
Diagnosis: Hematoma secondary to a bleeding renal angiomyolipoma
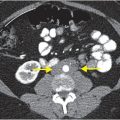
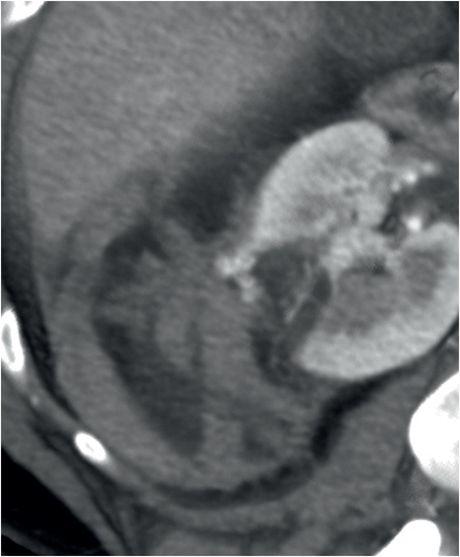
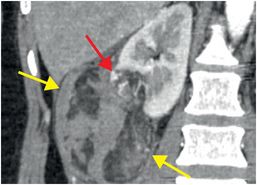
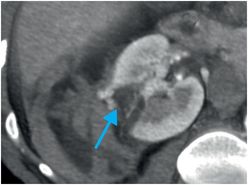
Coronal (left image), axial (middle image), and sagittal (right image) contrast-enhanced CT images demonstrate retroperitoneal hemorrhage surrounding an exophytic, fat-containing, hypervascular right renal mass (yellow arrows). Prominent intratumoral vessels are noted within the lesion (red arrows). Despite predominantly exophytic location, the lesion definitively arises from the renal cortex in the posterior interpolar region, as indicated by the cortical defect (blue arrow).

Discussion
Angiomyolipoma and risk of hemorrhage
As the name implies, angiomyolipoma (AML) is a benign renal tumor comprised of vascular, smooth muscle, and fatty elements.
Isolated or sporadic AMLs account for the vast majority of cases, in which tumors are typically unilateral and occur in middle-aged women. Up to 80% of patients with tuberous sclerosis have multiple, bilateral AMLs.
Although they are usually an incidental finding, AMLs may present in the acute setting with hemorrhage, especially if they grow larger than 4 cm. It is thought that abnormal intratumoral vessels are prone to microaneurysm formation and, hence, hemorrhage.
Clinical presentation of a bleeding AML includes hypotension, decreasing hematocrit, flank pain, and/or hematuria.
Imaging of AML
The diagnosis of AML relies on identification of intratumoral macroscopic (gross) fat, which is characterized by negative density on CT (typically <-20 HU), or intratumoral fat signal (saturation on fat-suppressed images) on MRI. Overwhelmingly, AML is a diagnosis made by radiologists.
Imaging diagnosis may be difficult in lipid-poor AMLs (4% of all AMLs). The finding of a small, hyperdense renal mass on CT should raise the suspicion of lipid-poor AML, particularly in a young female patient. Biopsy can be used to make the diagnosis and avoid unnecessary surgery.
On MR imaging, an AML is seen as a mass that contains focal macroscopic fat signal. Intra-lesional fat signal will follow retroperitoneal or mesenteric fat on all pulse sequences, with the fat-suppressed sequences most helpful. Note that in- and out-of-phase imaging, which is used to evaluate for the presence of water and fat in the same voxel, is not helpful to detect macroscopic fat.
In extremely rare instances, renal cell carcinomas (RCCs) can contain macroscopic intratumoral fat, which may be secondary to lipid-producing necrosis within a large RCC, intratumoral bone metaplasia with fatty marrow elements (usually associated with calcification), or entrapment of perirenal or sinus fat. Unlike a rare fat-containing RCC, AML should not have any calcification.
Clinical synopsis
This patient was admitted and treated with aggressive fluid resuscitation. After CT diagnosis, she was referred to interventional radiology, where she had an uneventful endovascular embolization. Following the procedure she was asymptomatic and hemodynamically stable, and she was discharged the following day.
Self-assessment
|
|
|
|
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree