5-6 levels. Although several contiguous segments may be involved, usually only two vertebrae are affected. The intervening intervertebral disc may be missing or rudimentary in both a vertical and horizontal dimension, the latter producing a narrowed waist at the junction of the fused segments. Very often the posterior arches of the segments are also fused and the corresponding intervertebral foramina appear prominent. |
| Butterfly vertebra (FIG. 7-56FIG. 7-57FIG. 7-58 and FIG. 7-59) |
This anomaly describes a persistent midline sagittal cleft of the vertebra body. When viewed from the frontal plane, the separated halves of the vertebra appear like the wings of a butterfly, or the full vertebra, like a sideways hourglass. It is common to note a slight triangular-shaped elevated area of bone that extends from the adjacent endplate of the normal segments above and below the butterfly defect that fits into the sagittal cleft of the anomalous segment. Disagreement exists over whether the configuration is an ossification defect of the right and left primary growth centers of the vertebral body, or results from a failure of notochordal regression. A butterfly vertebra is typically an isolated phenomenon and is of limited clinical significance. |
| Carotid calcification (Fig. 7-60) |
Calcification of the carotid vessel is often seen as an age-related phenomenon. However, vessel calcification does play a role in the development of atherosclerosis. Therefore, when present, a review of the patient’s history is advised to exclude clinical features of obstructive vessel disease. Severe calcification, especially in the area of the carotid siphon, correlates to vessel stenosis. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
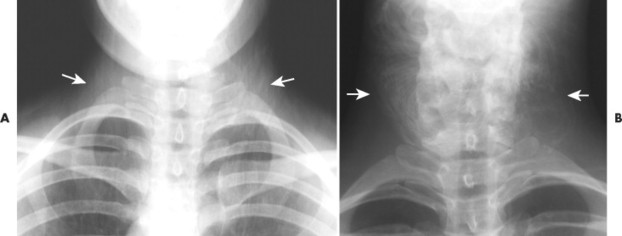
| Cervical ribs (Figs. 7-61 and 7-62) |
Cervical ribs are supernumerary ribs arising from cervical vertebrae. About 1% of the population demonstrates radiographic evidence of ribs from the cervical vertebrae. Cervical ribs usually are isolated to the C7 segment, bilateral about two thirds of the time, and are less commonly seen at more cephalic levels of the cervical spine. They may fuse to the first thoracic rib (osseously or by a fibrous band) or end freely. For reference, the T1 segment is identified as the first segment with transverse processes directed cephalically, in contrast to the lower cervical vertebrae, which exhibit a caudal direction of their transverse processes. Cervical ribs should not be confused with C7 transverse process hyperplasia; the latter does not exhibit a costotransverse joint. Transverse hyperplasia is defined as a transverse process that expends laterally to the distal tip of the T1 transverse process with no evidence of a costotransverse joint. Clinically, cervical ribs are significant because they may promote thoracic outlet syndrome by compressing the brachial plexus or the subclavian vessels at the thoracic outlet. Specifically, cervical ribs may narrow the space between the posterior margin of the first thoracic rib and anterior scalene muscle, through which the nerves and subclavian artery pass to the upper extremity. Thoracic outlet syndrome is marked by upper extremity claudication or neurologic symptoms, especially pain and paresthesia along the ulnar borders of the hands and forearm. The thenar eminence demonstrates muscle weakness and wasting in some patients. Symptoms may be exacerbated by turning the head to the ipsilateral side or raising the involved arm overhead. Additionally, symptoms are more likely with postural changes of drooping shoulders and increased thoracic kyphosis. Cervical ribs may have cartilaginous extensions that are not seen on radiographs, making it difficult to appreciate the true size of the rib on plain film studies. |
| Clasp-knife deformity (Figs. 7-63 and 7-64) |
Clasp-knife (or knife-clasp) deformity is the combination of a caudal elongation of the L5 spinous process and spina bifida occulta of S1. At times these individuals experience clinical symptoms (e.g., pain, bladder or bowel dysfunction) during lumbar extension, a presentation known as clasp-knife syndrome. |
| Cystic hygroma |
Cystic hygromas are nonmalignant malformations of lymph vessels occurring in the neck and (less commonly) head region. They are typically present during childhood, may be single or multiple, and may regress over time. They appear as a large mass or soft-tissue density in the anterior region of the neck. |
| Diastematomyelia (Fig. 7-65) |
This condition is marked by a fibrous, cartilaginous, or osseous bar, partially or completely extending across the vertebral canal. The bar may divide the cord, cauda equina, and meninges. It is most commonly found in the thoracolumbar region and is often accompanied by spina bifida occulta, hemivertebrae, and scoliosis. The impact of the bar on the neuroanatomy is best evaluated with magnetic resonance imaging. |
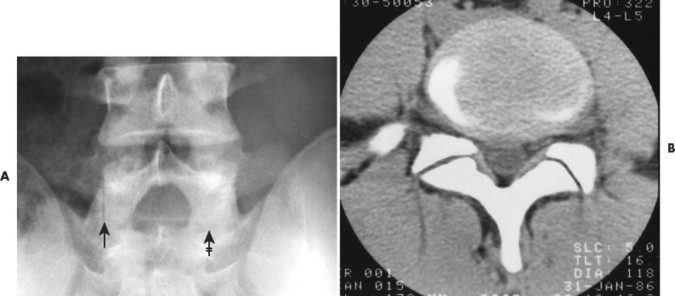
| Facet tropism (Figs. 7-66 and 7-67) |
The lumbar zygopopyphyseal joint planes are normally J-shaped, with the longest part of the joint oriented symmetrically in the sagittal plane. Facet tropism (Greek for “turn”) or facet asymmetry describes an asymmetric presentation of the joint planes, where one side is mostly in a sagittal plane and the contralateral side is mostly in a coronal plane. The clinical importance of this finding is debated in the related literature. Most studies trivialize facet joint asymmetry, although it may alter the application of chiropractic care given biomechanical concerns, as has been noted with upper cervical joint asymmetry. 92 The lumbar facet angle has been associated with disc degeneration and herniation. 24,35,77,109 However, other studies find no association with disc degeneration or disc herniation. 11,18,58,74,110 |
| Hahn’s fissures (clefts)/vascular grooves (Fig. 7-68) |
A single, thin, horizontal, radiolucent shadow traversing the middle of the vertebral body. It represents the channel for the segment’s vascular plexus. It is often visualized on radiographic projections of the thoracic and lumbar regions, typically presenting at multiple levels. Hahn’s fissures are common in young children, but the appearance may persist into adulthood. Vessels provide a similar appearance on the T2-weighted magnetic resonance scans, presenting as a small triangular focus of increased signal. |
|
|
|
|
|
|
|
|
|
|
| Hemivertebra (FIG. 7-69FIG. 7-70 and FIG. 7-71) |
