Figure 8.2 The coalescence of many of the patchy areas of infiltrate are seen throughout both lung fields, which eventually will create a more homogenous and extensive infiltrate.
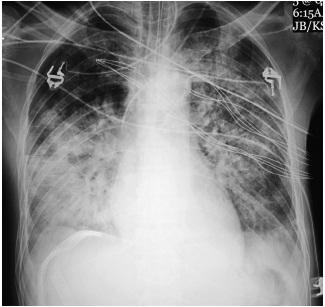
Figure 8.3 Extensive bilateral coalescent densities that have progressed over several days; note the classic air bronchograms.

Air bronchograms are commonly identified because the exudative process is very thick and involves the alveoli and the interstitium, but the fluid does not usually extend into the bronchi, which remain patent.
The findings may not change for days, possibly weeks, which is in sharp contrast to alveolar opacities secondary to cardiogenic edema or even pneumonia, which change more rapidly.122
Much remains to be understood about ARDS. One can consider it an imbalance between injury and repair, and the actual changes are quite complex. The specific site of injury is the alveolar capillary membrane, whose endothelium becomes permeable, permitting transcapillary migration of proteinaceous fluid and inflammatory cells into the alveoli as well as the interstitium. The alveolar basement membrane sluffs, as part of the repair process, and a hyaline membrane forms, secondary to the migration of the protein-rich edema fluid. The type II pneumocyte has been denuded and gas exchange is impaired. The patient becomes markedly hypoxic, cyanotic, and dyspneic Oxygen saturation falls, necessitating increased levels of PEEP, to, it is hoped, recruit and open other alveoli (Fig. 8.4). The danger is that overdistention of normally air-filled alveoli results in secondary barotraumas, complicating the patient’s ARDS.123
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree