Diagnosis: Posterior elbow dislocation
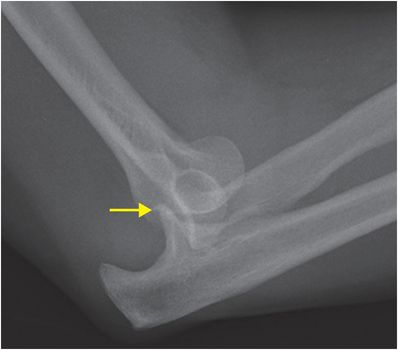
Lateral radiograph demonstrates a posterior elbow dislocation, with the distal humerus positioned anterior to the coronoid process and ulna dislocating posteriorly. There is cortical irregularity of the coronoid process (arrow), suspicious for fracture.
Discussion
Overview of elbow dislocation
Elbow dislocation is defined by the relative position of the proximal ulna and radius relative to the distal humerus. Posterior dislocations are more common and typically occur after a fall onto outstretched hand (FOOSH). The specific mechanism of injury most commonly involves a combination of axial compression, supination, and valgus stress.
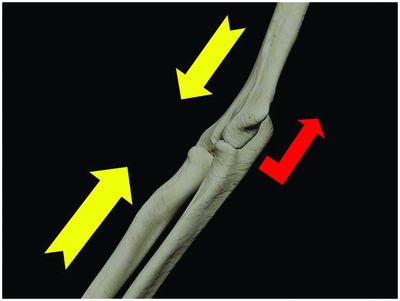
Fall onto outstretched hand with the arm in slight supination and valgus angulation at the elbow produces axial compression forces at the elbow (yellow arrows), which can cause posterior dislocation of the ulna relative to the humerus (red arrow).
Classification of elbow dislocation
Simple: no associated fractures.
Complex: associated fractures, such as radial head and coronoid process fractures (the terrible triad is the combination of posterior dislocation with both of these fractures). Additional fractures of the capitellum or olecranon may be seen.
Posterolateral rotatory instability (PLRI) is a progression of (predominantly) lateral ligamentous injuries caused by external rotation and posterior subluxation of the ulna with respect to the distal humerus. The most severe form of PLRI is a frank posterior dislocation, in which case there is also medial ligamentous injury. PLRI can clinically present with painful clicking, snapping, or locking, often associated with the subjective feeling of apprehension with activities such as pushing to rise from a chair. PLRI is thought to occur in a progressive sequence:
1. Stage 1: lateral ulnar collateral ligament (LUCL, an important lateral stabilizer that connects the lateral epicondyle of the humerus to the ulna) injury only.
2. Stage 2: radial collateral ligament (RCL, a secondary radial/lateral stabilizer that connects the lateral epicondyle to the annular ligament) and LUCL injury. Stage 2 PLRI presents as near-complete dislocation with perching of the humerus on the coronoid process.
3. Stage 3: anterior bundle of the medial collateral ligament (the most important medial/ulnar stabilizer that connects the medial epicondyle to the sublime tubercle of the proximal ulna) injury, in addition to LUCL and RCL injury. Once the medial-sided ligaments are injured, it is possible to have a dislocation even without a fracture.

Posterolateral elbow instability can be described in stages ranging from mild instability (I) to perching of the humerus on the coronoid process (II) to frank dislocation (III).
Associated injuries
“Terrible triad”: the previously discussed “terrible triad” is a posterior dislocation with associated radial head and coronoid process fractures. Surgery is almost always indicated for best management. Note that a posterior dislocation that has spontaneously reduced may be radiographically occult if there is no associated fracture. Posterior dislocations should be suspected if a coronoid process fracture is detected.
Coronoid process fracture: CT can be used to better characterize coronoid process fracture morphology. Fractures of the anteromedial facet of the coronoid process and sublime tubercle of the proximal ulna can predispose to posteromedial rotary instability (PMRI) since the sublime tubercle serves the attachment site of the anterior band of medial collateral ligament, a primary radial/medial-sided stabilizer of the elbow. Note that PMRI is always associated with a coronoid process fracture and is due to varus stress.

Coronal CT reformation in another patient showing a comminuted intra-articular fracture of the proximal ulna involving the ulnohumeral articulation and the sublime tubercle (arrow).
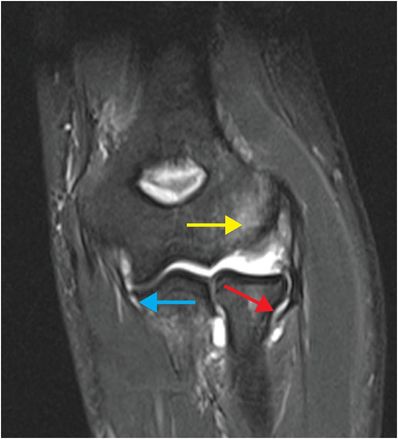
Coronal STIR MR in a different patient shows marrow edema in the capitellum / lateral epicondyle (yellow arrow) and apposing radial head following recent elbow dislocation. There is a full-thickness tear of the LUCL (red arrow). There is a partial-thickness tear of the deep surface of the medial collateral ligament (MCL), manifest by fluid interposed between the MCL and the sublime tubercle, also known as the “T-sign” (blue arrow). The RCL (not visualized on this image) was also injured, consistent with stage 3 PRLRI.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