The term hemivertebra describes a vertebra that is only half formed. These vertebrae usually appear in the thoracic region. Three varieties are noted based on the portion of the vertebral body that presents: lateral, dorsal, and ventral hemivertebrae. All hemivertebrae are trapezoidal or triangular in appearance in the frontal plane. They may be continuous with one or both of the adjacent segments (nonsegmented) or separated from the adjacent segments by an intervertebral disc (segmented). A singular lateral hemivertebra promotes a structural scoliosis with the lateral hemivertebra located at the apex of the curvature. Often lateral hemivertebrae are found in bilateral pairs, at differing spinal levels, forming a balanced S configuration of structural scoliosis that is usually only small in magnitude, because each compensates for the other. Dorsal hemivertebrae increase the thoracic kyphosis or decrease the lumbar lordosis. Ventral hemivertebrae create the opposite effect. The term scrambled spine has been applied to the presence of multiple levels of block vertebrae and hemivertebrae. |
| Hyoid fragmentation (Fig. 7-72) |
The hyoid may appear fragmented as a variant of normal. |
| Iliolumbar ligament calcification (Fig. 7-73) |
Calcification of the iliolumbar ligament appears as a radiodense band extending from the tip of the transverse process of the lowest lumbar vertebra laterally to the medial aspect of the iliac crest. It sometimes occurs with diffuse idiopathic skeletal hyperostosis (DISH), but more commonly is an isolated finding. Its relationship to clinical findings is ambiguous. |
| Intercalary ossicle (Figs. 7-74 and 7-75) |
A small ossicle is sometimes found in the anterior margin of the intervertebral disc space representing calcification of the anterior longitudinal ligament. It is metaplastic in origin and represents a normal variant of no clinical significance, or is found in association with degenerative disc disease of the corresponding disc segment. |
| Intervertebral disc calcification (FIG. 7-76FIG. 7-77 and FIG. 7-78) |
Intervertebral disc calcification occurs in the nucleus or, more commonly, the anulus fibrosus. It may appear linear, oval, or round. It is often seen in adults in association with degeneration, but idiopathic asymptomatic changes also can occur in children. A more lengthy discussion of intervertebral disc calcification is presented in Chapter 17. |
| Intervertebral disc hypoplasia |
Underdevelopment (or hypoplasia) of the intervertebral disc is seen in several congenital defects such as blocked segmentation and sacralization or lumbarization. When the L5 disc space is slightly decreased, care should be taken not to misinterpret the changes as degenerative. That is, a narrowed L5 disc space, without features of degeneration (e.g., osteophytes, vacuum phenomena) should be interpreted as disc hypoplasia, assuming that infection and other causes can be excluded. Disc hypoplasia is a common cause of a narrow disc space at the L5 level in a younger patient who is not likely to exhibit degeneration. |
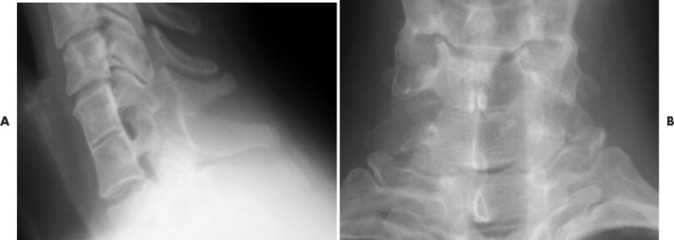
| Klippel-Feil syndrome (Figs. 7-79 and 7-80) |
Klippel-Feil syndrome is a rare condition marked by one or multiple levels of blocked segmentation. Approximately half the patients with multiple blocked segments demonstrate a clinical triad of low hairline, limited range of motion, and a short webbed neck. (See Chapter 8 for a complete discussion of Klippel-Feil syndrome.) |
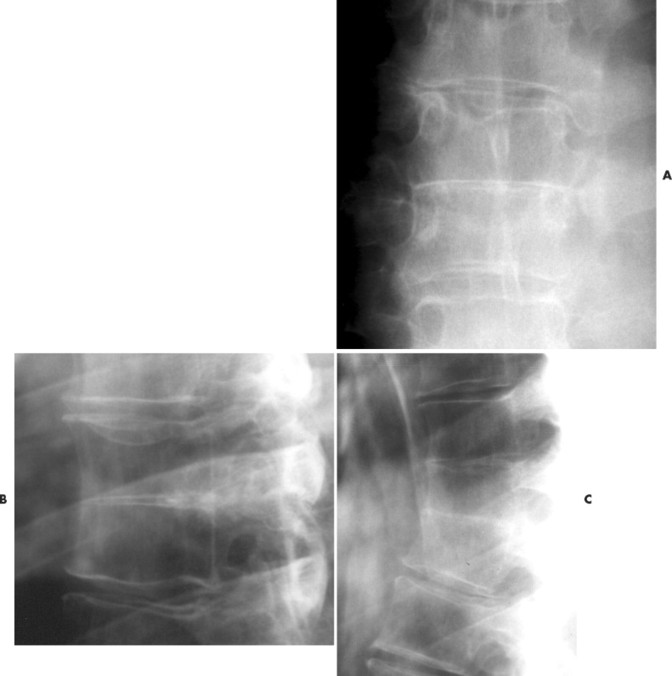
| Limbus bone (FIG. 7-81FIG. 7-82FIG. 7-83FIG. 7-84 and FIG. 7-85) |
A limbus bone is a small (<1 cm), permanently separated portion of the vertebra’s ring epiphysis that occurs secondary to a peripheral intravertebral herniation of disc material They are usually noted at the anterior-superior margin of a middle lumbar segment and are of little to no clinical significance. Limbus bones are caused by peripheral intravertebral disc herniations; by contrast, Schmorl’s nodes are caused by central intravertebral disc herniations. Limbus bones are distinguished from a teardrop fracture by their usual presence of smooth, well-corticated margins, close proximity to the segment, and lumbar location (teardrop fractures are more common to the cervical spine). Intercalary bones are typically in the cervical spine and do not have a defect in the adjacent vertebra, differentiating them from limbus bones. |
| Lymph node calcification (Fig. 7-86) |
Calcification of the lymph nodes is a common result of granulomatous diseases (e.g., tuberculosis or histoplasmosis). They usually appear mottled, but at times outer “eggshell” calcification is noted, a feature suggesting pneumoconiosis, treated lymphoma, and sarcoidosis as the etiology when presenting in the pulmonary tissue. Lymph node calcification often appears in the paraspinal soft tissues of the cervical spine. |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
| Myelogram remnant |
Some of the radiodense contrast may remain in the thecal sac following a myelographic procedure. The older oil-based residual contrast resorbs at approximately 5 ml/year until completely removed. The more contemporary water-based products resorb more quickly. Radiographically the contrast appears as multiple radiodense droplets in the lumbar dural sac. |
| Nuchal bone (Fig. 7-87) |
A nuchal bone is a focal ossification of the nuchal ligament appearing as an oblong, vertically oriented, radiodense osseous structure that varies in size, but is often approximately 1 cm wide and 2 to 4 cm long. It is commonly seen among patients more than 40 years of age and is of limited clinical significance. A nuchal bone is sometimes confused with an ununited secondary growth center of the spinous process, which is typically smaller and has an associated defect of the spinous process, or a Clay shoveler’s fracture, which usually is adjacent to a spinous fracture with ragged margins, is inferiorly displaced, and is accompanied by a history of trauma. |
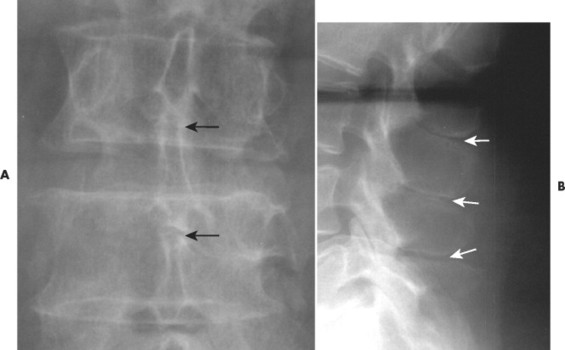
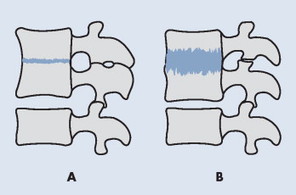
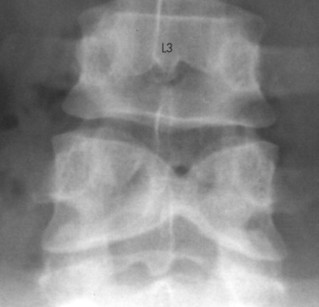
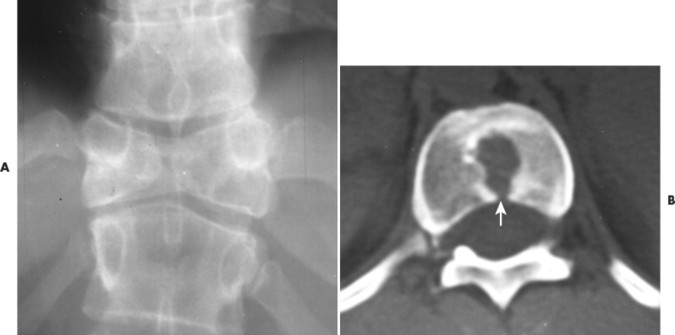
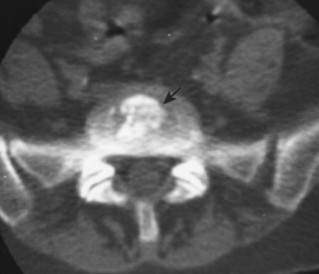
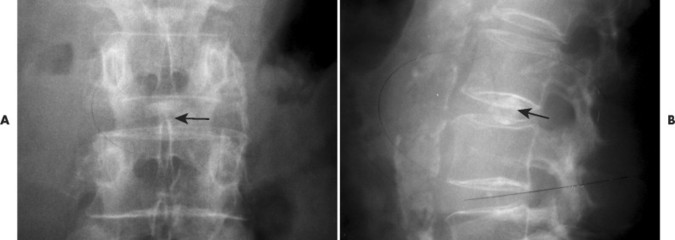
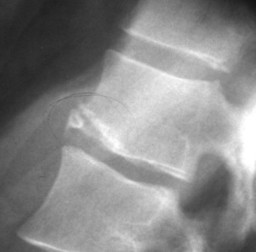
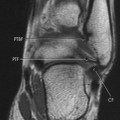
| Nuclear impression (FIG. 7-88FIG. 7-89 and FIG. 7-90) |
Nuclear impression, also known as notochordal persistence, is marked by subtle, gradual inward defects of the endplates that tend to involve most of the endplate. They appear as a concave deformity in a lateral radiographic projection. They may appear as two inward defects, creating a double hump appearance known as cupid’s bow in a frontal radiographic projection. The two inward defects appear as radiolucent disc material on axial computed tomography scans, known as an owl sign
Only gold members can continue reading. Log In or Register to continue
|